
Medical Imaging Blog
Diagnostic medical imaging technologies are evolving rapidly, with blog articles covering MRI, CT, ultrasound, PET, SPECT, AI, and radiopharmaceutical advancements.
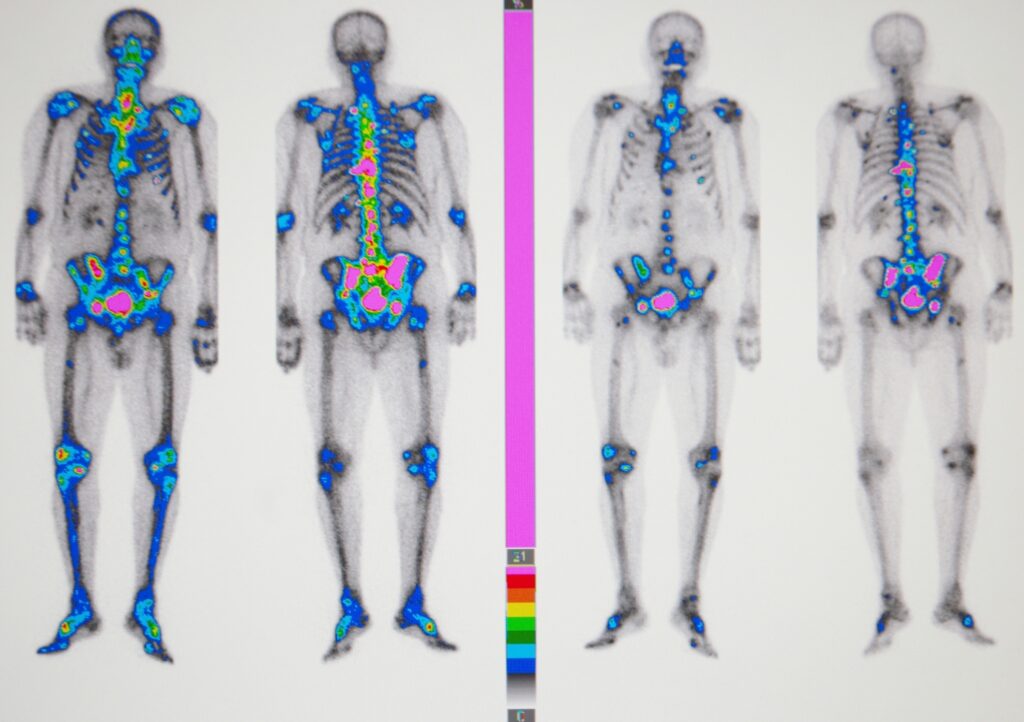
Nuclear Medicine
Nuclear medicine utilises PET and SPECT scanners with radiolabelled imaging agents to generate functional images for precise diagnostics.

Radiotheranostics
Radiotheranostics merges diagnosis and therapy, using radiolabelled compounds for precise imaging and targeted cancer treatment.

Cyber Security
Cyber security protects patient data, ensures service integrity, and requires strong measures to counter growing threats.

Medical Imaging News
Imaging News covers medical imaging advances, including AI and portable devices, improving diagnostics and accessibility. Image for illustration only. Person depicted is a model.

Radiopharmacy
Radiopharmaceuticals enhance imaging and therapy using radioactive isotopes such as technetium-99m and fluorine-18 for cancer care.
Radiotherapeutics
Medical radiotherapeutics use radionuclides such as actinium-225 for precise cancer treatment, minimising damage and personalising therapy.
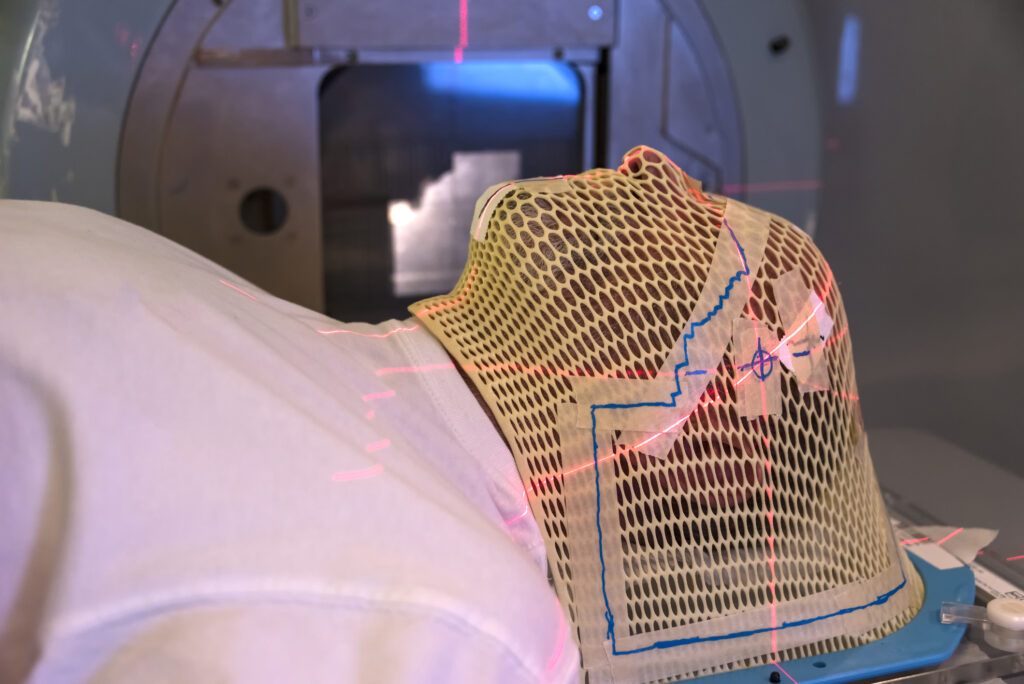
Radiation Therapy
Medical radiation therapy treats cancer using IMRT, IMAT, and SRT, targeting tumours while preserving healthy tissue. Image for illustration only. Person depicted is a model.

Medical Physics
Medical Health Physics ensures safe radiation use in healthcare, protecting patients, workers, and the public effectively.

Radiology
Medical radiology uses imaging for example X-ray, ultrasound, and CT for diagnosis, treatment, and minimally invasive procedures. Image for illustration only. Person depicted is a model.
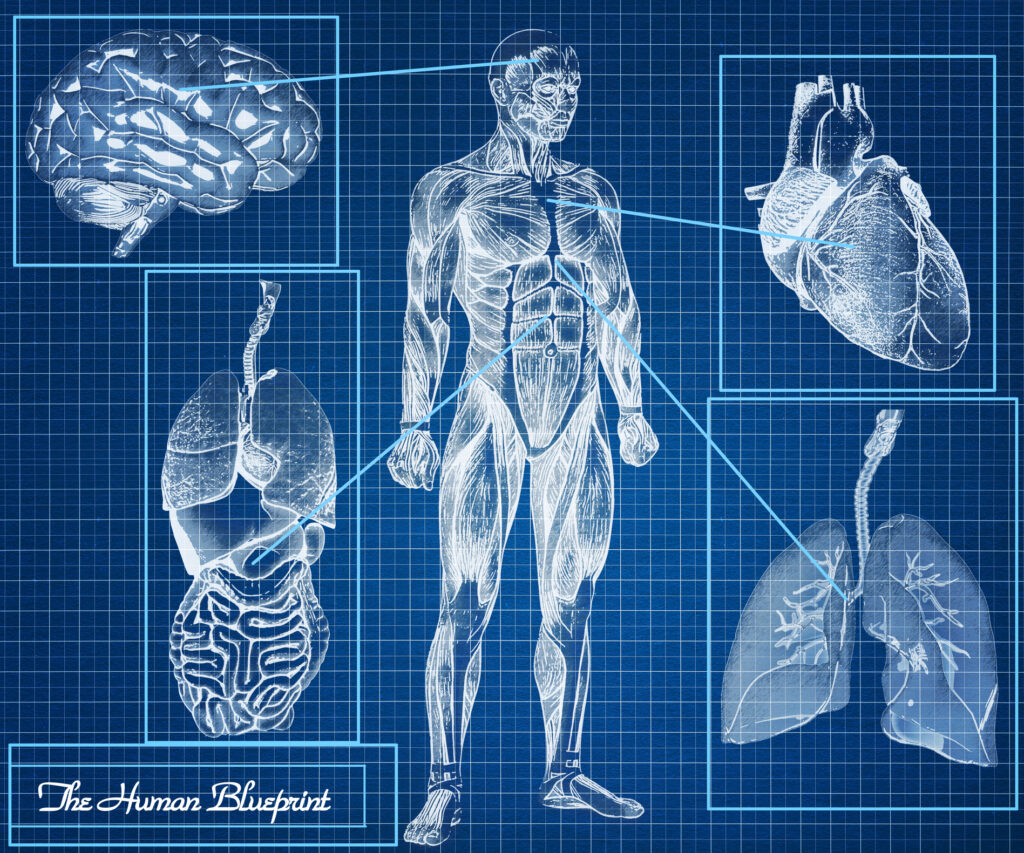
Human Anatomy
Medical human anatomy studies body structures through dissection, including gross anatomy, histology, embryology, and neuroanatomy.

Medical Devices
Medical devices, from thermometers to MRI, vary by risk, with innovations such as AI improving patient care.
Editorial Reviews
Open MedScience reviews medical imaging, therapy, and radiotheranostics, offering critical analyses to improve medical research quality.

Education
Radiography and medical technology training develops imaging skills, preparing students for essential roles in healthcare diagnostics.Image for illustration only. People depicted are models.
Medical Imaging Topics
Medical imaging uses X-rays, MRI, and CT scans to diagnose and treat conditions by visualising structures.
Journal
The Journal of Diagnostic Imaging in Therapy publishes research on imaging techniques, promoting healthcare advancements and collaboration.
Radiopharmaceuticals
Medical radiopharmaceuticals use SPECT, PET, and gamma cameras for diagnosis and treatment, requiring safety and regulatory approval.

Optical Imaging
Medical optical imaging uses light-based techniques for diagnostics and treatment, providing precise insights into body structures.

Regulatory Affairs
Regulatory affairs ensures pharmaceuticals, medical devices, and biologics meet safety standards for market approval.

Medical Science Liaison
Medical Science Liaison fosters relationships, shares clinical data, and supports safe, effective medication use in healthcare. Image for illustration only. People depicted are models.

Medicine
Medicine diagnoses, treats, and prevents diseases, combining various fields to improve health using medications, surgeries, and therapies.

Nutraceuticals
Nutraceuticals are food-derived products with health benefits, combining nutrients and pharmaceuticals in functional foods and supplements.

Health & Wellbeing
Health and wellbeing encompass physical, mental, and social wellness, promoting a balanced lifestyle and disease prevention.

Sustainability
Sustainability in medical imaging reduces environmental impact by optimising energy, minimising waste, and adopting eco-friendly technologies.

Health Matters
Health matters link social factors, policy, and wellbeing, using interventions and prevention to improve community resilience.

Artificial Intelligence
AI advancements enhance diagnostic imaging, enabling radiologists to analyse large data sets from modern equipment.

Medical Technologies
Advancing medical technologies improve diagnostics, treatment, and care, with AI, imaging, and robotics enhancing precision. Image for illustration only. Person depicted is a model.
