Summary: Diagnostic imaging plays a central role in modern medicine, providing vital insights into anatomy and physiology for accurate diagnosis and effective treatment. This article explores the evolving field of diagnostic imaging physics, focusing on how advances in X-ray, CT, MRI, ultrasound, nuclear medicine imaging, hybrid imaging, image reconstruction, and image analysis are being used to improve clinical outcomes. By optimising imaging protocols, enhancing image quality, and managing radiation exposure, medical physicists and clinicians are achieving better diagnostic accuracy while maintaining patient safety. Emphasis is also placed on developing advanced techniques and algorithms that underpin high-resolution imaging and quantitative analysis.
Keywords: Diagnostic Imaging, MRI, CT, Ultrasound, PET/CT, Image Analysis
The Role of Imaging Physics in Modern Healthcare
Medical imaging technologies have transformed diagnostic and therapeutic capabilities across nearly all clinical specialties. The discipline of diagnostic imaging physics ensures these technologies are used effectively, safely, and innovatively. It plays a crucial role in shaping how imaging is performed, with direct implications for patient care and treatment. From fine-tuning protocols to developing new reconstruction algorithms, imaging physicists help to maximise diagnostic yield while minimising risks such as unnecessary radiation exposure.
X-ray and CT Imaging: Balancing Dose and Diagnostic Yield
X-ray and computed tomography (CT) imaging remain the workhorses of diagnostic radiology. They provide rapid and detailed anatomical information, particularly valuable in emergency and oncological settings. However, both modalities involve ionising radiation, which carries inherent risk.
Optimising imaging protocols involves fine-tuning parameters such as tube voltage, current, exposure time, and slice thickness. Techniques like automatic exposure control (AEC) and iterative reconstruction algorithms enable personalised radiation dose while maintaining or enhancing image quality. In paediatric imaging, dose reduction strategies are particularly important due to the increased radiation sensitivity of children.
Advanced detector technologies and dual-energy CT (DECT) now offer improved tissue characterisation and contrast resolution without requiring higher doses. Protocol standardisation and regular quality control are also essential in ensuring consistent image quality across different scanners and institutions.
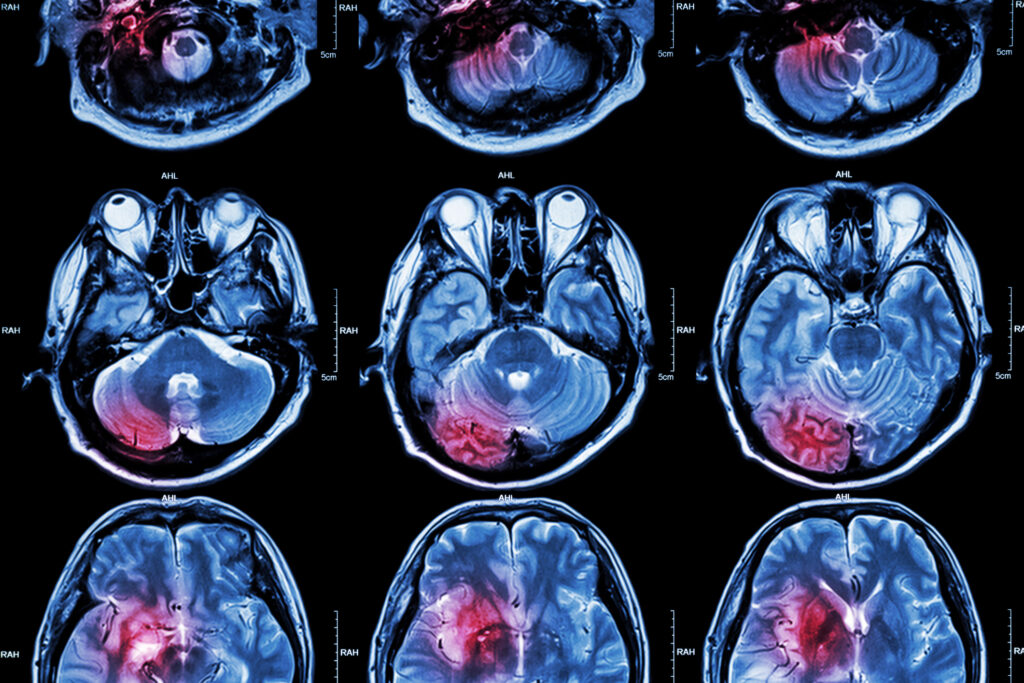
MRI: Advancing Contrast, Resolution, and Speed
Magnetic Resonance Imaging (MRI) offers unmatched soft-tissue contrast without ionising radiation, making it particularly valuable in neurological, musculoskeletal, and oncological imaging. However, image acquisition times are traditionally longer compared to CT, and motion sensitivity can affect quality.
Significant progress is being made in the development and application of advanced MRI techniques, including diffusion-weighted imaging (DWI), functional MRI (fMRI), and magnetic resonance spectroscopy (MRS). These methods provide functional and biochemical information in addition to structural imaging.
Parallel imaging, compressed sensing, and deep learning-based reconstruction algorithms have considerably reduced scan times while improving resolution. Techniques such as T1 and T2 mapping are being used for quantitative tissue characterisation, particularly in cardiology and liver imaging.
Optimising coil configurations and pulse sequences also play a key role in balancing signal-to-noise ratio (SNR), spatial resolution, and scanning time. Standardisation efforts, especially in multicenter studies, are crucial for ensuring the reproducibility and comparability of advanced MRI data.
Ultrasound: From Imaging to Intervention
Ultrasound is a versatile, real-time, and non-ionising imaging modality widely used in obstetrics, cardiology, and point-of-care settings. Its portability and safety profile make it ideal for bedside assessments. However, image quality is highly operator-dependent, and artefacts can interfere with interpretation.
Recent advances in ultrasound imaging include contrast-enhanced ultrasound (CEUS), elastography, and three-dimensional (3D) and four-dimensional (4D) imaging. CEUS enables improved visualisation of vascularity and tissue perfusion, while elastography provides insights into tissue stiffness, useful in liver fibrosis and thyroid assessments.
Ultrasound-guided therapeutic procedures, such as high-intensity focused ultrasound (HIFU) and ultrasound-mediated drug delivery, are expanding the modality’s utility beyond diagnostics.
Efforts to optimise ultrasound imaging involve improving transducer technology, refining beamforming techniques, and applying adaptive imaging algorithms. Machine learning is increasingly used to automate image acquisition and interpretation, thereby reducing variability and enhancing reproducibility.
Nuclear Medicine Imaging: Enhancing Functional Imaging with PET and SPECT
Nuclear medicine techniques such as Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) provide molecular-level insights into physiological processes, often before anatomical changes become visible.
Optimisation in PET and SPECT focuses on radiotracer selection, image acquisition protocols, and correction methods for attenuation, scatter, and motion. Advances in time-of-flight (TOF) PET and digital detectors have led to improved spatial resolution and sensitivity.
Efficient dose management is achieved through the use of short half-life radionuclides and optimised administered activity. Additionally, patient preparation protocols are being refined to minimise artefacts and maximise image quality.
The integration of artificial intelligence (AI) is facilitating improved quantification and lesion detection, particularly in oncology and neurology. Quantitative imaging biomarkers derived from PET and SPECT are increasingly utilised in assessing therapy response and monitoring disease progression.
Hybrid Imaging: The Power of Combined Modalities
Hybrid imaging systems, such as PET/CT, SPECT/CT, and PET/MRI, offer the unique advantage of combining anatomical and functional data in a single examination. This synergy enables improved localisation and characterisation of lesions, thereby enhancing diagnostic confidence.
Optimisation of hybrid imaging requires careful alignment of protocols across modalities to ensure spatial accuracy and consistency in image quality. Attenuation correction, often derived from CT or MRI data, plays a critical role in ensuring accurate quantification in PET and SPECT images.
PET/MRI, although less widely available than PET/CT, presents specific challenges due to the technical complexity of integrating the two systems. However, it offers lower radiation dose and superior soft-tissue contrast, making it valuable in paediatric oncology and neuroimaging.
Hybrid imaging is also playing an increasingly important role in therapy planning, particularly in radiotherapy and interventional procedures where precise targeting is essential.
Image Reconstruction: From Raw Data to Clinical Insight
Image reconstruction algorithms transform raw signals into clinically useful images. They are central to all imaging modalities and significantly influence image quality, resolution, and noise characteristics.
Traditional filtered back projection (FBP) methods have been largely replaced or supplemented by iterative reconstruction (IR) techniques, particularly in CT and nuclear medicine. These algorithms model the physics of data acquisition and system geometry to produce images with higher fidelity.
In MRI, reconstruction methods such as compressed sensing and parallel imaging are crucial for accelerating scans while maintaining resolution. Deep learning approaches are also making inroads, offering fast reconstruction with improved image quality and reduced artefacts.
Adaptive and model-based reconstruction techniques are being developed to account for patient-specific anatomy and motion, particularly in cardiac and abdominal imaging. These innovations contribute to personalised imaging strategies that improve diagnostic confidence.
Image Analysis: Quantifying the Invisible
Beyond visual assessment, quantitative image analysis enables the objective evaluation of imaging data, which is essential for monitoring disease progression and treatment response. Techniques such as segmentation, texture analysis, and radiomics are being increasingly utilised in clinical and research settings.
Image processing algorithms can extract metrics like volume, density, perfusion, and elasticity, which serve as biomarkers for disease characterisation. In oncology, radiomics is being explored as a non-invasive method to predict tumour aggressiveness and treatment outcomes.
AI and machine learning are transforming image analysis by enabling automated detection, classification, and tracking of abnormalities. These tools not only improve workflow efficiency but also reduce inter-observer variability.
Standardisation and validation of image analysis pipelines are necessary for clinical adoption. Regulatory and ethical considerations, particularly concerning the use of AI in diagnostics, are also gaining attention.
Engineering Precision for Better Outcomes
Diagnostic imaging physics sits at the intersection of clinical medicine, engineering, and data science. As imaging modalities become more advanced, the demand for precise, personalised, and efficient imaging grows. Optimising protocols, improving image quality, managing doses, and implementing sophisticated image processing methods are essential for modern diagnostics.
The future of diagnostic imaging lies in the integration of multimodal data, real-time image analysis, and AI-assisted decision-making. These developments have the potential to transform patient care by making diagnostics more accurate, accessible, and responsive to individual needs.
The continued collaboration between clinicians, physicists, and technologists will be key to realising these advancements, ensuring that the science of imaging translates into meaningful health outcomes.
Disclaimer
The content of this article is intended for informational and educational purposes only. Open Medscience does not provide medical, diagnostic, or therapeutic advice. All medical imaging techniques and technologies discussed should be interpreted and applied by qualified healthcare professionals in accordance with clinical guidelines and local regulations.
While efforts have been made to ensure the accuracy and currency of the information presented, no guarantee is given regarding its completeness or suitability for any particular use. Readers should not rely solely on this article when making decisions related to patient care or medical imaging practices.
Open Medscience, its authors, and affiliates accept no responsibility for any loss, injury, or damage resulting from the use or misuse of the information contained herein. The inclusion of specific technologies, software, or equipment does not imply endorsement or recommendation.
Always consult with appropriate specialists or regulatory authorities before implementing or modifying any diagnostic imaging protocols.
You are here: home » diagnostic medical imaging blog »