The search for reliable, human-relevant alternatives to traditional animal testing and static cell culture has accelerated in recent years. Among the most promising advances is the emergence of organ-on-a-chip (OoC) technology — miniature systems that simulate the function of living human tissues and organs in dynamic micro-engineered environments.
By combining cell biology, microfluidics and materials science, these chips recreate aspects of the body’s physiology, such as fluid flow, mechanical stress, and biochemical communication between different cell types. In doing so, they bridge the long-standing gap between two-dimensional cell cultures and whole-organism studies.
As the technology matures, the field has shifted from proof-of-concept demonstrations to scalable platforms ready for industrial and regulatory use. The latest developments reveal not only technical ingenuity but also a genuine step toward transforming preclinical research and personalised medicine.
Moving from Prototype to High-Throughput Systems
A major turning point has been the move towards scalable, high-throughput OoC systems. For years, early prototypes were handcrafted in research laboratories — each one tailored to a specific experiment and often requiring expert microfluidic handling. This made them ill-suited for large-scale screening or pharmaceutical workflows.
That situation is changing. At the 2025 Microphysiological Systems (MPS) World Summit, Emulate, Inc. presented its AVA Emulation System, capable of running up to 96 independent organ-chip experiments simultaneously. The platform integrates automated imaging, environmental control and data capture, allowing researchers to perform repeatable, parallel assays rather than single, bespoke experiments.
This type of automation signals a new phase for the field. High-throughput capability means that organ-on-a-chip devices are now realistic candidates for routine drug-screening pipelines, toxicity studies, and mechanism-of-action research within pharmaceutical companies.
The shift also encourages consistency and data standardisation — both essential for regulatory acceptance. When multiple laboratories can use the same platform under identical conditions, the results become more comparable and easier to interpret across studies.
Progress Towards Regulatory and Ethical Acceptance
Another striking development is the increasing interest from regulatory agencies. Governments and scientific bodies worldwide are exploring alternatives to animal models, which often fail to predict human responses accurately and raise ethical concerns.
In the United States, the Food and Drug Administration (FDA) has expressed formal support for the integration of non-animal approaches, including OoC systems, into safety testing. Meanwhile, in Europe, the Joint Research Centre (JRC) of the European Commission has published a roadmap for the standardisation and validation of OoC technology. This roadmap aims to create agreed-upon benchmarks, performance criteria and terminology to support international harmonisation.
The growing policy momentum is matched by investment from funding agencies and private industry. Initiatives such as the UK’s National Centre for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs) are providing grants for projects that employ OoC models to reduce reliance on animal testing.
The broader ethical and scientific case is clear: by accurately reproducing human tissue function in vitro, OoC systems offer a faster, safer and more humane route to understanding drug efficacy and toxicity before entering clinical trials.
Combining Organoids with Organ-on-a-Chip Platforms
One of the most significant technical trends is the merging of organoid technology with microfluidic OoC systems. Organoids are three-dimensional cell cultures derived from stem cells that self-organise into miniaturised, simplified versions of organs. They possess structural and functional characteristics that two-dimensional cultures lack, but are typically static and lack physiological flow or mechanical stimulation.
By placing organoids within the controlled microenvironment of an organ-on-a-chip, researchers gain the best of both worlds — the structural complexity of organoids and the dynamic, fluidic control of microengineered systems. These organoids-on-a-chip enable continuous nutrient supply and waste removal, the application of mechanical forces (such as breathing motions or heartbeats), and the measurement of tissue-level responses over time.
This hybrid approach is proving especially useful in modelling complex diseases. Liver-on-a-chip and gut-on-a-chip systems, for instance, can now include multiple cell types and microvascular structures, enabling studies of inflammation, drug metabolism, and host–microbiome interactions. Similarly, brain-on-a-chip models incorporating neural organoids are opening new possibilities for neurodegenerative disease research and drug discovery.
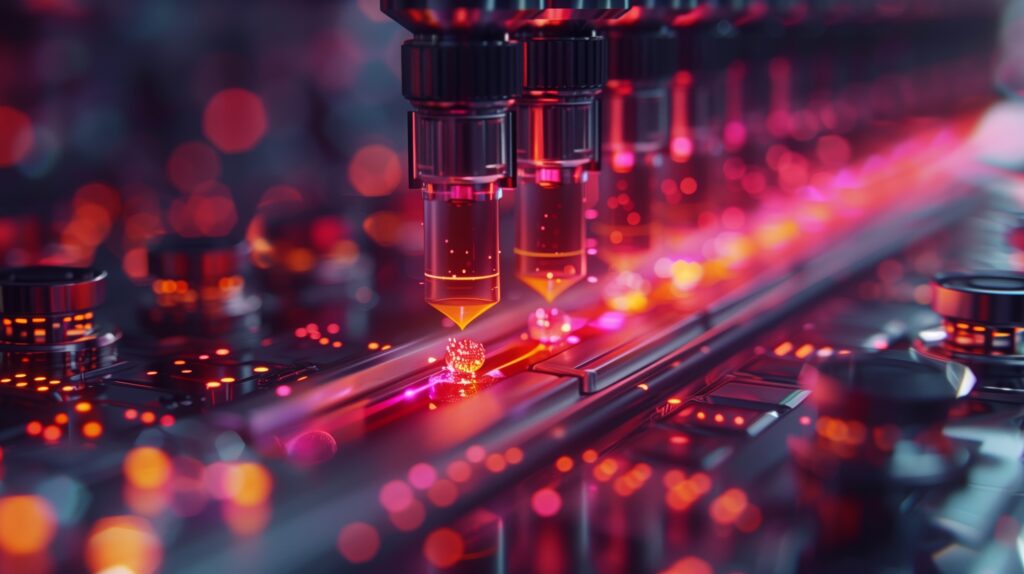
Enhanced Sensing and Real-Time Monitoring
Another area of progress lies in integrating embedded sensors and analytical tools into OoC devices. Traditional cell culture techniques often rely on endpoint assays — snapshots of biological activity taken at specific time points. By contrast, chips with built-in biosensors can continuously monitor cellular behaviour in real time.
Recent designs include electrical impedance sensors for measuring barrier integrity, optical sensors for tracking oxygen levels, and biochemical sensors for detecting metabolites such as glucose or lactate. Combining these signals provides a richer dataset that mirrors how tissues respond dynamically to changing conditions or treatments.
For imaging-focused researchers, this convergence of sensor technology and microfluidics is particularly exciting. It enables the use of advanced optical microscopy, fluorescence and even miniature magnetic resonance setups to visualise processes such as perfusion, diffusion, and tissue deformation inside the chip. In the longer term, these readouts may directly correlate with non-invasive clinical imaging biomarkers, providing a new bridge between preclinical and clinical data.
Expanding Market and Commercialisation
As performance and reliability improve, the OoC sector is experiencing rapid commercial growth. Market analyses predict that the global organ-on-a-chip market will increase from approximately US $150 million in 2024 to more than US $650 million by 2029, representing an annual growth rate of over 30 %. Some forecasts extend this to nearly US $1 billion by 2035.
This surge reflects both rising demand and a proliferation of new suppliers. In addition to Emulate, companies such as Mimetas, CN Bio, TissUse, Alveolix and InSphero are producing a variety of modular chips tailored for liver, kidney, lung, gut, heart and skin applications. Many offer plug-and-play systems compatible with standard laboratory equipment and data-management software, making them attractive to pharmaceutical companies and contract research organisations.
Universities and start-ups are also collaborating more closely with industry to translate prototypes into commercial products. Partnerships between engineering groups, biologists and clinicians are ensuring that new chips not only mimic biology more accurately but also meet the practical demands of research and regulatory testing.
Emerging Applications in Disease Modelling
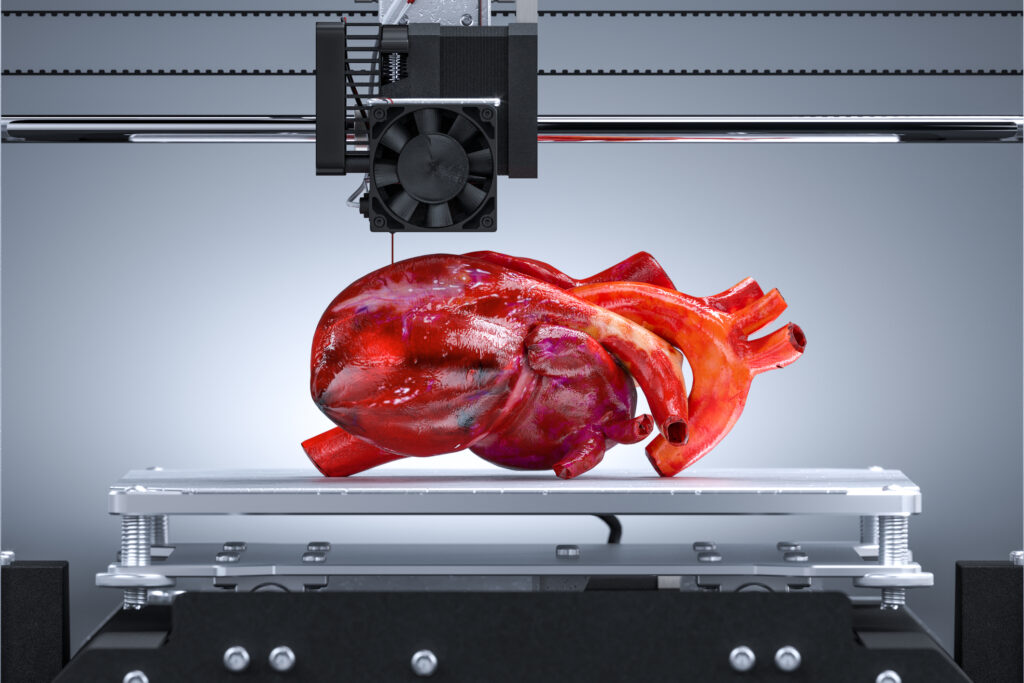
Beyond drug testing, organ-on-a-chip technology is being applied to a growing range of disease models. For instance, cardiac chips created using human stem-cell-derived cardiomyocytes can reproduce the electrical and mechanical behaviour of the heart, enabling researchers to study arrhythmias, drug-induced cardiotoxicity and patient-specific disease mutations.
Similarly, lung-on-a-chip systems that simulate the rhythmic stretching of breathing tissues are helping to investigate respiratory conditions such as asthma, pulmonary fibrosis and viral infections.
Joint-on-a-chip and bone-marrow-on-a-chip models are used to study inflammation, immune responses, and cancer metastasis, while gut-on-a-chip platforms with integrated microbiome components provide insights into digestion, barrier dysfunction, and drug absorption.
Because these systems use human cells, they capture subtle species-specific differences that animal models often miss. This is especially valuable in immunology, oncology and infectious disease research, where the complexity of human biology can lead to outcomes that differ sharply from those observed in animals.
Towards Multi-Organ and Whole-Body Systems
The next frontier is linking multiple organ chips together to form interconnected multi-organ or body-on-a-chip systems. These networks mimic systemic circulation, enabling the study of pharmacokinetics, metabolism, and multi-organ toxicity.
For example, connecting a liver chip to a kidney chip allows researchers to track how a drug is metabolised in the liver and subsequently excreted through renal pathways. Adding gut and vascular modules can simulate oral absorption and systemic distribution.
Ultimately, a full “human-on-a-chip” could replicate key organ interactions that determine overall drug response. Achieving this level of integration remains technically challenging, but steady progress is being made. Advances in microfluidic design, media compatibility and computational modelling are bringing such systems closer to practical use.
The Challenge of Standardisation and Validation
While the progress is impressive, significant challenges remain. One of the biggest is ensuring consistency in cell sourcing and chip fabrication. Variability in stem-cell differentiation protocols, matrix materials or microchannel geometry can lead to differences in performance and reproducibility between laboratories.
This is why standardisation is becoming a priority. The European JRC roadmap stresses the need for agreed-upon testing guidelines, reference materials and data-sharing frameworks. Without these, regulatory authorities cannot easily evaluate or approve OoC-based evidence.
Cost and scalability are also considerations. Although throughput has improved, complex chips remain more expensive and labour-intensive than conventional two-dimensional cultures. Efforts are underway to simplify fabrication and integrate automation to reduce these barriers.
Furthermore, even the most advanced models cannot yet capture every aspect of whole-body physiology. Many lack a fully developed vasculature, immune interactions or long-term stability. Bridging these gaps will require multidisciplinary collaboration across cell biology, bioengineering, microfabrication and computational science.
Integration with Artificial Intelligence and Data Science
As data from OoC experiments multiply, artificial intelligence (AI) and machine learning (ML) are becoming valuable analytical tools. Algorithms can detect subtle patterns in physiological responses, predict drug toxicity and optimise chip design parameters.
Combining AI with high-throughput OoC systems could eventually produce predictive models of human biology far more accurate than traditional approaches. For instance, integrating real-time sensor data with imaging readouts could allow AI systems to identify early biomarkers of tissue stress or therapeutic response.
Such data-driven insights will help refine not only preclinical testing but also clinical trial design, reducing failure rates and development costs.
Implications for Imaging and Translational Research
For researchers in medical imaging and diagnostic development, organ-on-a-chip models provide a new experimental bridge between molecular studies and in vivo observations. They can be used to validate imaging biomarkers, investigate tracer kinetics, or assess therapeutic effects before moving into animal or human trials.
For example, perfused tumour-on-a-chip systems can measure how radiopharmaceuticals or contrast agents distribute and clear within microvascular networks, producing quantitative data relevant to PET, MRI or optical imaging. These experiments can inform clinical imaging strategies and support regulatory submissions.
Furthermore, as chips increasingly incorporate optical transparency and compatible sensor arrays, imaging readouts such as fluorescence lifetime, confocal microscopy, or phase-contrast imaging can be integrated directly into the experimental workflow. This tight coupling of biology and imaging aligns perfectly with modern translational research priorities.
Looking Ahead
The trajectory of organ-on-a-chip development points towards more realistic, accessible and standardised human models for research, drug discovery and diagnostics. The technology is moving from academic novelty to industrial tool, driven by automation, regulatory interest and ethical necessity.
As multi-organ and patient-specific chips become more sophisticated, they could eventually support personalised medicine — testing an individual’s response to therapies before treatment begins. In parallel, integration with AI, imaging and advanced sensors will continue to deepen our understanding of dynamic human biology.
While technical and logistical challenges remain, the progress of the past few years demonstrates that organ-on-a-chip systems are no longer futuristic concepts but practical instruments reshaping biomedical research. Their continued evolution promises not only better science but also safer and more efficient routes from laboratory discovery to patient care.
Disclaimer
The information presented in “Organs on a Chip: Engineering the Future of Human Biology” is intended solely for general educational and informational purposes. While every effort has been made to ensure accuracy and relevance at the time of publication, Open MedScience makes no representations or warranties, express or implied, regarding the completeness, reliability or suitability of the material for any specific purpose.
This article does not constitute scientific, medical, legal, or regulatory advice and should not be relied upon as such. Readers are encouraged to consult qualified professionals and refer to official regulatory or scientific sources for specific guidance. References to organisations, technologies, products, or companies are provided for context and do not imply endorsement or commercial affiliation.
Research and technologies discussed, including organ-on-a-chip systems, may still be under development and subject to change as new data emerge. Open MedScience accepts no responsibility for any loss, injury, or damage arising from the use or interpretation of the information contained herein.
You are here: home » diagnostic medical imaging blog »