Advances in mobile CT technology are beginning to influence the delivery of emergency and critical-care neurology, with a growing focus on taking high-quality brain imaging to the patient rather than transporting the patient to a fixed scanner. This shift is particularly relevant in stroke care, neuro-intensive care units, remote environments, and pre-hospital settings where time, access, and clinical risk all play decisive roles. Over the past few years, a combination of technical innovation, clinical research, and industry investment has advanced mobile head CT scanners from experimental concepts to practical tools, with increasing real-world deployment.
This article explores the most significant developments, including technological progress and operational benefits, early clinical findings, market forces, and future directions.
The push towards mobile brain imaging
For many decades, CT scanners have been large, immovable systems housed in radiology departments behind layers of shielding and infrastructure. Their size, weight, cooling requirements, and mechanical complexity made them unsuitable for point-of-care use. However, emergency neurology—especially stroke—has always been constrained by this static model. The earlier a stroke is diagnosed, the greater the chance of preserving brain tissue and improving long-term outcomes. Moving critically ill patients from an ICU bed or transporting someone rapidly deteriorating in an ambulance can introduce delays and additional clinical risk.
These long-standing challenges created a clear need: compact, reliable CT scanners capable of providing high-quality head imaging at the patient’s bedside or on the move.
A new generation of mobile CT technology
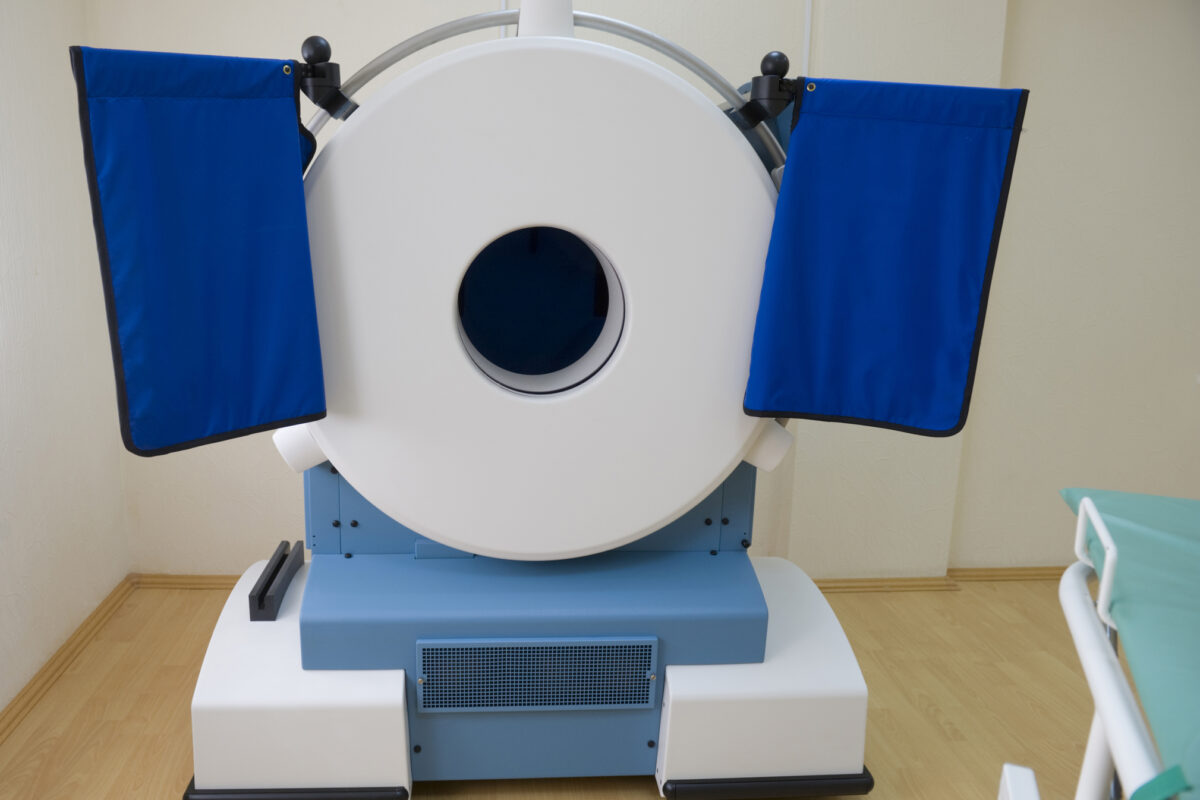
Siemens Healthineers’ Somatom On.site
One of the most discussed developments is Siemens Healthineers’ Somatom On.site, a mobile head CT system specifically designed for point-of-care imaging in intensive care units. Instead of transferring a patient to radiology, the scanner is wheeled directly to the bedside. This approach is particularly relevant for patients with traumatic brain injuries, external ventricular drains, unstable respiratory status, or multiple lines and infusions.
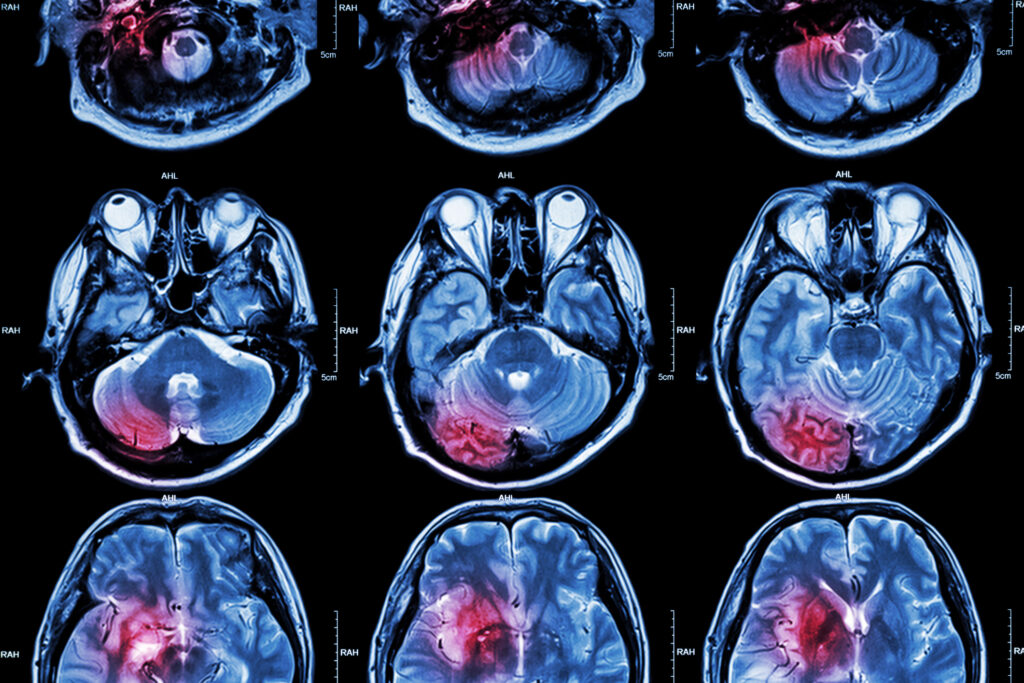
Clinical evaluations comparing the Somatom On.site with a conventional fixed 64-slice CT scanner have shown that image quality is closer to that of stationary systems than that of earlier portable designs. Studies have reported good diagnostic confidence across most brain regions, with only modest challenges in areas prone to motion or beam-hardening artefacts such as the posterior fossa.
Although the system requires more setup time than a standard radiology workflow, it eliminates the risks of transferring patients through hospital corridors, disconnecting them from monitoring equipment, and coordinating multiple staff members. For many hospitals, these workflow improvements alone justify exploration of mobile CT as part of modern critical-care planning.
Micro-X and the rise of ultra-lightweight head CT
Australian company Micro-X has taken a different approach, focusing on weight, power consumption, and rugged design. Its new lightweight head CT prototype—around 70 kg—has been engineered to fit inside a standard ambulance. This makes pre-hospital CT scanning a realistic option rather than a distant aspiration.
Micro-X uses carbon-nanotube x-ray emitters, which allow faster pulsing, smaller geometry, and far lower heating loads than traditional CT tubes. As a result, the scanner does not require the large cooling and housing systems seen in conventional clinical CT systems. Field trials aim to demonstrate accurate assessment of ischaemic and haemorrhagic stroke at the roadside, enabling earlier specialist referral, faster thrombolysis, and potentially significant improvements in patient outcomes.
If proven reliable, such systems could transform stroke pathways in both urban and rural settings. The possibility of deploying CT-equipped ambulances in remote regions—often hours from the nearest major hospital—offers a major opportunity for reducing healthcare inequality.
Integration into mobile stroke units
Mobile stroke units (MSUs) are specially equipped ambulances designed to deliver rapid stroke assessment before the patient reaches the hospital. They typically include a CT scanner, point-of-care laboratory testing, telemedicine connectivity, and a stroke-specialist team.
For many years, MSUs relied on compact but limited CT systems that were often difficult to operate and produced images below the diagnostic standard achieved in hospital scanners. Newer scanners, such as the Somatom On.site are beginning to change this.
Recent deployments have shown that image quality within an MSU can now be sufficient for reliable decision-making regarding thrombolysis and onward triage to thrombectomy centres. As MSUs increasingly integrate scanners designed for resilient mobile use—lighter frames, lower vibration sensitivity, automated positioning, and robust data-transfer protocols—the service becomes more scalable and better suited to longer shifts, extended urban coverage, and national roll-out programmes.
Mobile CT for remote and underserved regions
A further area of growth is the use of mobile CT scanners in rural or underserved regions. Many communities worldwide do not have rapid access to neuroimaging, resulting in late diagnoses, increased morbidity, and higher long-term care costs.
New mobile CT platforms are being trialled in remote clinics, temporary hospitals, and outreach programmes. For instance, lightweight units based on Micro-X technology are being positioned to support remote healthcare in Australia, where long distances and sparsely populated regions create distinctive public-health challenges. Mobile CT bridges the gap between regional clinics and fully equipped tertiary hospitals, improving emergency response capabilities and supporting the early management of head injuries, stroke, and neurological complications.
As more countries invest in mobile diagnostic networks—particularly in areas where hospital resources are concentrated in metropolitan centres—mobile CT is likely to become an important tool in reducing geographical barriers to care.
Workflow transformation in ICUs
One area where mobile CT has shown immediate practical benefit is the neuro-intensive care unit. Traditional imaging workflows often require coordinating multiple staff members to transfer a patient—sometimes intubated, sedated, ventilated, or unstable—along corridors and into lifts before reaching the radiology suite.
Mobile CT significantly reduces:
- Transport time
- Staffing requirements
- Risk of accidental line removal
- Risk of blood-pressure instability or hypoxia during transport
- Interruption to continuous monitoring or ventilation
A recent study comparing mobile and stationary CT workflows in an ICU showed that, although mobile scanning takes longer for the radiographer, the overall patient-centred workflow is far more efficient. Staff remain on the ward, and patients continue to be monitored consistently during the scan.
These operational advantages have contributed to growing interest among hospitals seeking to improve safety and reduce strain on critical-care teams.
Technical challenges still being addressed
While progress is significant, several challenges remain:
Image quality variation
Although new mobile scanners deliver strong results, they are still subject to movement artefacts, tight scanning geometries, and the constraints of smaller gantry systems. The posterior fossa and subtle early ischaemia are more difficult to evaluate in some mobile systems than in full-sized scanners.
Setup time and workflow changes
Mobile CT requires ward space, nearby power access, and well-trained staff capable of navigating both radiographic and environmental challenges. Integration into PACS, RIS, and tele-neurology workflows must also be seamless.
Radiation shielding
Scanning in non-shielded rooms raises questions about radiation protection. Manufacturers now design systems with tightly collimated beams and integrated shielding, but hospital radiation-protection teams must assess each deployment individually.
Cost and maintenance
Although the cost of mobile CT has dropped compared with earlier systems, high-quality scanners remain significant capital investments. Maintenance, calibration, and service contracts must be considered, especially in rural or mobile settings where technical support may be distant.
Market trends and industry growth
The global mobile CT market is expanding steadily, driven by emergency-care demand, technological innovation, and the growing availability of compact imaging platforms. Reports forecast continued growth through the 2030s, with a particular rise in:
- Pre-hospital stroke imaging
- ICU-based point-of-care CT
- Remote and rural diagnostic services
- AI-supported CT reconstruction and workflow automation
As more healthcare systems shift towards decentralised diagnostic models, mobile CT is moving beyond a niche innovation and into a central role in modern emergency imaging.
Implications for UK healthcare
Within the UK, stroke care already relies on rapid access to CT imaging. However, geographical variation, ambulance travel times, and staffing pressures still introduce variation in real-world response times.
Mobile CT could help strengthen regional stroke networks by:
- Providing faster imaging in ambulance services
- Supporting hyperacute stroke centres with earlier triage
- Reducing pressure on radiology departments
- Improving access in remote regions such as parts of Scotland, Wales, and Northern Ireland
- Enhancing ICU imaging capacity in major trauma centres
As NHS trusts look for service improvements that reduce delays and improve outcomes, mobile CT may become increasingly attractive, especially when combined with tele-neurology and AI-enhanced image analysis.
Looking ahead
The next few years are likely to bring further progress in mobile CT technology, including:
- Greater miniaturisation of X-ray tubes
- Improved reconstruction algorithms and noise suppression
- Integrated AI for stroke classification
- More robust ambulance-ready CT platforms
- Enhanced battery-powered or low-power systems
- Expanded clinical trials comparing mobile and stationary imaging across diverse patient groups
The long-term direction points towards a world where imaging no longer depends on physical proximity to a radiology department. Instead, high-quality CT scanning becomes a flexible tool that travels to the patient, supporting faster decisions, improving safety, and reducing clinical risk across many settings.
Conclusion
Mobile CT brain scanners are moving from experimental prototypes to meaningful clinical tools offering tangible benefits in stroke care, neuro-critical care, and remote medicine. Advances in design, image quality, and workflow integration are enabling compact, practical scanners well-suited to real-world challenges. As clinical trials progress and operational models mature, mobile CT is likely to play an increasingly important role in emergency neurology and wider diagnostic imaging services in the UK and abroad.
Disclaimer
The information presented in From Bedside to Ambulance: The New Era of Mobile CT Brain Imaging is provided for general informational and educational purposes only. It is not intended to serve as medical, clinical, regulatory, legal, or professional advice, nor should it be relied upon as a substitute for consultation with qualified healthcare professionals, clinical specialists, medical physicists, radiologists, or regulatory authorities.
All descriptions of technologies, clinical workflows, research findings, market trends, and future directions reflect publicly available information, published studies, and industry developments as of the publication date. While reasonable care has been taken to ensure accuracy, completeness, and relevance, Open MedScience makes no representations or warranties, express or implied, regarding the accuracy, reliability, or applicability of the content in specific clinical, operational, or commercial contexts.
References to specific companies, products, or technologies are included for informational purposes only and do not constitute endorsement, recommendation, or commercial affiliation. Performance, availability, regulatory approval status, and clinical suitability of medical devices may vary by jurisdiction and over time.
Clinical decisions, procurement choices, and patient-care pathways should always be based on local clinical guidelines, regulatory frameworks, professional judgement, and direct consultation with appropriately qualified experts. Open MedScience accepts no responsibility or liability for any loss, harm, or adverse outcomes arising from reliance on the information contained in this article.
home » blog » medical imaging modalities »