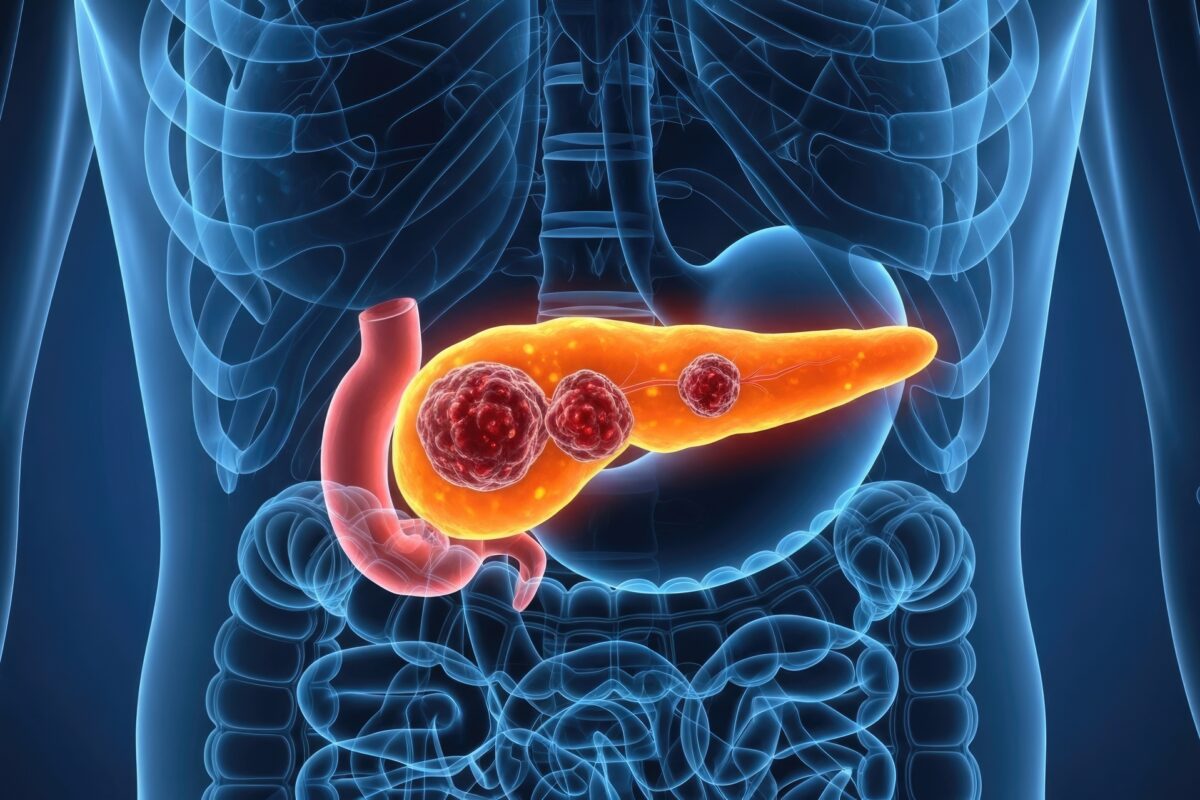
Pancreatic cancer remains one of the most challenging malignancies in modern medicine. It is often diagnosed late, progresses rapidly, and responds poorly to many standard treatments. Survival rates have changed little over the decades, leaving clinicians, researchers, and patients urgently searching for meaningful advances. In recent years, however, a series of developments across early detection, device-assisted therapies, molecular targeting, and immunological strategies have begun to shift expectations. While no single breakthrough has transformed outcomes overnight, the combined momentum is significant.
This article reviews the most important recent developments shaping pancreatic cancer research and care as we move through 2025, focusing on what is most likely to influence clinical practice and what may define the next generation of therapies.
Earlier detection: addressing the central problem
The greatest obstacle in pancreatic cancer has always been timing. Most patients are diagnosed when the disease is already locally advanced or metastatic, ruling out curative surgery. Research efforts are now strongly focused on identifying the disease earlier, particularly in people with vague or non-specific symptoms who would not traditionally be fast-tracked for imaging.
One of the most promising approaches under evaluation in the UK is breath testing. Large-scale clinical studies are assessing whether patterns of volatile organic compounds in exhaled breath can act as biomarkers for pancreatic cancer. The aim is not to replace imaging or biopsy, but to provide a rapid, non-invasive triage tool that can flag higher-risk individuals for urgent investigation. If validated, this approach could fit naturally into primary care pathways and help reduce diagnostic delays.
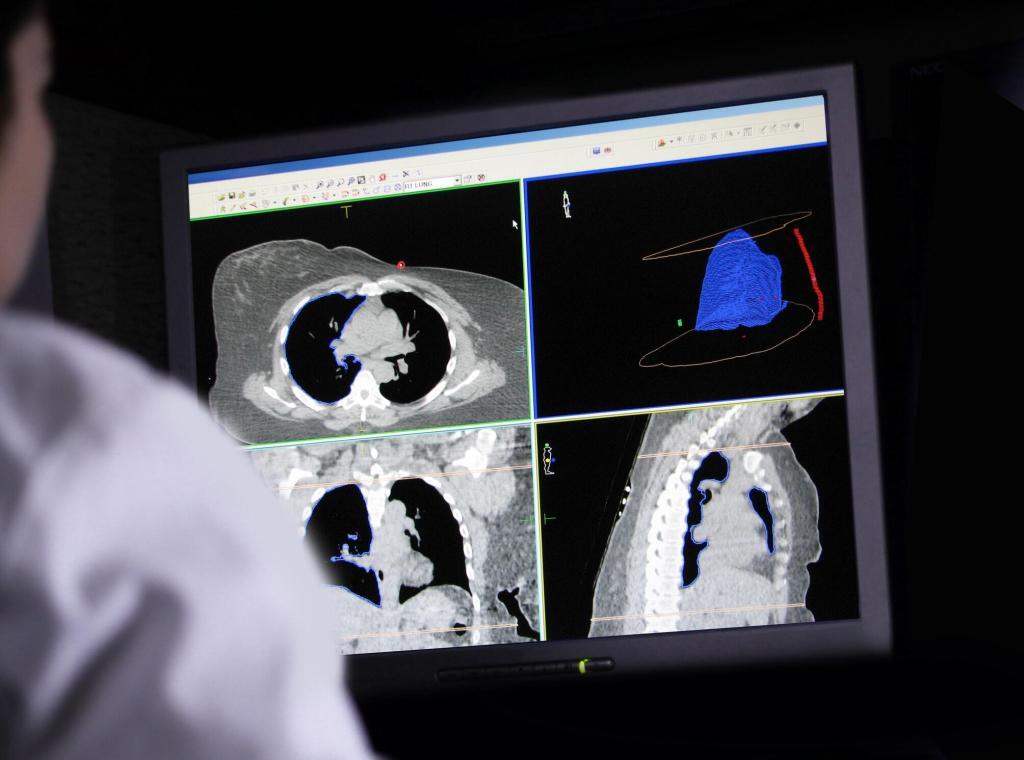
Blood-based tests are also gaining traction, especially in defined higher-risk groups. One area of interest involves people over 50 who develop new-onset type 2 diabetes. An underlying pancreatic tumour drives a small but clinically meaningful proportion of these cases. Multi-analyte blood tests combining circulating tumour DNA, protein markers, and clinical variables are being trialled to identify those who may benefit from early imaging. This risk-stratified strategy avoids population-wide screening while still targeting those most likely to benefit.
Together, these detection-focused efforts represent a pragmatic shift away from broad screening and towards smarter identification of risk, where sensitivity, speed, and feasibility matter as much as absolute diagnostic certainty.
Tumour Treating Fields: a device-based survival gain
One of the clearest late-stage clinical advances has come from an unexpected direction: medical devices. Tumour Treating Fields (TTFields) use low-intensity, alternating electric fields delivered through external electrodes to disrupt cancer cell division. The technology has already been used in glioblastoma, and recent Phase III data suggest a role in pancreatic cancer as well.
In patients with unresectable locally advanced pancreatic adenocarcinoma, adding TTFields to standard chemotherapy (gemcitabine plus nab-paclitaxel) has been associated with an overall survival improvement. Importantly, this benefit appears to come without the systemic toxicity that often limits the efficacy of combination regimens. Pain-related outcomes and quality-of-life measures have also been highlighted in trial reporting, which is especially relevant in a disease with high symptom burden.
While adoption will depend on regulatory decisions, cost considerations, and real-world feasibility, TTFields stand out as a rare example of a non-pharmacological intervention showing a survival signal in pancreatic cancer. It also reinforces a broader trend towards multimodal treatment strategies that extend beyond drugs alone.
Targeting KRAS: a long-standing barrier begins to crack
KRAS mutations are present in the vast majority of pancreatic ductal adenocarcinomas and have long been considered “undruggable”. That assumption is now changing. The most significant recent progress involves drugs that target KRAS and related RAS proteins in their active, signalling state.
Daraxonrasib (RMC-6236) is a multi-selective RAS(ON) inhibitor that has generated enough early clinical activity to move into Phase III trials in pancreatic cancer. Unlike earlier agents that targeted only specific KRAS mutations, this approach aims to inhibit a broader range of RAS-driven signalling, which is crucial given the genetic diversity of pancreatic tumours.
The launch of large, randomised trials marks an important milestone. It signals a transition from proof-of-concept to definitive testing, where survival, durability of response, and resistance mechanisms can be properly assessed. These programmes also highlight the growing importance of molecular profiling. Increasingly, patients with advanced disease are being tested using tumour tissue or circulating DNA to guide trial eligibility and treatment selection.
While challenges remain, including adaptive resistance and tumour heterogeneity, RAS-targeted therapies are no longer theoretical. They are becoming central to the future treatment landscape.
Immunotherapy: slower progress, sharper focus
Pancreatic cancer has been notoriously resistant to conventional immunotherapy. Checkpoint inhibitors, which have transformed outcomes in melanoma and lung cancer, have shown limited benefit except in rare molecular subtypes. Rather than abandoning immunological approaches, researchers have refined their strategies.
Therapeutic cancer vaccines are one area of renewed interest. These approaches aim to train the immune system to recognise tumour-specific antigens, often using personalised neoantigen profiles derived from an individual’s tumour. Early-phase studies suggest that some vaccines can generate measurable immune responses, and ongoing trials are exploring whether these responses translate into longer disease control when combined with chemotherapy or other immune-modulating agents.
Researchers are also studying ways to modify the tumour microenvironment, which in pancreatic cancer is dense, fibrotic, and immunosuppressive. Strategies that alter stromal barriers or reprogramme immune cell populations may be essential for immunotherapy to work effectively in this setting. Progress is incremental, but the field is more targeted and biologically informed than it was even five years ago.
Blocking spread: insights into metastasis biology
Metastasis is the leading cause of death in pancreatic cancer, and recent basic science research has begun to uncover molecular drivers of tumour spread. Studies identifying proteins linked with aggressive behaviour and metastatic potential are opening new avenues for drug development.
Targets such as SPP1 have been implicated in pathways that promote invasion and dissemination. While these findings are still at an early stage, they matter because they shift attention towards preventing progression rather than simply shrinking established tumours. Over time, therapies aimed at limiting spread could complement existing treatments and improve long-term outcomes.
What this means for patients and clinicians
Taken together, these developments suggest that pancreatic cancer research is entering a more productive phase. Earlier detection tools could help shift diagnosis towards stages where treatment is more effective. Device-assisted therapies are adding to the therapeutic toolkit without compounding toxicity. Molecularly targeted drugs are finally challenging the dominance of KRAS-driven disease. Immunotherapy research is becoming more precise, and metastasis biology is receiving sustained attention.
For clinicians, this reinforces the importance of multidisciplinary care, molecular testing, and awareness of clinical trial options. For patients, it means that conversations about treatment and prognosis increasingly include emerging strategies rather than only long-established regimens.
Progress remains uneven, and pancreatic cancer is still a formidable diagnosis. Yet the direction of travel is clearer than it has been for many years. Incremental advances, when combined, can change standards of care. The next decade is likely to be shaped not by a single dramatic discovery, but by the steady integration of earlier diagnosis, more intelligent targeting, and more personalised treatment strategies.
In a field that has long struggled to deliver good news, that shift alone is meaningful.
Q &A on the Latest Developments
Why is pancreatic cancer so difficult to treat?
Pancreatic cancer is challenging because it is usually diagnosed late, when the disease has already spread beyond the pancreas or become locally advanced. Early symptoms are often vague, such as abdominal discomfort, weight loss, or fatigue, and do not immediately trigger urgent investigation. The biology of the disease also plays a role. Pancreatic tumours tend to grow within a dense, fibrotic environment that limits drug penetration and suppresses immune responses. In addition, most tumours are driven by mutations that have historically been very hard to target with drugs.
What has changed recently in terms of early detection?
Early detection has become one of the strongest areas of progress. Rather than aiming for population-wide screening, researchers are focusing on identifying people at higher risk and testing them more intelligently. In the UK, extensive studies are evaluating breath tests that look for chemical patterns associated with pancreatic cancer. These tests are quick, non-invasive, and potentially suitable for use in primary care as a triage tool.
Blood tests are also being studied, particularly in people over 50 who develop new-onset type 2 diabetes. In a small but significant proportion of cases, the diabetes is triggered by an underlying pancreatic tumour. Multi-marker blood tests may help identify which individuals need urgent imaging, improving the chances of diagnosis at a more treatable stage.
Are any of these detection tools available in routine care yet?
At present, most of these tools are still in clinical trials or pilot studies. They are not replacements for scans or biopsies, but they could help decide who should be investigated more quickly. If the ongoing studies confirm their accuracy and practicality, some may begin to enter routine care pathways over the next few years, particularly within the NHS.
What are Tumour Treating Fields, and why are they important?
Tumour Treating Fields is a treatment that uses low-intensity electric fields to interfere with cancer cell division. The fields are delivered via electrodes placed on the skin and continuously target the tumour region. In pancreatic cancer, recent Phase III trial results have shown that adding this therapy to standard chemotherapy can extend overall survival in people with unresectable locally advanced disease.
Its importance lies in the fact that it provides a survival benefit without adding the systemic side effects commonly seen with extra drugs. This makes it especially relevant in pancreatic cancer, where maintaining quality of life is a significant concern.
Does this mean chemotherapy is being replaced?
No. Chemotherapy remains the backbone of treatment for most patients. What is changing is the way treatments are combined. Instead of simply adding more drugs, which often increases toxicity, newer approaches are layering different types of therapy together, such as devices, targeted agents, or immune-based strategies. The goal is to improve outcomes without overwhelming patients with side effects.
What progress has been made in targeting KRAS mutations?
KRAS mutations are present in the majority of pancreatic cancers and have been a significant obstacle for decades. Recently, new drugs have been developed that can block KRAS-related signalling more broadly. One of the most advanced examples is a drug that targets RAS proteins in their active state and has now moved into significant Phase III trials.
This marks a turning point. For the first time, drugs aimed at the core genetic driver of pancreatic cancer are being tested in studies designed to change standard practice. While these treatments are not yet available outside trials, they represent one of the most promising directions in the field.
Will all patients benefit from KRAS-targeted therapies?
Probably not. Pancreatic cancer is genetically complex, and tumours can develop resistance to targeted treatments over time. That is why molecular testing is becoming increasingly important. By analysing tumour tissue or circulating DNA in the blood, clinicians can identify which patients are most likely to benefit from specific therapies or clinical trials.
Why has immunotherapy been less effective in pancreatic cancer?
Immunotherapy relies on the immune system recognising and attacking cancer cells. In pancreatic cancer, the tumour environment actively suppresses immune activity and creates physical barriers that immune cells struggle to penetrate. As a result, treatments such as checkpoint inhibitors have shown limited benefit except in rare molecular subtypes.
Is immunotherapy research still ongoing?
Very much so. The focus has shifted towards more tailored approaches, including personalised cancer vaccines that train the immune system to recognise tumour-specific targets. Researchers are also studying ways to alter the tumour microenvironment to make immune-based treatments more effective. Progress is gradual, but the strategies are becoming more refined and grounded in tumour biology.
What is being done about metastasis?
Most deaths from pancreatic cancer are caused by metastatic disease. Recent research has identified molecules involved in tumour spread, opening up new possibilities for treatment. These discoveries are still at an early stage, but they highlight a growing interest in preventing progression and dissemination, not just treating established tumours.
What do these developments mean for patients today?
For patients, the most immediate impact is greater access to clinical trials and more personalised treatment planning. Molecular testing is playing a larger role, and new therapies are increasingly being tested alongside standard care. While pancreatic cancer remains a serious diagnosis, patients today are more likely to be offered innovative options than they were even a few years ago.
What should clinicians take from these advances?
Clinicians should be aware that pancreatic cancer care is becoming more complex and more individualised. Early referral, participation in research studies, and routine consideration of molecular profiling are becoming central elements of good practice. Collaboration across specialties is essential as new diagnostic and therapeutic tools emerge.
Is there reason for optimism?
Cautious optimism is appropriate. Pancreatic cancer still has one of the poorest survival rates among major cancers, but the pace of research has clearly increased. Progress is coming from multiple directions at once, and that combined effect has the potential to reshape outcomes over time.
Disclaimer
The information presented in this article is intended for general informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment, and should not be relied upon as a substitute for professional medical guidance. Clinical decisions should always be made in consultation with qualified healthcare professionals who are familiar with an individual’s medical history and circumstances.
Research findings, clinical trials, and emerging therapies discussed reflect the state of knowledge at the time of writing and may evolve as new evidence becomes available. Availability of tests, treatments, and technologies may vary by region and healthcare system, including within the NHS.
Open MedScience does not endorse any specific test, device, drug, or treatment mentioned in this article. Readers are encouraged to seek advice from their doctor, specialist, or other appropriately qualified healthcare provider regarding any questions or concerns related to pancreatic cancer or its management.
home » blog » medicine »