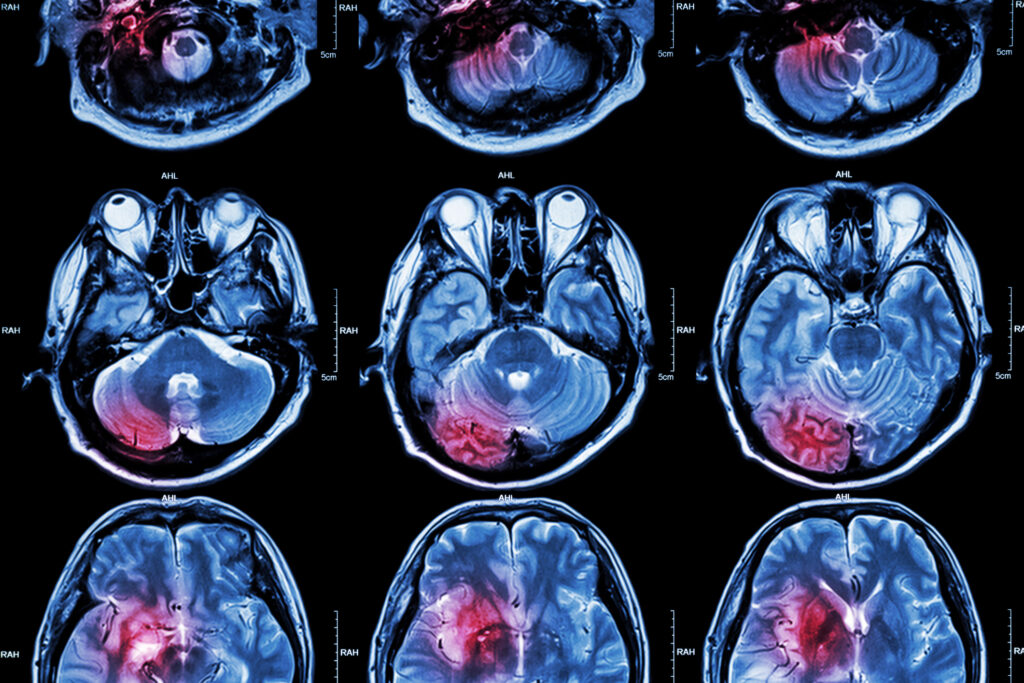
Medical imaging sits at the centre of modern healthcare. From emergency departments to oncology clinics and routine outpatient services, images now guide a huge proportion of clinical decisions. At the same time, radiology, the medical speciality that interprets and applies these images, is undergoing rapid change. What was once a discipline focused mainly on producing and reading scans is becoming a highly connected, data-driven diagnostic service. Understanding these developments helps explain why imaging is no longer just about pictures, but about turning visual information into faster, safer and more accurate patient care.
Before exploring what is changing, it is useful to clarify the difference between the two terms that are often confused. Medical imaging refers to the technologies and processes used to create images of the body. This includes X-ray, CT, MRI, ultrasound, mammography and nuclear medicine techniques such as PET and SPECT. It also covers the professionals who operate scanners, ensure quality control and manage imaging data. Radiology, on the other hand, is the medical speciality that uses these images to diagnose disease, advise clinicians and guide treatment. Radiologists are medically trained doctors who interpret imaging studies and increasingly perform image-guided procedures. In simple terms, medical imaging provides the tools, while radiology turns those tools into clinical decisions.
Artificial intelligence is becoming part of everyday workflow
One of the most visible developments in recent years has been the integration of artificial intelligence into imaging and radiology. Early AI tools focused on narrow tasks such as detecting lung nodules or identifying fractures. While these systems demonstrated impressive technical performance, they often struggled to fit naturally into clinical routines. The current shift is towards embedding AI directly into reporting platforms, picture archiving systems and workflow management tools.
This approach treats AI less as a standalone product and more as background infrastructure. Instead of radiologists having to open a separate application, the software quietly assists during normal reporting. It may highlight areas of concern, prioritise urgent cases in worklists, or automatically measure structures such as tumours and organs. The aim is not to replace professional judgement, but to remove repetitive tasks and reduce the chance of missing subtle findings during busy reporting sessions.
Another important use of AI is in administrative and communication tasks. Generative language systems are being applied to reporting workflows to improve speech recognition, standardise report structure and reduce time spent on documentation. These systems can suggest phrasing that aligns with clinical guidelines, help summarise relevant patient history, and automatically populate structured report fields. For radiologists working under constant time pressure, this type of support can make a significant difference to efficiency and consistency.
At the same time, caution remains essential. AI systems can produce confident outputs that are incorrect or misleading. In medicine, this risk carries real consequences. As a result, hospitals and professional bodies are placing strong emphasis on governance, transparency and human oversight. Radiologists remain responsible for the final report, and AI is increasingly viewed as a supportive assistant rather than an independent decision-maker.
New scanner technology is changing image quality and dose balance
While software is advancing rapidly, hardware innovation continues to reshape what scanners can achieve. One of the most important recent developments in CT imaging is the introduction of photon-counting detector technology. Traditional CT systems measure incoming X-ray energy in a combined way. Photon-counting detectors instead register individual photons and their energy levels. This allows for higher spatial resolution, improved contrast detail and better separation of different materials within the body.
For patients, this translates into clearer images with the potential for lower radiation dose. For clinicians, it means improved confidence when assessing small structures, subtle disease changes and complex anatomy. Areas such as cardiac imaging, lung disease assessment and musculoskeletal imaging are likely to benefit significantly from this technology. Over time, as more centres adopt photon-counting systems, scanning protocols and diagnostic pathways will continue to evolve.
In nuclear medicine, similar progress is underway through the development of long axial-field-of-view and total-body PET scanners. These systems can image a much larger portion of the body at once, dramatically increasing sensitivity. This enables shorter scan times, lower injected tracer doses or higher image quality, depending on clinical priorities. More importantly, total-body PET opens new possibilities for simultaneously tracking disease processes across the entire body. Researchers can observe how drugs move through tissues, how inflammation spreads and how cancers respond to therapy in near real time. This has major implications for personalised medicine and drug development.
Portable and low-field MRI is expanding access
MRI has traditionally been associated with large, expensive installations that require specialist rooms and infrastructure. Recent developments in ultra-low-field and portable MRI systems are beginning to challenge this model. These scanners operate at much lower magnetic field strengths than conventional hospital MRI units, allowing them to be smaller, lighter and easier to install.
While image resolution is lower than that of high-field MRI, portable systems can still provide clinically useful information, particularly for brain imaging. The ability to bring MRI closer to the patient is especially valuable in intensive care units, emergency departments and remote settings. Moving critically ill patients to a scanner can be risky and resource-intensive. Portable MRI enables bedside imaging, reducing transport risks and improving access to timely diagnosis.
This trend reflects a broader shift in medical imaging: instead of expecting patients to travel to technology, technology is increasingly being designed to travel to patients. As portable systems improve and clinical evidence grows, their role in routine care is likely to expand.
Radiology is becoming more interventional and patient-facing
Another important development is the continued growth of interventional radiology. Using real-time imaging guidance, radiologists perform minimally invasive procedures that once required open surgery. These include tumour ablation, targeted drug delivery, vascular interventions and image-guided biopsies.
Advances in imaging quality, navigation software and robotic assistance are making these procedures safer and more precise. Patients often benefit from shorter hospital stays, reduced pain and faster recovery compared with traditional surgical approaches. This has changed the public perception of radiology. Instead of being a behind-the-scenes diagnostic service, radiology is becoming a visible part of direct patient care.
This shift also affects training and workforce planning. Radiologists now need a broader skill set that combines diagnostic expertise with procedural competence and patient communication. As imaging-guided therapies continue to expand, the boundary between radiology and other clinical specialities will become increasingly collaborative.
Connected systems and remote reporting are reshaping service delivery
The volume of imaging studies continues to rise each year, driven by ageing populations, expanding screening programmes and more complex clinical pathways. At the same time, many healthcare systems face shortages of trained radiologists. To manage this imbalance, digital connectivity and remote reporting have become essential.
Teleradiology allows images to be reported by specialists who may be located in different hospitals, regions or even countries. This enables round-the-clock coverage, access to subspecialist expertise and more flexible workforce models. Modern systems also allow intelligent case distribution, ensuring that urgent studies are prioritised and directed to appropriate readers.
Beyond reporting, connectivity supports multidisciplinary collaboration. Clinicians can review images together in virtual meetings, share annotated studies and integrate imaging findings directly into electronic patient records. This level of integration helps reduce communication errors and supports more coordinated care.
However, greater connectivity also brings challenges. Cybersecurity has become a major concern, as imaging systems handle large volumes of sensitive patient data and rely on networked infrastructure. Protecting these systems is now a core responsibility of imaging departments and healthcare organisations.
Quantitative imaging is turning pictures into data
Traditionally, radiology reports were largely descriptive. A radiologist might note the presence of a lesion, comment on its appearance and provide an interpretation. Increasingly, imaging is becoming quantitative. Software tools can automatically measure tumour volumes, calculate tissue characteristics and track changes over time with high precision.
This shift supports more objective monitoring of disease progression and treatment response. In oncology, for example, quantitative imaging can help assess whether a therapy is working long before visible size changes appear. In chronic diseases such as liver fibrosis or lung disease, imaging biomarkers can provide valuable information about disease severity and risk.
As imaging becomes increasingly data-rich, radiologists are assuming a new role as interpreters of complex quantitative information. This requires closer collaboration among clinicians, physicists, and data scientists, as well as new validation and reporting standards.
What does all of this mean for the future of care?
Taken together, these developments point to a future in which radiology and medical imaging are more integrated, more efficient, and more central to clinical decision-making than ever before. Patients are likely to experience faster diagnosis, more personalised treatment planning and improved access to imaging services. Clinicians will increasingly rely on imaging not only to confirm disease, but to guide therapy choices and monitor outcomes in real time.
For the professionals working in this field, the pace of change brings both opportunity and responsibility. New technologies require ongoing education, careful evaluation and strong ethical oversight. The goal is not to adopt innovation for its own sake, but to ensure that every advancement genuinely improves patient care.
Radiology began as a discipline focused on shadows on film. Today, it sits at the intersection of medicine, engineering and data science. As scanners become smarter, software becomes more capable, and healthcare systems become more connected, the difference between medical imaging and radiology remains clear, yet their relationship is closer than ever. Medical imaging provides the tools and data, while radiology turns that information into action. Together, they are shaping a new era of diagnosis and treatment that is faster, more precise, and more responsive to patients’ needs.
Disclaimer
The information provided in this article is intended for general educational and informational purposes only. It does not constitute medical advice, clinical guidance, diagnosis, or treatment recommendations. While every effort has been made to ensure accuracy at the time of publication, medical imaging technologies, clinical practices, and regulatory standards continue to evolve, which may affect the relevance of specific details over time. Readers should not rely on this content as a substitute for professional medical consultation and should always seek advice from qualified healthcare professionals regarding individual health concerns or clinical decisions. Open MedScience accepts no responsibility for any actions taken based on the information presented in this article.