The Investigational New Drug (IND) application is a critical step in the process of drug development in the United States. This formal request to the US Food and Drug Administration (FDA) allows pharmaceutical companies or research institutions to legally administer an investigational drug or biological product to humans for the purpose of conducting clinical trials. This article explores the various types of INDs, the submission process, the regulatory requirements, and the steps involved in obtaining authorisation for human clinical trials. It also outlines the importance of the IND in ensuring safety and efficacy before a drug or biological product reaches the market.
Introduction to the Investigational New Drug (IND) Application
The Investigational New Drug (IND) application is a pivotal document in the drug development pipeline, serving as a formal request to the US Food and Drug Administration (FDA) for permission to administer a new drug or biological product to humans in clinical trials. The IND is necessary before any human subject is exposed to an investigational drug, ensuring that clinical research is conducted under rigorous scientific and ethical standards. It is designed to safeguard the health and safety of human participants whilst also facilitating innovation in the pharmaceutical industry.
What Is an Investigational New Drug?
An Investigational New Drug (IND) refers to a new drug or biological product that is in the process of being tested but has not yet received FDA approval for marketing. These drugs are at a preliminary stage, meaning their safety and efficacy in humans are still being evaluated. The investigational stage is crucial because, at this point, extensive nonclinical laboratory and animal studies have already been conducted. However, before moving to clinical trials involving human subjects, the manufacturer or researcher must obtain authorisation from the FDA through an IND application.
Types of IND Applications
There are several types of IND applications, each serving different purposes within the research and development process. Understanding the different categories of INDs helps clarify the scope of the application process and the specific regulations that apply.
Commercial IND
A Commercial IND is typically submitted by pharmaceutical companies or biotechnology firms intending to market the drug after successful clinical trials. This type of IND supports the traditional drug development pathway, which includes a series of well-defined phases (Phase I, II, and III) of clinical research. Each phase builds upon the findings of the previous one, with increasing numbers of human subjects involved in later phases.
Investigator-Initiated IND
In some cases, independent investigators or academic institutions may submit an IND application to conduct clinical trials on an investigational drug. These are known as Investigator-Initiated INDs. The sponsor in this scenario is the individual researcher, rather than a pharmaceutical company. Such trials are often aimed at exploring new uses for existing drugs or understanding disease mechanisms, rather than commercial development.
Treatment IND
A Treatment IND is submitted for drugs that are being developed to treat serious or life-threatening conditions, particularly when no comparable or satisfactory alternative treatments exist. This type of IND allows patients who are not eligible for clinical trials to access potentially life-saving medications before the product receives full marketing approval.
Emergency Use IND
An Emergency Use IND is requested when an investigational drug must be used in an emergency situation where no other treatments are available, and there isn’t enough time to submit a standard IND application. This category allows the FDA to quickly authorise the use of an investigational drug for a single patient or a small group of patients.
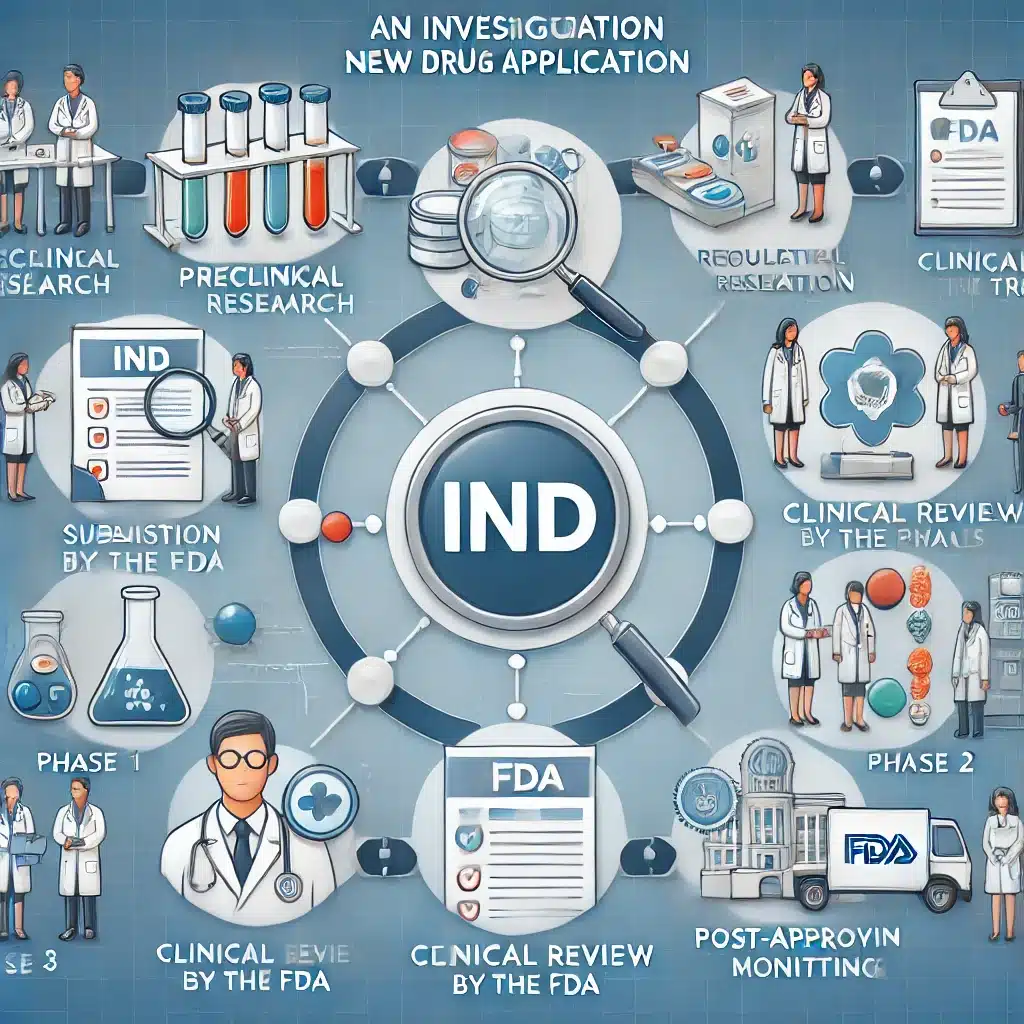
The IND Submission Process
The process of submitting an IND to the FDA involves several key steps, beginning with the preparation of the application and concluding with the FDA’s decision. The application itself consists of three major components: preclinical data, clinical trial protocols, and manufacturing information.
Preclinical Data
Preclinical data forms the foundation of the IND application. This section includes results from laboratory and animal studies that provide evidence of the investigational drug’s safety and biological activity. The data must demonstrate that the drug is reasonably safe for testing in humans and provide insight into potential toxic effects or adverse reactions.
Clinical Trial Protocols
The clinical trial protocols outline the planned studies involving human participants. These protocols must detail the objectives, design, methodology, and statistical considerations of the proposed clinical trial. They also specify the criteria for patient selection, the dosing regimen, and the procedures for monitoring patient safety. The protocols serve as a roadmap for the study, ensuring that it will be conducted ethically and scientifically.
Chemistry, Manufacturing, and Control Information (CMC)
This section of the IND application focuses on the production of the investigational drug. The sponsor must provide comprehensive information on the drug’s composition, its manufacturing process, and the measures in place to ensure the drug’s quality and consistency. The CMC data is crucial for ensuring that the drug can be manufactured reliably and safely at the required scale for clinical trials.
FDA Review and Decision Process
Once the IND application is submitted, the FDA has 30 calendar days to review the submission. During this time, the agency assesses the safety and scientific validity of the proposed clinical trials. The FDA review process involves experts from various disciplines, including pharmacologists, toxicologists, chemists, and clinical reviewers.
The review focuses on several critical questions:
- Does the preclinical data support the safety of the drug in humans?
- Are the clinical trial protocols well-designed to answer the key scientific questions?
- Is the investigational drug manufactured in a way that ensures its safety and quality?
FDA Responses to an IND
At the end of the 30-day review period, the FDA will respond in one of three ways:
- Allow the clinical trial to proceed: If the IND is approved, the sponsor can begin the clinical trial as outlined in the application.
- Impose a clinical hold: If the FDA has concerns about the safety of the drug or the design of the trial, it may place the trial on hold. The sponsor must address the FDA’s concerns before the trial can proceed.
- Request additional information: In some cases, the FDA may ask the sponsor to provide more data or clarification on certain aspects of the application before making a final decision.
The Role of the Institutional Review Board (IRB)
While the FDA is responsible for approving the IND application, an Institutional Review Board (IRB) must also review and approve the clinical trial before it begins. The IRB is an independent body that ensures the rights, welfare, and safety of human participants are protected. The IRB’s approval is an essential part of the ethical framework for conducting clinical research.
Phases of Clinical Trials
Once an IND is approved, the investigational drug moves through three key phases of clinical trials, each with specific objectives.
Phase I: Safety and Dosage
Phase I trials are the first step in testing the drug in humans. These trials typically involve a small number of healthy volunteers or patients. The primary goal is to assess the drug’s safety and determine the appropriate dosage range. Researchers also monitor how the drug is absorbed, distributed, metabolised, and excreted by the body.
Phase II: Efficacy and Side Effects
Phase II trials involve a larger group of patients and focus on evaluating the drug’s effectiveness in treating the target condition. Researchers also gather more data on the drug’s safety and potential side effects. Phase II trials help refine the dosing regimen and provide early indications of the drug’s therapeutic potential.
Phase III: Large-Scale Efficacy and Safety
Phase III trials are conducted on an even larger scale and involve hundreds or thousands of patients. These trials provide a more comprehensive assessment of the drug’s efficacy and safety in a broader patient population. The data from Phase III trials are often used to support the submission of a New Drug Application (NDA) or Biologics License Application (BLA) for FDA approval.
Special Considerations for Biological Products
The IND application process for biological products, such as vaccines, gene therapies, and monoclonal antibodies, follows the same general principles as for traditional drugs. However, biological products are more complex and require additional considerations, particularly regarding their manufacturing and quality control.
Biological products are often derived from living organisms, which introduces variability in the manufacturing process. As a result, the CMC section of the IND for a biological product must include detailed information on the source of the biological material, the manufacturing processes, and the steps taken to ensure the consistency and purity of the final product.
Importance of Good Manufacturing Practice (GMP)
Throughout the development process, adherence to Good Manufacturing Practice (GMP) is essential for ensuring the safety and quality of the investigational drug. GMP regulations require that drugs are consistently produced and controlled according to quality standards. For an IND, the sponsor must demonstrate that the investigational drug is manufactured in compliance with GMP to protect the safety of human participants in clinical trials.
Safety Monitoring and Reporting Requirements
Once a clinical trial begins, the sponsor has ongoing responsibilities to monitor the safety of the participants and report any adverse events to the FDA. This process includes submitting regular safety reports, known as Investigational New Drug Safety Reports (IND Safety Reports), which detail any serious or unexpected adverse reactions that occur during the trial.
The FDA closely monitors these reports to ensure that the risk-to-benefit ratio remains acceptable as the trial progresses. If new safety concerns arise, the FDA has the authority to halt the trial, modify the protocols, or take other actions to protect the participants.
Expanded Access and Compassionate Use
For patients with serious or life-threatening conditions who do not qualify for clinical trials, the FDA allows access to investigational drugs through expanded access programs, often referred to as “compassionate use.” Under these programs, patients can receive investigational drugs outside of clinical trials if there are no other available treatments. Sponsors must submit an IND for expanded access, and the FDA must approve the request, ensuring that the investigational drug presents an appropriate risk-to-benefit ratio for the specific patient or group of patients.
Types of Expanded Access Programs
Expanded access programs are divided into several categories, depending on the circumstances and the number of patients involved.
Individual Patient Expanded Access
This is the most common type of expanded access, allowing a single patient to receive an investigational drug outside of a clinical trial. The patient’s physician, in collaboration with the drug sponsor, submits a request to the FDA. The FDA evaluates the application to ensure the drug is likely to provide a potential benefit without posing an unreasonable risk to the patient.
Intermediate Expanded Access -Size Patient Population
When a group of patients with a similar medical condition needs access to an investigational drug but does not qualify for clinical trials, the FDA may approve an intermediate-size expanded access program. This is typically used for conditions that are rare or when clinical trials are not feasible for logistical reasons.
Expanded Access for Large Patient Populations
In certain situations where a drug shows promise in treating a widespread serious condition, the FDA may authorise access for a large patient population. This usually occurs when a drug is in late-stage clinical trials and early data suggests significant potential benefits. Expanded access for large populations ensures that more patients can benefit from the investigational treatment before it is formally approved for market use.
Conditions for Expanded Access
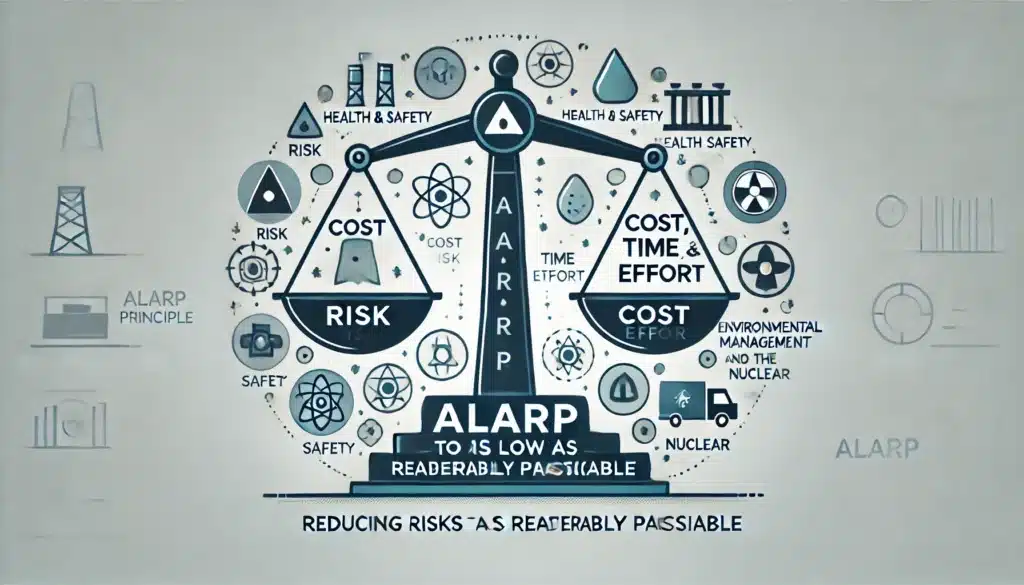
Before an expanded access IND can be granted, the FDA requires the following conditions to be met:
- Serious or Life-Threatening Condition: The patient must have a serious or life-threatening disease or condition for which there are no satisfactory alternative treatments available.
- Lack of Alternative Treatment: There must be no comparable or satisfactory therapy available to the patient. The investigational drug must provide a potential benefit over existing treatments.
- Potential Benefit Outweighs Risks: The FDA must determine that the potential benefits of using the investigational drug outweigh the risks based on the available evidence from preclinical and early clinical studies.
- No Interference with Clinical Trials: The expanded access must not interfere with the completion of clinical trials that could provide broader access to the drug in the future.
Post-IND Approval and the Path to New Drug Application (NDA)
After the successful completion of Phase III trials, the sponsor can submit a New Drug Application (NDA) or Biologics License Application (BLA) to the FDA to seek formal approval for marketing the drug. The NDA contains all the data from the preclinical studies, clinical trials, and information about the drug’s manufacturing processes. This process is highly detailed and must convincingly demonstrate the drug’s safety, efficacy, and manufacturing quality to gain approval.
Components of the NDA/BLA Submission
An NDA or BLA includes a vast array of data and documentation. Some of the critical components include:
- Preclinical and Clinical Data: Comprehensive data from all phases of clinical trials, as well as preclinical testing, are submitted to support the claim that the drug is safe and effective.
- Manufacturing Information: Detailed information on the manufacturing process, ensuring the drug can be consistently produced at a high quality. This includes compliance with GMP standards.
- Labelling: Proposed labelling for the drug, including information on indications, dosage, safety warnings, and instructions for use.
- Patent Information: Any relevant patents that apply to the drug must be disclosed to the FDA, including data exclusivity claims.
- Risk Evaluation and Mitigation Strategies (REMS): For certain drugs that pose high risks, an REMS may be required. REMS outlines strategies to ensure that the drug’s benefits outweigh its risks.
FDA Approval and Post-Market Surveillance
Once the NDA or BLA is submitted, the FDA begins a rigorous review process. During this period, a panel of experts in various scientific and medical fields assesses the submission, including the quality of the data, the manufacturing process, and the proposed labelling. If the review is positive, the FDA will approve the drug for marketing.
Accelerated Approval and Priority Review
In cases where the investigational drug addresses a critical unmet need or treats a serious condition, the FDA may grant accelerated approval or priority review status. These pathways allow drugs to reach the market more quickly based on early evidence, especially when they fill an important therapeutic gap.
Accelerated Approval
Accelerated approval allows the FDA to approve a drug based on surrogate endpoints that predict clinical benefits rather than waiting for more traditional outcomes like overall survival. This pathway is often used for drugs treating life-threatening diseases such as cancers or rare genetic disorders. Post-approval trials are typically required to confirm the predicted clinical benefits.
Priority Review
When a drug shows significant therapeutic potential over existing treatments, it may qualify for priority review. Under this program, the FDA commits to reviewing the drug application within six months instead of the standard ten months, expediting access to treatments for patients in need.
Post-Market Surveillance
After a drug is approved and enters the market, the FDA continues to monitor its safety and effectiveness through post-market surveillance. This involves:
- Adverse Event Reporting: Healthcare providers and patients are encouraged to report adverse reactions to the FDA’s MedWatch program. This helps identify rare or long-term side effects that may not have appeared in clinical trials.
- Phase IV Clinical Trials: These are post-approval studies designed to gather additional information about the drug’s long-term effects, optimal use, and safety in the general population. Phase IV trials are often required for drugs that received accelerated approval.
- Risk Evaluation and Mitigation Strategies (REMS): For drugs with significant safety risks, REMS may include requirements such as additional labelling, restricted distribution, or patient monitoring programs.
Challenges in IND and Drug Development
The IND process is a critical gateway in drug development, but it is also fraught with challenges that can slow down or halt progress. These challenges can range from scientific obstacles to regulatory and financial hurdles.
Scientific Challenges
Developing a new drug is an inherently risky and complex process. Many investigational drugs fail to progress past the preclinical or early clinical stages due to unexpected toxicity or a lack of efficacy. Even drugs that show promise in animal models may not translate well to human clinical trials.
Moreover, biological variability in human populations can present difficulties in demonstrating consistent results, especially in smaller trials. This variability must be carefully managed through study design and statistical analysis.
Regulatory Challenges
The FDA’s stringent requirements for safety and efficacy mean that sponsors must provide comprehensive and compelling evidence. Regulatory delays can occur if the submitted data is incomplete or if the trial design fails to meet the FDA’s standards. Moreover, responding to FDA requests for additional data or addressing clinical holds can introduce delays that affect the overall timeline for drug development.
Financial Challenges
The cost of drug development is notoriously high, with estimates suggesting that it can take over $1 billion to bring a new drug to market. Funding must cover not only the research and development but also the manufacturing, regulatory submissions, and post-approval activities. Smaller companies or academic investigators may face financial barriers that hinder their ability to navigate the lengthy IND process.
The Global Perspective: INDs Beyond the US.
While the US IND process is regulated by the FDA, other countries have their own equivalent processes for authorising investigational drugs. For example:
- European Union: In the EU, investigational drugs must receive approval from the European Medicines Agency (EMA) under the Clinical Trial Application (CTA) process. The CTA is similar to the IND in that it requires comprehensive preclinical data, clinical trial protocols, and manufacturing information.
- United Kingdom: In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) oversees the approval of clinical trials involving investigational drugs. Sponsors must submit a Clinical Trial Authorisation (CTA) to the MHRA.
- Japan: In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) is responsible for regulating clinical trials. Sponsors must submit a Clinical Trial Notification (CTN) to the PMDA before initiating human trials.
Each country has its own set of regulations and requirements, but the principles of ensuring drug safety and efficacy before human exposure remain universal. Sponsors aiming to conduct global clinical trials must navigate multiple regulatory frameworks, which can complicate the IND submission process.
Conclusion
The Investigational New Drug (IND) application is a cornerstone of drug development in the US, serving as a gateway to human clinical trials. Through the IND process, the FDA ensures that investigational drugs are subjected to rigorous safety and efficacy evaluations before they reach the market. By allowing sponsors to test new drugs in human participants, the IND process accelerates medical innovation while protecting patient safety.
Navigating the IND submission process is a complex task that requires careful preparation, scientific diligence, and close attention to regulatory requirements. However, the rewards for successful IND submissions can be transformative, potentially leading to the development of new therapies that improve and save lives.
From initial preclinical studies to post-market surveillance, the journey of a drug through the IND process is one of the most demanding yet vital endeavours in pharmaceutical science. The ultimate goal is to ensure that new drugs reach the patients who need them, with the assurance that they have been rigorously tested for safety and effectiveness.
Q&A: Understanding the Investigational New Drug (IND) Application
Q1: What is an Investigational New Drug (IND) Application?
An Investigational New Drug (IND) application is a formal request submitted to the US Food and Drug Administration (FDA) to gain approval for testing a new drug or biological product in humans through clinical trials. This step is essential before any human subject can receive the investigational drug, ensuring the safety and proper regulation of the study.
Q2: Why is an IND application necessary?
An IND application is necessary to protect human participants in clinical trials and to ensure the investigational drug has undergone adequate preclinical testing to demonstrate a reasonable expectation of safety. It also ensures that the study will be scientifically and ethically conducted under FDA oversight.
Q3: What are the key components of an IND application?
An IND application consists of three main components:
- Preclinical Data: Evidence from laboratory and animal studies that show the investigational drug is safe for human testing.
- Clinical Trial Protocols: Detailed plans for how the clinical trials will be conducted, including study design, patient selection, dosing, and safety monitoring.
- Chemistry, Manufacturing, and Control (CMC) Information: Information about how the drug is made, its composition, and how its quality and consistency will be maintained during clinical trials.
Q4: Who can submit an IND application?
An IND application can be submitted by a variety of sponsors, including pharmaceutical companies, biotechnology firms, academic researchers, or individual investigators. There are different types of INDs depending on the nature and goals of the trial, such as Commercial INDs, Investigator-Initiated INDs, Treatment INDs, and Emergency Use INDs.
Q5: What are the different types of IND applications?
There are four main types of IND applications:
- Commercial IND: Submitted by pharmaceutical companies aiming to develop a drug for marketing.
- Investigator-Initiated IND: Submitted by individual researchers or academic institutions conducting their own clinical studies.
- Treatment IND: Allows the use of an investigational drug for patients with serious or life-threatening conditions who are not part of clinical trials.
- Emergency Use IND: Used when an investigational drug is needed in an emergency and there is no time for a standard IND review.
Q6: How long does the FDA take to review an IND application?
The FDA has 30 days to review an IND application after submission. During this time, experts assess the safety, design, and manufacturing information provided. If the application meets the requirements, the trial can proceed. However, the FDA can place the trial on hold if they have concerns about safety or other aspects of the study.
Q7: What happens after the FDA approves an IND?
Once the IND is approved, the sponsor can begin clinical trials in human subjects. The trial is typically conducted in phases:
- Phase I: Focuses on safety and dosage in a small group of participants.
- Phase II: Examines efficacy and side effects in a larger patient group.
- Phase III: Involves large-scale testing to confirm effectiveness, monitor side effects, and gather more data on safety.
Q8: What role does the Institutional Review Board (IRB) play in the IND process?
The Institutional Review Board (IRB) is an independent body that reviews and approves clinical trial protocols to ensure the rights, safety, and welfare of human participants are protected. IRB approval is required before any clinical trial can begin, in addition to FDA approval.
Q9: What is Good Manufacturing Practice (GMP), and why is it important for an IND?
Good Manufacturing Practice (GMP) refers to regulations that ensure the quality and safety of drugs throughout the manufacturing process. For an IND, the sponsor must demonstrate that the investigational drug is produced in compliance with GMP to ensure that it can be manufactured reliably and safely during the clinical trials.
Q10: What happens if an investigational drug shows serious adverse effects during a clinical trial?
If a clinical trial reveals serious or unexpected adverse effects, the sponsor must report these incidents to the FDA through Investigational New Drug Safety Reports. The FDA may decide to halt the trial, modify the protocol, or implement additional safety measures to protect participants.
Q11: What is expanded access (compassionate use), and how does it relate to an IND?
Expanded access, or compassionate use, allows patients with serious or life-threatening conditions to receive investigational drugs outside of clinical trials when no satisfactory treatments are available. Sponsors must submit an IND for expanded access, and the FDA must approve the use based on the drug’s potential benefits and risks.
Q12: What are the requirements for a New Drug Application (NDA) after completing clinical trials?
Once clinical trials are successfully completed, sponsors submit a New Drug Application (NDA) to seek FDA approval for marketing the drug. The NDA includes all preclinical and clinical data, information on the drug’s manufacturing, proposed labelling, and evidence that the drug is safe and effective for its intended use.
Q13: What is accelerated approval, and how does it expedite drug development?
Accelerated approval allows the FDA to approve drugs based on early evidence (such as surrogate endpoints) that suggests a clinical benefit, especially for life-threatening conditions. This pathway speeds up the availability of promising drugs while requiring further post-approval studies to confirm their benefits.
Q14: How does the FDA monitor drug safety after approval?
After a drug is approved, the FDA continues to monitor its safety through post-market surveillance. This includes adverse event reporting, Phase IV clinical trials, and, in some cases, Risk Evaluation and Mitigation Strategies (REMS) to ensure that the drug’s benefits continue to outweigh the risks in the general population.
Q15: What are the main challenges in the IND process and drug development?
Key challenges in the IND process include:
- Scientific Challenges: Many investigational drugs fail in clinical trials due to unexpected toxicity or lack of efficacy.
- Regulatory Challenges: Sponsors must navigate stringent FDA requirements and respond to clinical holds or requests for additional information.
- Financial Challenges: Drug development is expensive, often costing over $1 billion to bring a drug to market, which can be a barrier for smaller companies or academic researchers.
Q16: How does the IND process differ in other countries?
Different countries have their own regulatory processes for investigational drugs. For example:
- European Union: The Clinical Trial Application (CTA) is submitted to the European Medicines Agency (EMA).
- United Kingdom: The Medicines and Healthcare products Regulatory Agency (MHRA) oversees Clinical Trial Authorisation (CTA).
- Japan: The Pharmaceuticals and Medical Devices Agency (PMDA) manages Clinical Trial Notification (CTN) submissions. While the regulations vary, the core principles of ensuring drug safety and efficacy before human trials are universal across regulatory bodies.
Q17: How does an Emergency Use IND work?
An Emergency Use IND allows a drug to be used in a life-threatening situation where no standard treatment is available, and there isn’t enough time to submit a formal IND. This IND is often granted in urgent cases where quick access to a drug may save lives.
Q18: What is the difference between a Commercial IND and an Investigator-Initiated IND?
A Commercial IND is submitted by a pharmaceutical or biotechnology company intending to market the drug after clinical trials. An Investigator-Initiated IND, on the other hand, is submitted by an independent researcher or academic institution conducting clinical trials, often to study new uses for existing drugs rather than for commercial purposes.
Q19: What role does patient safety play in the IND process?
Patient safety is paramount throughout the IND process. From preclinical testing to post-market surveillance, every step is designed to minimise risks and ensure that investigational drugs are tested under safe and ethical conditions. The FDA and IRB review clinical trial protocols to safeguard participants and adverse events are closely monitored to protect patient welfare.
Q20: How do expanded access programs benefit patients?
Expanded access programs allow patients with serious conditions to receive investigational drugs when no other treatments are available. These programs provide potential life-saving benefits to patients who cannot participate in clinical trials, offering hope and treatment options when traditional therapies are not sufficient.
Disclaimer
The content provided in this article is for informational purposes only and is not intended as legal, regulatory, or medical advice. While every effort has been made to ensure the accuracy and currency of the information presented, Open Medscience makes no warranties or representations as to its completeness or suitability for any particular purpose. Readers are advised to consult the US Food and Drug Administration (FDA) or other qualified professionals for guidance on specific regulatory requirements or clinical decisions. The views expressed in this article do not necessarily reflect those of regulatory authorities or other institutions referenced.
home » blog » regulatory affairs »