Summary: Medical imaging stands on the cusp of a revolutionary change, driven by rapid advancements in artificial intelligence, data interoperability, sensor technologies, and patient-centric innovations. By 2025, radiological departments will see diagnostics refined with unprecedented detail, merging high-resolution modalities with real-time data analysis. This transformation will empower clinicians with sharper tools to detect, diagnose, and treat conditions far more accurately and earlier than ever before. Patients will become active participants in their healthcare journey, benefiting from personalised imaging plans, safer radiation doses, and more accessible imaging platforms. As we approach 2025, the focus shifts towards patient-centred outcomes, streamlined workflows, better training for radiologists, and rigorous data security standards, all culminating in an era where imaging guides precision medicine and improves population health worldwide.
Keywords: Medical Imaging; Precision Medicine; Artificial Intelligence; Radiology Workflows; Data Interoperability; Personalised Healthcare.
Introduction: A Revolution in Sight
Medical imaging has always been at the heart of diagnostic medicine, illuminating the hidden recesses of the human body to guide effective treatment. Historically, the field was defined by modalities such as X-rays, CT scans, and MRI, each one offering clinicians unique insights. Over the last two decades, imaging technologies have evolved swiftly, improving detail, reducing invasiveness, and speeding up turnaround times. Now, as we look to 2025, the sector stands poised to enter an era of transformative innovation, where cutting-edge technologies and integrated data systems converge. Rather than merely observing the body, new imaging techniques will enable a deeper understanding of physiological processes, refining diagnoses with pinpoint accuracy.
This imminent metamorphosis is driven by key factors. Advances in sensor design, the maturation of artificial intelligence (AI) and machine learning algorithms, the increasing availability of high-quality imaging datasets, and growing emphasis on patient-centric care are all contributing to a richer landscape. Radiologists and imaging technicians will have at their disposal advanced tools that integrate seamlessly into their workflow, enabling them to offer more nuanced interpretations. Patients will benefit from clearer explanations, more timely diagnoses, and better-informed treatment pathways. Ultimately, the future of medical imaging promises to reshape the very notion of what is possible in healthcare.
Setting the Stage: Medical Imaging’s Evolution
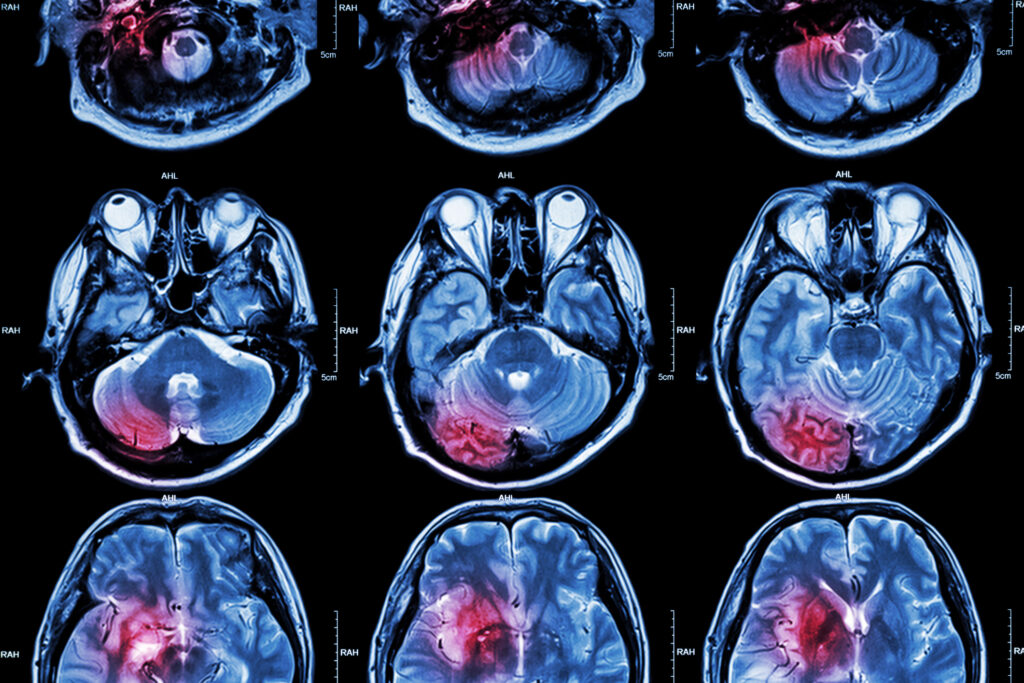
Before looking to 2025, it is worth remembering how far medical imaging has come. Early imaging techniques were largely limited to planar X-rays, helpful but crude by today’s standards. The introduction of computed tomography (CT) and magnetic resonance imaging (MRI) in the late 20th century allowed for more detailed, cross-sectional views of the body, ushering in a new era of diagnosis. Ultrasound technology contributed real-time views inside the body without harmful ionising radiation. Nuclear medicine imaging, including PET scans, illuminated metabolic processes, giving clinicians insights into conditions such as cancer at a molecular level.
In recent years, these modalities have been refined further. MRI machines have grown stronger, producing remarkably detailed anatomical images. CT scans have become faster and more accurate, reducing patient exposure to radiation. New hybrid modalities, like PET/MRI, have allowed for simultaneous imaging of structure and function. The digital revolution has brought powerful post-processing tools, enabling radiologists to manipulate and enhance images for clearer interpretations.
By 2025, these incremental improvements will coalesce into a holistic upgrade. We will see not just improved hardware, but also the seamless integration of software platforms, AI-driven analysis, and interoperable data systems that make image sharing and interpretation more collaborative than ever.
Artificial Intelligence Redefining Diagnostic Accuracy by 2025
AI will play a pivotal role in shaping the future of medical imaging. Radiology departments already use machine learning models to detect fractures or early cancers. By 2025, these models will become even more robust and refined, capable of detecting subtle patterns that human eyes might miss. AI algorithms will not only highlight abnormalities but also suggest potential diagnoses and probabilities, vastly improving radiologists’ confidence.
Natural language processing (NLP) will streamline the reporting process, automatically generating structured reports based on the findings identified by AI. This will save clinicians time and reduce errors that arise from tedious manual documentation. In addition, advanced machine learning techniques will compare patient scans against extensive databases of previously diagnosed cases, providing radiologists with instant access to population-level insights and trends.
AI’s influence will extend to personalised medicine too. Algorithms will predict a patient’s likely response to specific treatments, guiding decisions about the best course of action. By integrating imaging data with genomic and proteomic information, clinicians will tailor interventions to individual patient profiles. Through these synergies, medical imaging in 2025 will be not just about “seeing more,” but about interpreting images in a richer, more meaningful context.
Precision Imaging: Detecting the Undetectable
As hardware and software advances coalesce, the ability to detect faint traces of disease will increase markedly. Today’s imaging can show tumours down to millimetre scales, but by 2025, improved resolution may push boundaries even further. Ultrafast MRI sequences and advanced CT detectors will allow visualisation of subtle tissue changes far earlier in a disease’s progression.
Functional imaging, such as diffusion-weighted MRI or dynamic contrast-enhanced ultrasound, will help clinicians differentiate between aggressive and indolent tumours more accurately. Molecular imaging agents, tagged with specific biomarkers, will bind to cancer cells, lighting them up in ways previously unimaginable. This enhanced specificity will allow treatments to be timed and targeted with tremendous precision, sparing healthy tissue and improving patient outcomes.
This level of granularity will extend beyond oncology. Neurological conditions, for example, could be diagnosed earlier by detecting minute structural or functional anomalies in the brain. Heart disease might be intercepted before a major cardiac event occurs, as imaging reveals early plaque formation or subtle changes in myocardial perfusion. By detecting the undetectable, imaging in 2025 will shift the healthcare paradigm from reactive treatment to proactive prevention.
Enhanced Patient Experience and Safety
Medical imaging has not always prioritised patient comfort. Lengthy MRI scans, uncomfortable positions, or claustrophobic environments are common complaints. By 2025, patient experience will take centre stage. Advances in scanner design, such as wider MRI bores and quieter sequences, will improve comfort. More portable imaging devices will allow certain scans to be performed at the bedside, reducing the need for patient transport within hospitals.
Patient safety will also improve as imaging protocols become more refined. Lower-dose CT scans and more judicious use of contrast agents will minimise risks. AI-driven dose optimisation software will ensure each patient receives the minimal necessary radiation, without compromising image quality. Through these improvements, patients will feel more at ease and more engaged with their imaging experiences, removing a significant barrier to timely and regular scans.
In addition, patients will have easier access to their imaging data. Secure patient portals and mobile apps will allow individuals to view their scans, read simplified reports, and gain a clearer understanding of their diagnosis. Greater transparency builds trust and encourages patients to participate more fully in their healthcare journey. By 2025, imaging will not just inform physicians—it will empower patients.
The Future of Medical Imaging for 2025: Integrated and Interoperable Systems
One of the most exciting developments by 2025 will be the integration of imaging platforms into broader healthcare ecosystems. Historically, imaging data often lived in silos, accessible only to radiology departments or specialists. In the near future, interoperable data systems will allow images and reports to flow seamlessly across electronic health records (EHRs), enabling surgeons, oncologists, and general practitioners to view and act on imaging findings promptly.
Interoperability will also facilitate more effective multidisciplinary team meetings. Oncologists, for instance, will no longer need to schedule separate imaging reviews; they will access scans in real-time, comparing them side-by-side with laboratory results, pathology data, and genomics. This integrated approach will streamline diagnosis and treatment decision-making, reducing delays and improving patient outcomes.
Cloud-based storage solutions and advanced cybersecurity measures will support this connectivity. Secure data exchange protocols will ensure that patient confidentiality is maintained while enabling frictionless collaboration. Thus, medical imaging in 2025 will not be a stand-alone process but part of a fluid, dynamic ecosystem working towards holistic patient care.
Virtual Reality, Augmented Reality, and Beyond
New visualisation techniques will revolutionise how clinicians interact with imaging data. By 2025, many healthcare professionals will rely on virtual reality (VR) and augmented reality (AR) tools to interpret scans. Instead of viewing static 2D slices, radiologists and surgeons will immerse themselves in three-dimensional reconstructions of organs and tissues. They will interact with these digital models, rotating and dissecting them virtually to understand complex anatomies more thoroughly.
AR overlays in the operating theatre will guide surgeons with precision. For instance, a surgeon performing a tricky liver resection could wear AR goggles displaying a patient’s anatomical landmarks extracted from pre-operative scans. This enhances accuracy and reduces the risk of complications. Such innovations will narrow the gap between imaging and treatment, making it a continuous process rather than separate, discrete steps.
VR-based training modules will also accelerate the learning curve for new radiologists. Trainees can practise interpreting images in a simulated environment, with immediate feedback. By experiencing a range of cases virtually, they will quickly gain the competence and confidence needed to excel in real-life scenarios. Through VR and AR, imaging data will leap off the screen and into the hands of clinicians, enriching their understanding and enabling safer, more precise interventions.
Data Security, Ethics, and Regulation
With great technological power comes a heightened responsibility for data security and ethical governance. By 2025, medical imaging will produce even more data—high-resolution images, functional maps, and AI-generated insights. Storing and transmitting these datasets securely is paramount to maintain patient confidentiality.
Regulatory bodies will step in to set standards. Guidelines on AI algorithm validation, bias detection, and interpretability will be established to ensure that automated decision-support tools are reliable and equitable. Imaging professionals will need to be versed not only in technology but also in the ethical frameworks that govern its use. Questions such as how much autonomy to grant AI, how to safeguard against biased datasets, and how to handle incidental findings will shape policies and protocols.
Increased transparency will be a hallmark of this era. Patients will expect to know how their data is used and protected. Hospitals and imaging centres will need clear data governance policies, and audit trails will monitor who accesses imaging records and for what purpose. Robust encryption, decentralised storage solutions, and blockchain-based verification may become commonplace as imaging data becomes a valuable commodity in personalised healthcare ecosystems.
Empowering the Radiology Workforce
The radiology workforce will not vanish in the face of AI and automation. On the contrary, by 2025, radiologists will be more important than ever, their roles evolving into those of data interpreters, team leaders, and healthcare strategists. While AI handles routine tasks such as identifying common pathologies, human professionals will focus on complex cases, correlating imaging findings with clinical and laboratory data, and making nuanced judgments that machines cannot replicate.
Training for the next generation of radiologists and imaging technicians will emphasise digital literacy, data science principles, and the interpretation of AI outputs. Radiologists will learn how to validate the suggestions offered by machine learning models, ensuring that patient care is guided by the best of human and artificial intelligence combined.
This shift in focus will also improve job satisfaction. Freed from the repetitive drudgery of sifting through thousands of images, radiologists can concentrate on challenging cases that demand critical thinking. They will become active participants in multidisciplinary teams, helping to shape treatment plans and follow-up strategies. In an era defined by advanced imaging and AI, the human element—compassion, intuition, and clinical experience—will remain irreplaceable.
Democratising Access to Imaging
As technology advances and costs drop, one of the most significant changes by 2025 will be the democratisation of imaging access. Lower-cost, portable imaging devices can be deployed in rural clinics or mobile screening units, bringing quality diagnostic services to underserved populations. Tele-radiology services, bolstered by reliable high-speed connectivity and cloud-based image sharing, will enable patients in remote areas to benefit from the expertise of top radiologists thousands of miles away.
This broader access will improve public health outcomes. Early detection programmes for cancer, heart disease, and other conditions can be implemented more widely. Screening initiatives can be extended to communities that previously lacked the necessary infrastructure. With AI-powered triage, even basic imaging centres can flag suspicious findings and refer patients to specialist facilities for further investigation.
By 2025, medical imaging will no longer be the privilege of well-resourced urban hospitals. Instead, it will be a cornerstone of equitable healthcare, ensuring that all patients, regardless of geography or socioeconomic status, can benefit from timely and accurate diagnostics. This shift promises a more inclusive approach to healthcare, where imaging contributes to reducing disparities rather than reinforcing them.
A Catalyst for Preventive and Precision Medicine
Modern healthcare is moving from a reactive model towards a proactive, preventive approach. Medical imaging will be central to this transition by 2025. Instead of waiting for symptoms to manifest, imaging could be part of routine check-ups, catching conditions at their earliest stages. Annual low-dose CT scans might identify nodules that, left unchecked, could become malignant tumours. Regular cardiac imaging could alert clinicians to evolving risk factors, prompting lifestyle interventions or early treatments.
The integration of imaging data with other patient information—genetic markers, lifestyle data from wearable devices, electronic health records—will enable clinicians to practise true precision medicine. They can identify patient subgroups that benefit most from a particular intervention, adjusting treatment protocols for optimal results. Over time, this personalised approach will reduce healthcare costs, lessen the burden of chronic diseases, and improve life expectancy.
As we approach 2025, the line between diagnosis and prevention will blur. Imaging will not simply confirm that a disease is present; it will highlight vulnerabilities, predict trajectories, and guide targeted interventions. This shift in perspective will transform healthcare from a reactive enterprise into a proactive force that saves lives and enhances quality of life.
Looking Beyond 2025: The Road Ahead
By 2025, medical imaging will have made enormous strides, yet it will still be evolving. Technologies that seem cutting-edge today—like AI-based diagnostics or AR-guided surgeries—may become commonplace. Subsequent years will bring deeper integration with nanotechnology, allowing imaging at the cellular or even molecular level. Gene-editing tools, immunotherapies, and novel pharmaceuticals will be complemented by imaging techniques that track how these interventions shape the body over time.
Global collaboration will accelerate innovation. Researchers from around the world will share imaging data sets to refine AI models, study rare conditions, and develop unified standards. International regulatory bodies will harmonise guidelines, ensuring that new imaging technologies reach the market smoothly and benefit patients everywhere.
The ultimate goal remains the same: to improve patient outcomes and advance healthcare. By guiding early detection, informing better treatments, enhancing patient comfort, and promoting equitable access, medical imaging will be a linchpin of modern medicine. The year 2025 will be a milestone, a snapshot in a much larger journey, as imaging continually transforms to illuminate the human body in ever more intricate and meaningful ways.
Conclusion: A Clearer, Brighter Vision
As we approach 2025, medical imaging is on track to achieve remarkable feats. AI and data science will amplify diagnostic accuracy, new imaging modalities will reveal subtle changes at the earliest stage, and VR/AR tools will revolutionise how clinicians interact with data. Patients will become active participants, with easier access to their images, clearer explanations, and a greater say in their healthcare decisions. Interoperability, ethical standards, and robust data security frameworks will ensure that these advancements unfold responsibly.
The future of medical imaging promises not just sharper images, but deeper insights. By 2025, imaging will no longer be confined to diagnostic snapshots; it will actively guide therapy, prevent diseases, and personalise treatments. As technology and human expertise unite, the field will continue to evolve, delivering a more equitable, efficient, and patient-centric approach to healthcare. The road ahead may be complex, but the vision has never been clearer.
Disclaimer:
The content of this article is intended for informational purposes only and does not constitute professional medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy of the information presented, Open Medscience makes no guarantees regarding the completeness, timeliness, or applicability of any data, predictions, or opinions expressed. Developments in medical imaging and related technologies are evolving rapidly, and projections for 2025 should be viewed as indicative rather than definitive.
Readers should consult qualified healthcare professionals for advice relating to their specific medical conditions or imaging needs. References to emerging technologies, clinical practices, or regulatory expectations are speculative and may not reflect future standards or outcomes. Open Medscience does not accept liability for any loss or harm arising from reliance on the content provided herein.
You are here: home » diagnostic medical imaging blog »