Summary: Access to high-quality lung imaging has long been a challenge across the world. Traditional high-field MRI systems are expensive, complex to maintain, and not always suited to imaging the lungs due to low proton density and respiratory motion. A new generation of low-field MRI scanners, powered by powerful artificial intelligence (AI), is now rewriting that story. By combining lower costs, simplified infrastructure, and AI-driven image reconstruction, these scanners are making lung MRI more accessible than ever. This breakthrough could bring high-quality, radiation-free imaging to community clinics, rural hospitals, and developing healthcare systems, enabling earlier diagnosis and better monitoring of lung disease.
Keywords: low-field MRI, AI-enhanced reconstruction, lung MRI accessibility, hyperpolarised gas imaging, cost-effective MRI, clinical adoption
Low-field MRI
Low-field MRI refers to imaging systems operating at magnetic field strengths significantly lower than traditional machines. While conventional scanners use fields of 1.5 T or 3 T, low-field systems can function effectively below 1 T. Historically, this was considered a limitation because lower magnetic fields meant weaker signals and reduced image clarity. However, the landscape is changing. Advances in magnet design, electronics, and image processing have revitalised the potential of low-field MRI.
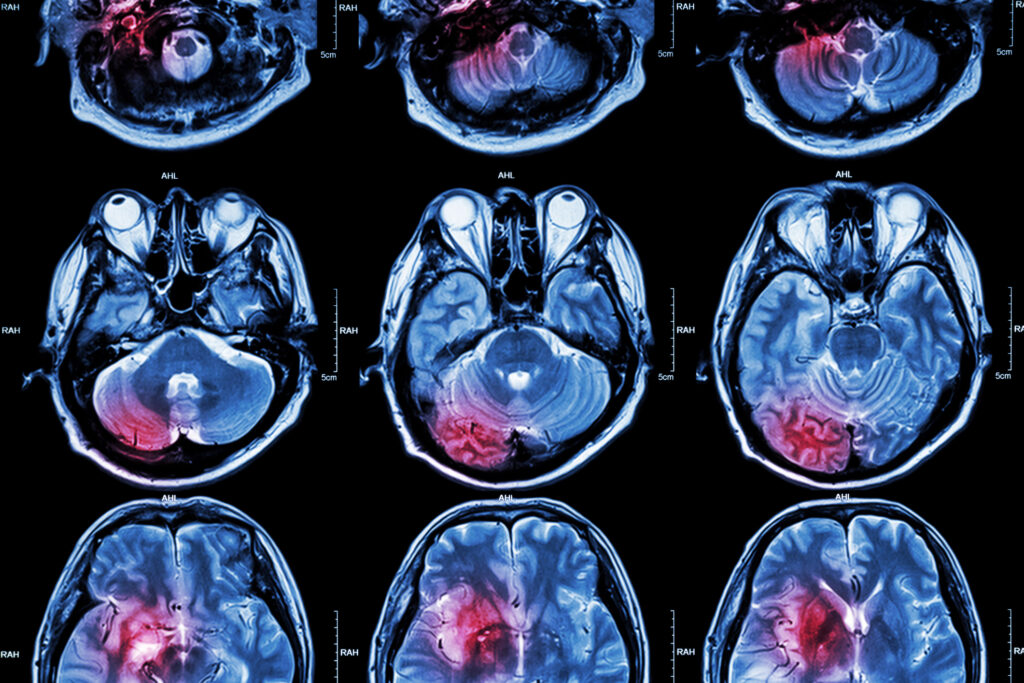
For lung imaging, this shift is particularly significant. The lungs contain a large volume of air, making proton signals weak and uneven. High-field MRI struggles to capture precise details of lung tissue, often ceding ground to CT scans. Low-field MRI, on the other hand, is less sensitive to artefacts caused by magnetic susceptibility differences between air and tissue. When paired with intelligent reconstruction software, low-field systems can now produce diagnostic images suitable for respiratory conditions, and at a fraction of the traditional cost.
AI-enhanced image reconstruction
Artificial intelligence is the crucial partner in this technological transformation. Using deep learning, AI systems can process low-field images and enhance them to match the quality of high-field images. Neural networks trained on thousands of high-field and low-field image pairs learn to “fill in” missing detail, sharpen contrast, and suppress noise.
This process, known as AI-enhanced reconstruction, allows radiologists to see clearer anatomical features even when raw scanner data appears blurry or underexposed. In practical terms, AI closes the quality gap between low- and high-field MRI, turning smaller, cheaper machines into clinically capable tools. For lung imaging, AI also helps compensate for breathing motion and the low signal-to-noise ratio typical of pulmonary scans, delivering sharp, consistent results without the need for more powerful magnets.
Lung MRI accessibility
Making lung MRI more accessible means taking advanced imaging out of specialist centres and into everyday healthcare. Traditional MRI machines are heavy, costly, and require rooms with specific magnetic shielding, cooling systems, and stable power supplies. Low-field MRI removes many of these barriers. Smaller magnets mean lighter machines, reduced helium use, and less stringent siting requirements.
This opens the door to widespread deployment in local hospitals, outpatient clinics, and even mobile scanning units. In settings where CT has been the only viable imaging method, low-field MRI now offers a radiation-free alternative that can visualise lung structure and function. The implications are enormous: shorter waiting times, earlier disease detection, and improved access for people living far from major cities. By democratising MRI access, low-field scanners could fundamentally reshape pulmonary diagnostics and long-term respiratory care.
Hyperpolarised gas lung imaging
A fascinating frontier in this field is hyperpolarised gas imaging. This innovative technique uses specially prepared gases such as xenon-129, which the patient inhales before the scan. The gas acts as a tracer, allowing MRI to visualise how air moves through the lungs and where it interacts with blood flow for gas exchange.
In combination with low-field MRI and AI reconstruction, hyperpolarised gas imaging can reveal detailed ventilation maps of the lungs, showing well-functioning areas and those affected by disease. It provides functional information that complements structural imaging, giving clinicians a clearer understanding of how lung disease impacts airflow and oxygen transfer. Importantly, all of this is achieved without exposure to ionising radiation—making it safer for patients who require repeated monitoring, such as those with asthma, COPD, or interstitial lung disease.
Cost-effective MRI deployment
The cost of traditional MRI has been one of the biggest obstacles to broader use in healthcare. High-field systems require specialised rooms, heavy cooling systems, and continuous maintenance—costing hospitals millions in setup and running expenses. Low-field MRI breaks this cycle by offering comparable diagnostic capability with far less overhead.
Because low-field machines consume less power and often operate without liquid helium, they can be installed in smaller facilities without extensive infrastructure upgrades. They also take up less space and require simpler shielding. This means hospitals can install multiple units across regions rather than relying on a single large scanner in a central hub. For national healthcare systems, it’s a chance to expand imaging capacity, shorten waiting lists, and reduce the overall cost per scan.
AI integration enhances this economic advantage further. By improving image quality in real time, AI reduces the need for repeat scans and shortens the time needed for each patient. Together, these efficiencies make the prospect of nationwide low-field MRI deployment both achievable and sustainable.
Clinical adoption of low-field systems
The transition from promising research to everyday clinical reality is now underway. Hospitals and imaging centres are testing low-field AI-enhanced MRI systems in pilot studies, with results showing comparable diagnostic value to high-field systems in key areas such as brain, musculoskeletal, and lung imaging.
For successful adoption, healthcare professionals must gain confidence that these systems deliver reliable, repeatable results. Radiologists are learning how to interpret AI-enhanced images and adapt reporting workflows to accommodate them. Manufacturers, meanwhile, are working towards regulatory approval, ensuring that low-field MRI meets safety and performance standards.
Training and education will play a key role. Radiographers need to understand the subtleties of low-field scanning, such as patient positioning and sequence optimisation, while clinicians must learn to integrate functional data—such as that from hyperpolarised gas imaging—into clinical decision-making. As evidence grows, the medical community is increasingly viewing low-field AI-enhanced MRI as a serious, cost-effective complement to CT and high-field MRI in the respiratory diagnostic toolkit.
Conclusion
The combination of low-field MRI and AI-driven enhancement represents a bold step towards accessible, affordable, and high-quality lung imaging. What once required a large, costly, high-field scanner can now be achieved using smaller, more innovative technology. Add the capabilities of hyperpolarised gas imaging, and clinicians gain a unique view into lung function—without the risks of radiation.
This shift could transform how healthcare systems deliver imaging, from speeding up diagnosis to improving management of chronic respiratory diseases. For patients, it means earlier intervention, safer follow-up scans, and easier access to advanced diagnostics, no matter where they live. Low-field AI-enhanced MRI isn’t just a new tool—it’s a reimagining of what medical imaging can be: accessible, intelligent, and patient-centred.
Q and A
Q1: Why has lung MRI traditionally been difficult?
A1: The lungs have very low proton density because they’re filled with air rather than soft tissue. This makes it hard for MRI to capture strong signals. Breathing motion and air-tissue interfaces also create artefacts that reduce image clarity.
Q2: How does AI help low-field MRI scanners produce clear images?
A2: AI algorithms trained on high-quality data can reconstruct low-field images by enhancing contrast, removing noise, and sharpening detail. This allows images from smaller magnets to reach near high-field quality levels suitable for diagnosis.
Q3: What advantages does low-field MRI have over CT?
A3: Unlike CT, MRI doesn’t use ionising radiation, making it safer for repeated scans. Low-field systems are also cheaper to install and operate, expanding access to safe imaging for long-term monitoring of lung diseases.
Q4: What is hyperpolarised gas imaging, and why is it important?
A4: It’s a technique where patients inhale polarised xenon gas before an MRI. The gas allows imaging of how air moves through the lungs and how efficiently oxygen exchange occurs—something not visible on standard scans.
Q5: Could low-field MRI replace high-field systems entirely?
A5: Not completely. High-field MRI remains essential for detailed brain, cardiac, and musculoskeletal imaging. Low-field systems complement them by offering affordable, accessible scanning options—especially for lungs and in areas with limited resources.
Q6: How soon could patients benefit from AI-enhanced low-field lung MRI?
A6: Pilot installations and early clinical studies are already underway. As more evidence accumulates and regulatory approvals progress, widespread clinical adoption could happen within the next few years, starting in community and regional hospitals.
Disclaimer
The information provided in this article is intended for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment. Readers should consult qualified healthcare professionals for guidance regarding specific medical conditions or imaging options. Open MedScience and its contributors make no representations or warranties regarding the accuracy, completeness, or applicability of the content to individual circumstances.