The article explores the biological principles of Targeted Radionuclide Therapy (TRT) for cancer. This innovative approach precisely delivers radioactive isotopes to tumour cells, thereby maximising therapeutic effects while minimising damage to healthy tissues. TRT employs radionuclides such as alpha particles, beta particles, and gamma rays, each with distinct properties suited for different cancer treatment scenarios.
Key mechanisms of TRT include targeted delivery, radiation-induced cell damage, and the bystander effect. Targeted delivery involves conjugating radionuclides with molecules that bind to specific cancer cell markers. Radiation-induced cell damage occurs directly through DNA ionisation or indirectly via reactive oxygen species. The bystander effect extends the therapeutic impact to adjacent non-irradiated cells.
Biological factors like the tumour microenvironment, tumour heterogeneity, and cellular repair mechanisms influence TRT’s effectiveness. Strategies to enhance TRT include modulating the microenvironment, targeting multiple receptors, and inhibiting DNA repair pathways.
Clinical applications of TRT include treatments for neuroendocrine tumours, prostate cancer, and lymphoma, utilising well-defined targets such as somatostatin receptors, PSMA, and CD20. Prominent therapeutic agents include Lutetium-177-DOTATATE for neuroendocrine tumours, Lutetium-177-PSMA-617 for prostate cancer, and Iodine-131-rituximab for lymphoma.
Challenges in TRT include managing radiotoxicity, overcoming cancer cell resistance, and improving radionuclide delivery technologies. Innovations in dosimetry, combination therapies, and nanoparticle-based delivery systems are critical to addressing these challenges.
The article concludes by emphasising the potential of TRT to revolutionise cancer treatment through its targeted approach, driven by ongoing advancements in molecular biology, imaging, and nanotechnology. The future of TRT promises enhanced precision and effectiveness, offering new hope to cancer patients.
Introduction to Targeted Radionuclide Therapy for Cancer
Targeted radionuclide therapy (TRT) represents a burgeoning field in oncology. It provides a sophisticated approach to cancer treatment by delivering radioactive isotopes directly to tumour cells. This precision therapy aims to maximise the therapeutic effect on cancer cells while minimising damage to surrounding healthy tissue. This article explores the biological principles underpinning TRT, its mechanisms, and its clinical applications, offering a comprehensive understanding of this innovative treatment modality.
Understanding Radionuclides
Radionuclides are atoms with unstable nuclei that release energy in the form of radiation as they decay. These emissions can be in the form of alpha particles, beta particles, or gamma rays, each with distinct properties and implications for cancer therapy.
- Alpha Particles: These are heavy, positively charged particles with high energy but limited penetration, making them suitable for targeting small clusters of cancer cells without affecting nearby healthy tissues.
- Beta Particles: Lighter and more penetrating than alpha particles, beta particles can travel a few millimetres in tissue, making them ideal for targeting larger or more diffuse tumour masses.
- Gamma Rays: High-energy photons with significant penetration power, gamma rays are often used for imaging rather than direct treatment due to their potential to affect distant tissues.
Mechanisms of Action
TRT leverages the biological processes of cancer cells to deliver radionuclides precisely where they are needed. The primary mechanisms include:
1. Targeted Delivery
Targeted delivery relies on the unique biological markers or receptors overexpressed on cancer cells. Monoclonal antibodies, peptides, or small molecules designed to bind specifically to these markers are conjugated with radionuclides. Upon administration, these conjugates circulate through the bloodstream, binding selectively to cancer cells and delivering the radioactive payload directly to the tumour site.
2. Radiation-Induced Cell Damage
Once the radionuclides bind to the tumour cells, they emit radiation, damaging the cancerous DNA. This damage can be direct, through the ionisation of DNA molecules, or indirect, by generating reactive oxygen species (ROS) that further damage cellular components. The result is the inhibition of cellular replication and eventual cell death.
3. Bystander Effect
An intriguing aspect of TRT is the bystander effect, where non-irradiated cells adjacent to the targeted cancer cells also exhibit damage. This phenomenon occurs due to the release of signalling molecules from irradiated cells, spreading the therapeutic effect beyond the directly targeted cells.
Biological Considerations
1. Tumour Microenvironment
The tumour microenvironment plays a critical role in the effectiveness of TRT. Factors such as hypoxia, interstitial fluid pressure, and the presence of stromal cells can influence the distribution and uptake of radionuclide conjugates. Hypoxic regions with low oxygen levels can be particularly challenging as they are less responsive to radiation therapy. Strategies to modulate the microenvironment, such as normalising blood vessels or using hypoxia-activated prodrugs, can enhance TRT efficacy.
2. Tumour Heterogeneity
Tumour heterogeneity, the existence of diverse cancer cell populations within a single tumour, poses a significant challenge. Different cells may express varying levels of target receptors, affecting the uniformity of radionuclide delivery. Combination therapies that target multiple receptors or integrate TRT with other treatment modalities can address this heterogeneity, improving therapeutic outcomes.
3. Cellular Repair Mechanisms
Cancer cells, like all cells, have intrinsic repair mechanisms to counteract DNA damage. The efficiency of these repair mechanisms can influence the sensitivity of tumour cells to TRT. Inhibitors of DNA repair pathways, such as PARP inhibitors, can be used in conjunction with TRT to enhance its effectiveness by preventing cancer cells from repairing the radiation-induced damage.
Clinical Applications
TRT has shown promise in treating various cancers, particularly those with well-defined targets for radionuclide conjugates. Some notable applications include:
1. Neuroendocrine Tumours
Neuroendocrine tumours (NETs) often overexpress somatostatin receptors and have been successfully treated with somatostatin analogues conjugated with radionuclides like Lutetium-177. This approach, known as peptide receptor radionuclide therapy (PRRT), has demonstrated significant efficacy in controlling tumour growth and improving patient survival.
2. Prostate Cancer
Prostate-specific membrane antigen (PSMA) is a well-characterised target in prostate cancer. Radionuclide-labelled PSMA inhibitors, such as PSMA-617 conjugated with Lutetium-177, have shown promising results in treating metastatic castration-resistant prostate cancer (mCRPC), offering a new avenue for patients who have exhausted conventional therapies.
3. Lymphoma
CD20 is a common target in B-cell lymphomas. Radiolabelled anti-CD20 antibodies, such as Iodine-131-labelled rituximab, have been used to deliver targeted radiation to lymphoma cells. This approach has shown efficacy in both newly diagnosed and relapsed cases, providing an additional treatment option for patients.
Challenges and Future Directions
1. Radiotoxicity and Side Effects
While TRT aims to minimise damage to healthy tissues, radiotoxicity remains a concern. The radiation emitted by radionuclides can affect nearby normal cells, leading to side effects such as bone marrow suppression, renal toxicity, and gastrointestinal disturbances. Advances in dosimetry, the calculation of the absorbed radiation dose, are crucial to optimising treatment plans and minimising these side effects.
2. Resistance Mechanisms
Cancer cells can develop resistance to TRT through various mechanisms, such as downregulation of target receptors, activation of alternative signalling pathways, or enhanced DNA repair capabilities. Overcoming this resistance requires a multifaceted approach, including developing new radionuclide conjugates, combination therapies, and personalised treatment strategies based on the tumour’s molecular profile.
3. Innovations in Radionuclide Delivery
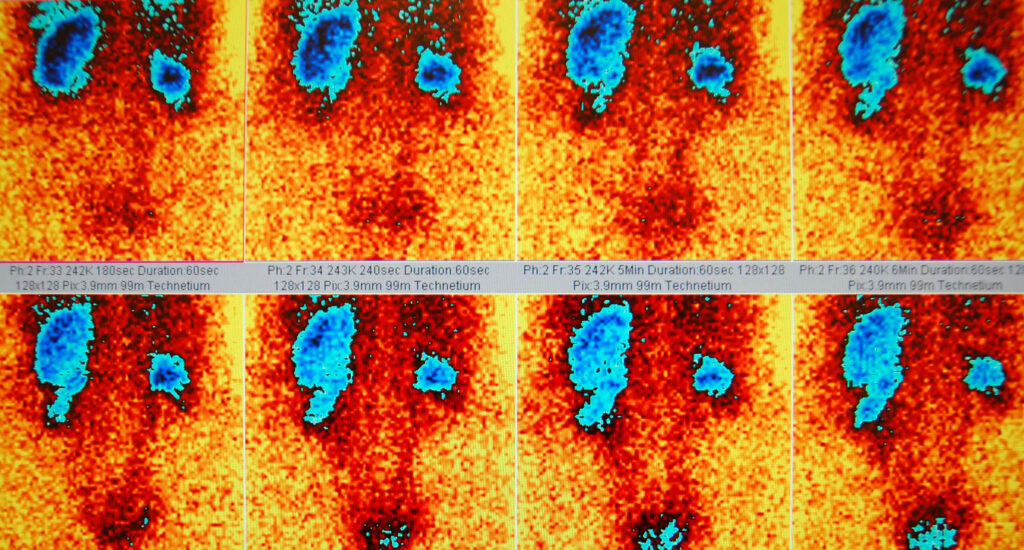
Emerging technologies are enhancing the precision and efficacy of radionuclide delivery. Nanoparticles, for instance, can be engineered to carry multiple radionuclides, drugs, or imaging agents, providing a multifunctional platform for cancer therapy. Advances in imaging techniques, such as positron emission tomography (PET) and single-photon emission computed tomography (SPECT), are also improving the ability to track radionuclide distribution and optimise treatment in real-time.
Conclusion
Targeted radionuclide therapy represents a paradigm shift in cancer treatment, offering a highly specific and effective approach to targeting malignant cells. By understanding the biological principles underlying TRT, clinicians can better harness its potential, addressing challenges and improving outcomes for patients. The continued evolution of this field, driven by innovations in molecular biology, imaging, and nanotechnology, promises to expand the horizons of cancer therapy, bringing new hope to those affected by this pervasive disease.
The table below outlines some key molecular targets for targeted radionuclide therapy (TRT), along with the associated radionuclides and cancer types:
| Molecular Target | Associated Radionuclide | Cancer Type | Therapeutic Agent |
| Somatostatin Receptors (SSTR) | Lutetium-177, Yttrium-90 | Neuroendocrine Tumours (NETs) | Lutetium-177-DOTATATE, Yttrium-90-DOTATOC |
| Prostate-Specific Membrane Antigen (PSMA) | Lutetium-177, Actinium-225 | Prostate Cancer | Lutetium-177-PSMA-617, Actinium-225-PSMA-617 |
| CD20 | Iodine-131, Yttrium-90 | B-cell Lymphomas | Iodine-131-rituximab, Yttrium-90-ibritumomab tiuxetan |
| HER2/neu | Lutetium-177, Copper-64 | Breast Cancer, Gastric Cancer | Lutetium-177-pertuzumab, Copper-64-trastuzumab |
| Glypican-3 (GPC3) | Yttrium-90, Lutetium-177 | Hepatocellular Carcinoma | Yttrium-90-YB-1, Lutetium-177-anti-GPC3 |
| CEA (Carcinoembryonic Antigen) | Iodine-131, Lutetium-177 | Colorectal Cancer, Pancreatic Cancer | Iodine-131-labetuzumab, Lutetium-177-labetuzumab |
| MUC1 | Lutetium-177, Technetium-99m | Breast Cancer, Ovarian Cancer | Lutetium-177-anti-MUC1, Technetium-99m-anti-MUC1 |
| Epidermal Growth Factor Receptor (EGFR) | Lutetium-177, Iodine-131 | Lung Cancer, Head and Neck Cancer | Lutetium-177-cetuximab, Iodine-131-cetuximab |
| Mesothelin | Actinium-225, Lutetium-177 | Mesothelioma, Pancreatic Cancer | Actinium-225-anti-mesothelin, Lutetium-177-anti-mesothelin |
| PSMA (Prostate-Specific Membrane Antigen) | Lutetium-177, Actinium-225 | Prostate Cancer | Lutetium-177-PSMA-617, Actinium-225-PSMA-617 |
Understanding Targeted Radionuclide Therapy for Cancer: A Q&A Guide
Q: What is Targeted Radionuclide Therapy (TRT)?
A: TRT is an advanced cancer treatment that delivers radioactive isotopes directly to tumour cells, maximising therapeutic effects on cancer cells while minimising damage to healthy tissues.
Q: What types of radiation are used in TRT?
A: TRT uses alpha particles, beta particles, and gamma rays. Alpha particles have high energy but limited penetration, beta particles can travel a few millimetres in tissue, and gamma rays have significant penetration power, often used for imaging.
Q: How does TRT achieve targeted delivery to cancer cells?
A: TRT employs molecules like monoclonal antibodies, peptides, or small molecules that specifically bind to unique markers or receptors overexpressed on cancer cells. These molecules are conjugated with radionuclides and administered into the bloodstream, where they bind to cancer cells and deliver the radioactive payload.
Q: What is the bystander effect in TRT?
A: The bystander effect occurs when non-irradiated cells adjacent to targeted cancer cells exhibit damage due to the release of signalling molecules from irradiated cells, extending the therapeutic impact beyond directly targeted cells.
Q: How does the tumour microenvironment affect TRT efficacy?
A: Factors such as hypoxia, interstitial fluid pressure, and stromal cell presence can influence the distribution and uptake of radionuclide conjugates, affecting TRT efficacy. Strategies to modulate the microenvironment can enhance TRT outcomes.
Q: What are some challenges associated with TRT?
A: Challenges include managing radiotoxicity, overcoming cancer cell resistance, and improving radionuclide delivery. Radiotoxicity can affect nearby normal cells, and cancer cells can develop resistance through various mechanisms. Advances in dosimetry, combination therapies, and delivery technologies are critical to addressing these challenges.
Q: Can you name some cancers and their molecular targets treated with TRT?
A: Yes, some examples include:
- Neuroendocrine Tumours (NETs): Targeting somatostatin receptors with Lutetium-177-DOTATATE.
- Prostate Cancer: Targeting PSMA with Lutetium-177-PSMA-617.
- B-cell Lymphomas: Targeting CD20 with Iodine-131-rituximab.
Q: What innovations are improving the precision and efficacy of TRT?
A: Innovations include the use of nanoparticles to carry multiple radionuclides, drugs, or imaging agents, and advances in imaging techniques like PET and SPECT for real-time tracking of radionuclide distribution, optimising treatment plans.
Q: How does tumour heterogeneity affect TRT?
A: Tumour heterogeneity, the existence of diverse cancer cell populations within a single tumour, can affect the uniformity of radionuclide delivery as different cells may express varying levels of target receptors. Combination therapies targeting multiple receptors can help address this challenge.
Q: What are TRT’s future prospects?
A: The future of TRT looks promising with ongoing advancements in molecular biology, imaging, and nanotechnology. These innovations aim to enhance the precision and effectiveness of TRT, offering new hope for improved cancer treatment outcomes.
Disclaimer
The content presented in this article, Biological Principles of Targeted Radionuclide Therapy for Cancer, is intended for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. While the article summarises current scientific understanding and clinical applications of targeted radionuclide therapy (TRT), it does not constitute medical or clinical guidance.
Readers are advised to consult qualified healthcare professionals or specialists before making any decisions related to medical treatment or the use of TRT. Open MedScience makes every effort to ensure the accuracy and reliability of the information at the time of publication, but does not accept liability for any loss, injury, or damage resulting from reliance on this content.
The views and interpretations expressed are those of the authors and do not necessarily reflect those of Open MedScience or its editorial team. Inclusion of specific products, therapies, or radionuclides does not imply endorsement or recommendation by Open MedScience.
All medical treatments, including TRT, carry risks and potential side effects. Decisions about treatment options should be made on a case-by-case basis, in consultation with a licensed medical professional.
home » blog » radiotherapeutics »