Summary: Magnetic Resonance Imaging (MRI) has revolutionised the diagnosis and management of spinal cord tumours through its exceptional soft-tissue contrast, multiplanar capabilities, and absence of ionising radiation. It enables clinicians to distinguish between intramedullary, intradural-extramedullary, and extradural lesions, providing critical anatomical and pathological detail that influences treatment planning and prognosis. This article explores the principles behind spinal cord MRI, characteristic imaging features of various tumour types, advances in imaging technology, and the clinical implications of MRI findings in spinal oncology.
Keywords: Spinal cord tumours, Magnetic Resonance Imaging, intramedullary lesions, spinal neoplasms, diagnostic imaging, neuro-oncology
Introduction
Tumours of the spinal cord represent a diverse group of neoplastic lesions that may arise within or around the spinal cord, leading to neurological dysfunction through compression or neural tissue infiltration. Early and accurate diagnosis is crucial, as delayed recognition often results in irreversible neurological damage. Among the imaging modalities available, Magnetic Resonance Imaging (MRI) is the gold standard for evaluating suspected spinal cord tumours. Its ability to delineate soft-tissue contrast, define tumour boundaries, and assess associated pathological changes has made it indispensable in modern neuroradiology.
MRI not only provides essential diagnostic information but also contributes significantly to preoperative planning and postoperative monitoring. The modality allows clinicians to visualise spinal cord pathology in exquisite detail, identify the exact tumour location, and distinguish between neoplastic, inflammatory, and vascular causes of spinal cord compression.
Principles of MRI in Spinal Cord Imaging
MRI functions on the principle of nuclear magnetic resonance, in which hydrogen nuclei within body tissues align with a strong magnetic field. Radiofrequency pulses temporarily disturb this alignment, and as the nuclei return to equilibrium, they emit signals that are translated into detailed cross-sectional images.
In spinal cord imaging, MRI sequences such as T1-weighted, T2-weighted, and contrast-enhanced scans provide complementary information. T1-weighted images offer clear anatomical detail, while T2-weighted images highlight pathological changes such as oedema, demyelination, or cystic degeneration. Gadolinium-based contrast agents further enhance tumour delineation by highlighting areas of disrupted blood–brain barrier integrity, which is characteristic of many spinal neoplasms.
Advancements such as diffusion tensor imaging (DTI), magnetic resonance spectroscopy (MRS), and functional MRI (fMRI) have extended the diagnostic reach of conventional MRI. These techniques provide insights into tumour cellularity, biochemical composition, and potential involvement of white matter tracts, aiding both diagnosis and surgical decision-making.
Classification of Spinal Cord Tumours
MRI plays a pivotal role in determining the anatomical location of spinal cord tumours, which can be classified as intramedullary, intradural-extramedullary, or extradural. This classification is essential because tumour location often correlates with specific histological subtypes and clinical presentations.
Intramedullary tumours arise within the spinal cord parenchyma itself and include astrocytomas, ependymomas, and hemangioblastomas. MRI typically shows an expanded cord with areas of mixed T2 signal intensity. The presence of syringomyelia or cystic changes adjacent to the lesion is common. Contrast enhancement patterns help differentiate tumour types; for instance, ependymomas often exhibit homogeneous enhancement, while astrocytomas show more heterogeneous uptake.
Intradural-extramedullary tumours are located within the dura but outside the spinal cord. The most common examples are meningiomas and nerve sheath tumours such as schwannomas or neurofibromas. These lesions appear as well-defined masses that compress the cord rather than infiltrate it. On MRI, they typically demonstrate clear margins and avid enhancement following gadolinium administration. Meningiomas often exhibit a characteristic dural tail sign, while schwannomas may show cystic degeneration or a target-like appearance.
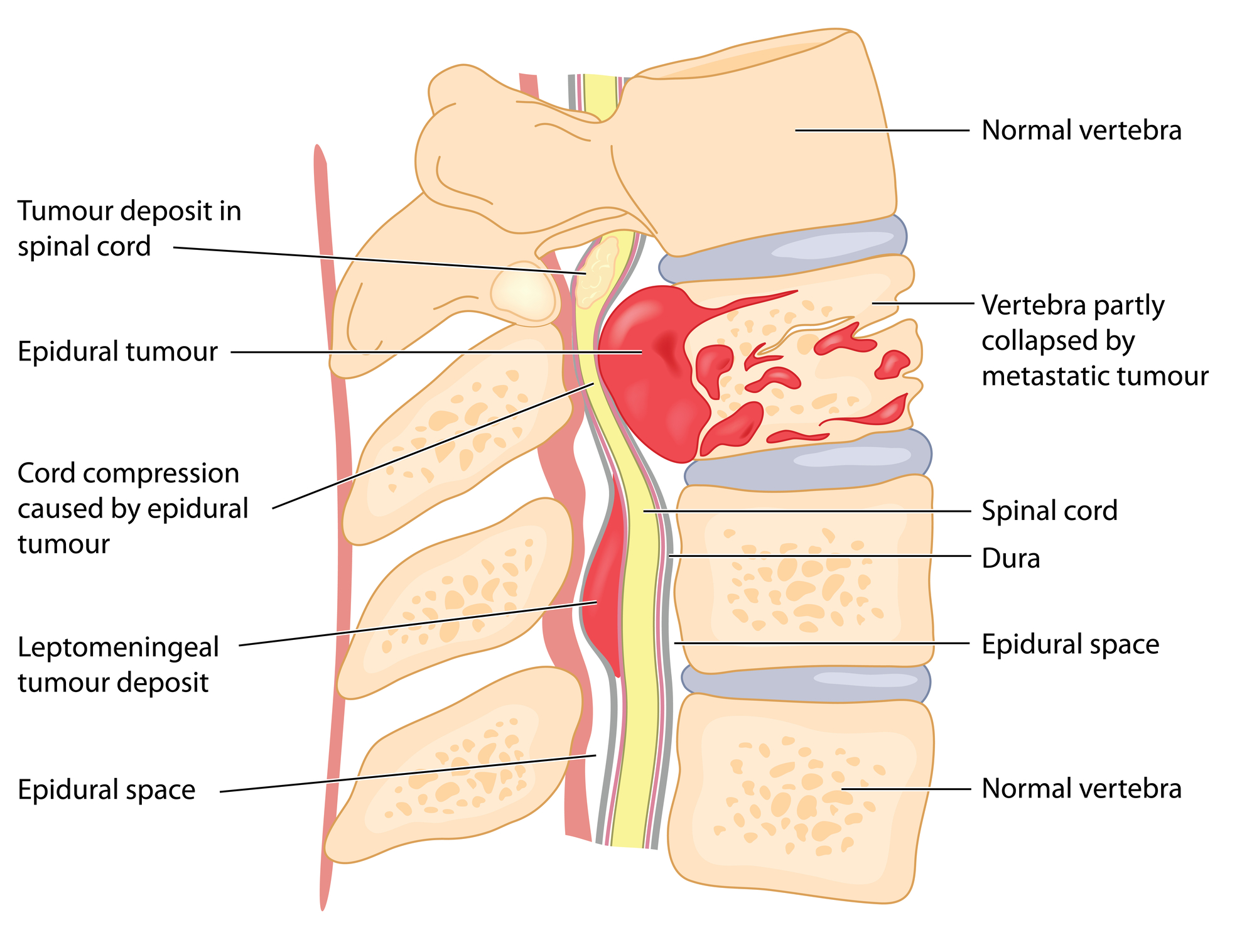
Extradural tumours arise outside the dural sac and usually originate from vertebral bone, epidural fat, or metastatic deposits. MRI is particularly valuable in identifying the extent of epidural spread, vertebral body involvement, and potential spinal canal compromise. The modality also helps distinguish between primary bone tumours and secondary metastases.
MRI Features of Common Spinal Cord Tumours
The imaging characteristics of spinal cord tumours vary depending on their histological type and location. Accurate interpretation requires correlating imaging findings with the clinical presentation and, when necessary, histopathological confirmation.
Ependymomas are the most frequent intramedullary tumours in adults. They are centrally located and may span several vertebral segments. MRI often reveals an isointense or hypointense mass on T1-weighted images and a hyperintense appearance on T2-weighted sequences. The presence of a hemosiderin cap—seen as a hypointense rim on T2—helps distinguish ependymomas from other intramedullary lesions.
Astrocytomas, which are more common in children, tend to be eccentrically located and less well-defined. They usually demonstrate patchy enhancement, with associated oedema and cord expansion. The infiltrative nature of astrocytomas makes complete surgical resection challenging, and MRI findings are critical for evaluating the feasibility of intervention.
Hemangioblastomas are highly vascular tumours often associated with von Hippel–Lindau disease. On MRI, they appear as well-circumscribed nodules with intense enhancement following contrast administration. Flow voids from feeding and draining vessels are frequently visible, indicating their hypervascular nature.
Meningiomas typically occur in middle-aged women and are most often located in the thoracic region. They appear isointense on T1 and T2 images and show uniform enhancement post-contrast. The dural tail sign, which represents thickening and enhancement of the adjacent dura, is a helpful diagnostic feature.
Schwannomas and neurofibromas usually present as round or oval masses that may expand the neural foramen, producing a dumbbell configuration. On MRI, these tumours are iso- to hypointense on T1 and hyperintense on T2-weighted sequences, with variable enhancement patterns. Cystic or haemorrhagic areas may also be present.
Metastatic tumours represent the most common cause of extradural spinal neoplasms. MRI identifies these lesions by their low signal intensity on T1 and high signal on T2, with enhancement following contrast administration. The modality is highly sensitive in detecting vertebral body destruction, epidural extension, and spinal cord compression, which guide oncological management.
Clinical Applications of MRI in Spinal Tumour Diagnosis
The role of MRI extends beyond detection and localisation of spinal tumours; it also informs clinical decision-making throughout the patient’s diagnostic and therapeutic journey.
In the diagnostic phase, MRI helps differentiate tumours from non-neoplastic lesions such as demyelination, infection, or vascular malformations. For example, the identification of a well-defined enhancing mass compressing the cord suggests a neoplastic process, whereas diffuse cord swelling without a discrete lesion may indicate inflammatory or demyelinating disease.
In treatment planning, MRI provides precise information on tumour margins, relationship to the spinal cord, and involvement of surrounding structures. These details are critical for neurosurgeons when determining the surgical approach and minimising postoperative neurological deficits. Additionally, MRI helps evaluate spinal stability in cases with significant vertebral body involvement, which can influence the need for spinal fixation or reconstruction.
During postoperative and follow-up imaging, MRI is essential for assessing residual disease, detecting recurrence, and evaluating treatment response. Contrast-enhanced studies can differentiate between postoperative scar tissue and recurrent tumour. Serial imaging enables clinicians to monitor progression in cases managed conservatively or with adjuvant radiotherapy.
Advances in MRI Techniques for Spinal Cord Tumours
Recent technological developments have significantly improved the diagnostic capabilities of spinal MRI. High-field scanners, typically operating at 3 Tesla, offer enhanced spatial resolution and signal-to-noise ratio, allowing for better visualisation of small or complex lesions.
Diffusion-weighted imaging (DWI) provides insights into tumour cellularity by measuring the random motion of water molecules within tissues. Highly cellular tumours often demonstrate restricted diffusion, which can help differentiate malignant from benign lesions.
Magnetic resonance spectroscopy (MRS) analyses the chemical composition of spinal lesions, offering metabolic information that complements conventional imaging. The presence of certain metabolites, such as choline and lactate, may indicate high-grade or aggressive tumours.
Perfusion MRI measures blood flow within the lesion, which is particularly valuable for distinguishing active tumour tissue from post-treatment changes. Increased perfusion often correlates with tumour angiogenesis and aggressiveness.
Functional MRI (fMRI) and tractography allow for visualisation of functional spinal pathways and white matter tracts. These methods are increasingly used to plan surgical interventions by identifying critical neural structures that must be preserved during tumour excision.
Furthermore, artificial intelligence (AI) and machine learning algorithms are being integrated into spinal imaging workflows. These technologies assist in automated lesion detection, segmentation, and classification, reducing interobserver variability and improving diagnostic accuracy.
MRI in Differentiating Neoplastic and Non-Neoplastic Lesions
A significant diagnostic challenge in spinal imaging is distinguishing tumours from conditions that mimic neoplasia, such as transverse myelitis, multiple sclerosis, sarcoidosis, or vascular malformations. MRI plays a crucial role in this differentiation.
Neoplastic lesions generally cause focal cord expansion and show distinct patterns of enhancement, whereas inflammatory or demyelinating processes tend to produce more diffuse cord signal changes without a discrete mass. In transverse myelitis, for example, T2 hyperintensity extends over several vertebral segments without significant enhancement. Conversely, spinal cord metastases usually exhibit patchy or ring-like enhancement and are often associated with leptomeningeal spread.
Advanced MRI techniques such as DWI and MRS further aid differentiation. Restricted diffusion and elevated choline peaks are more characteristic of neoplastic lesions, while inflammatory changes show variable metabolic profiles. Correct interpretation of these findings is essential to avoid unnecessary invasive procedures and ensure appropriate treatment.
Prognostic and Therapeutic Implications
MRI findings hold significant prognostic value in patients with spinal cord tumours. Tumour size, location, enhancement pattern, and the degree of spinal cord involvement all correlate with patient outcomes. Intramedullary tumours that span multiple vertebral levels or demonstrate extensive infiltration often have poorer prognoses compared to well-circumscribed extramedullary lesions.
In surgical management, MRI helps determine the potential for complete resection. Lesions with clear margins, such as ependymomas or meningiomas, can often be excised completely, leading to favourable outcomes. In contrast, infiltrative astrocytomas may require partial resection followed by adjuvant therapy.
MRI also guides radiotherapy planning by accurately defining the target volume and sparing adjacent healthy tissue. During follow-up, MRI assesses therapy efficacy and identifies radiation-induced myelopathy or recurrent disease.
Limitations and Challenges
Although MRI is the preferred imaging technique for spinal cord tumours, it has several limitations. Motion artefacts caused by patient movement, respiration, or cerebrospinal fluid pulsation can degrade image quality, particularly in long scanning sessions. The use of high-field MRI may introduce susceptibility artefacts, especially near metallic implants.
Gadolinium-based contrast agents, while generally safe, carry a small risk of nephrogenic systemic fibrosis in patients with renal impairment. Furthermore, MRI may not always differentiate between tumour recurrence and post-treatment changes, necessitating correlation with clinical findings or biopsy results.
Accessibility and cost can also be limiting factors in some healthcare settings, potentially delaying diagnosis. Nevertheless, the diagnostic benefits of MRI far outweigh its disadvantages, and ongoing technological advancements continue to mitigate many of these challenges.
Future Directions
The future of spinal tumour imaging is likely to be shaped by continued advances in MRI technology and computational analysis. Ultra-high-field imaging at 7 Tesla offers the potential for unprecedented detail in spinal cord anatomy, although its clinical adoption remains limited.
Integration of AI-driven diagnostic systems promises to streamline image interpretation, detect subtle abnormalities, and predict tumour histology based on imaging biomarkers. Combined with quantitative imaging techniques such as radiomics, these systems may enable personalised treatment planning and more accurate prognostic assessment.
Hybrid imaging methods that merge MRI with positron emission tomography (PET/MRI) are also gaining interest. They combine the superior soft-tissue contrast of MRI with the metabolic sensitivity of PET, providing both anatomical and functional information in a single examination. Such approaches could significantly enhance early detection and treatment monitoring of spinal tumours.
Conclusion
Magnetic Resonance Imaging remains the cornerstone of spinal cord tumour diagnosis and management. Its unparalleled ability to visualise soft-tissue detail, define anatomical relationships, and evaluate pathological processes has transformed spinal oncology. From initial lesion detection to treatment planning and postoperative follow-up, MRI provides clinicians with vital information that shapes therapeutic decisions and influences patient outcomes.
Ongoing developments in imaging technology, including diffusion, perfusion, and spectroscopic techniques, continue to enhance diagnostic precision. As AI and high-field imaging evolve, the role of MRI in spinal tumour assessment will expand even further, reinforcing its status as the most powerful non-invasive tool for evaluating spinal cord pathology.
Q&A: Understanding the Role of MRI in Detecting Spinal Cord Tumours
Q1: Why is MRI considered the gold standard for detecting spinal cord tumours?
MRI provides exceptional soft-tissue contrast, enabling clear visualisation of the spinal cord and surrounding tissues. It accurately defines the size, shape, and extent of tumours without using ionising radiation, offering greater diagnostic detail than CT or X-ray imaging.
Q2: What are the main types of spinal cord tumours identified by MRI?
MRI distinguishes three primary tumour locations: intramedullary (within the spinal cord), intradural-extramedullary (within the dura but outside the cord), and extradural (outside the dura, often involving vertebrae or metastases). This classification guides both diagnosis and surgical planning.
Q3: How does MRI differentiate between various tumour types?
Each tumour type exhibits distinctive imaging features. For instance, ependymomas are centrally located and enhance uniformly with contrast, astrocytomas are irregular and infiltrative, and meningiomas show a characteristic “dural tail” sign. Gadolinium-enhanced imaging accentuates these distinctions, supporting accurate diagnosis.
Q4: What advanced MRI techniques improve tumour assessment?
Techniques such as diffusion-weighted imaging (DWI), magnetic resonance spectroscopy (MRS), and perfusion MRI add valuable data about tumour density, metabolism, and blood supply. These tools help differentiate benign from malignant lesions and refine pre-surgical assessment.
Q5: How does MRI contribute to treatment planning?
MRI defines tumour margins and their proximity to spinal and bony structures, allowing surgeons to plan interventions that minimise neurological damage. It also identifies spinal instability, which may influence the decision to perform fixation or reconstruction procedures.
Q6: Can MRI be used after surgery or during follow-up?
Yes. Postoperative MRI detects residual or recurrent disease, differentiates scar tissue from tumour recurrence, and evaluates response to radiotherapy or chemotherapy. Serial scans allow for long-term monitoring and timely intervention if changes occur.
Q7: What are some limitations of MRI in spinal tumour imaging?
MRI can be affected by motion artefacts, long scan times, and interference from metallic implants. Distinguishing between post-treatment effects and tumour recurrence can be challenging, and high costs or limited access may delay diagnosis in certain healthcare settings.
Q8: How is artificial intelligence changing spinal MRI interpretation?
Artificial intelligence (AI) is transforming image analysis by automating lesion detection, segmentation, and classification. AI tools enhance diagnostic consistency, reduce reporting time, and may eventually predict tumour histology and prognosis through image-based biomarkers.
Q9: What makes MRI superior to other imaging techniques for spinal tumours?
MRI visualises both soft tissue and bone in one scan without radiation exposure. It identifies spinal cord compression, oedema, cystic degeneration, and vascular changes, offering a complete diagnostic picture that other imaging modalities cannot match.
Q10: What does the future hold for MRI in spinal tumour detection?
Emerging technologies such as ultra-high-field MRI (7 Tesla), PET/MRI fusion, and AI-driven analytics promise greater precision and personalisation in diagnosis. These developments will enhance early detection, improve treatment outcomes, and deepen understanding of spinal tumour behaviour.
Glossary of Key Terms
Astrocytoma: A tumour that starts inside the spinal cord, made up of support cells called astrocytes. These tumours often spread within the cord and can be harder to remove completely.
Diffusion-Weighted Imaging (DWI): A special MRI scan that shows how water moves inside tissues. It helps doctors tell the difference between cancerous and non-cancerous growths.
Ependymoma: A common spinal cord tumour in adults that usually grows slowly and has clear edges. It often shows up brightly when contrast dye is used in MRI.
Extradural Tumour: A tumour that grows outside the protective covering of the spinal cord, often starting in the bones or spreading from another part of the body.
Functional MRI (fMRI): A type of MRI that shows how different parts of the brain or spinal cord work by measuring blood flow. It helps surgeons plan operations safely.
Gadolinium: A contrast dye used in MRI scans to make tumours and blood vessels more visible.
Hemangioblastoma: A small, blood-rich tumour that can appear in the spinal cord, sometimes linked to a rare inherited condition called von Hippel–Lindau disease.
Intradural-Extramedullary Tumour: A tumour that grows inside the spinal canal but outside the spinal cord. Common examples include meningiomas and schwannomas.
Intramedullary Tumour: A tumour that starts within the spinal cord itself, such as astrocytomas or ependymomas.
Magnetic Resonance Spectroscopy (MRS): An MRI technique that studies the chemical makeup of a tumour, helping doctors learn how aggressive it might be.
Meningioma: A usually non-cancerous tumour that grows from the membranes covering the spinal cord. It often has a “tail-like” appearance on MRI.
Metastatic Tumour: A tumour that has spread to the spine from another organ, such as the lungs or breast.
Perfusion MRI: A scan that measures blood flow in tissues and helps doctors see if a tumour is active or shrinking after treatment.
Schwannoma: A benign tumour that grows from the cells covering nerves. It may press on the spinal cord, but it can usually be removed safely.
Syringomyelia: A fluid-filled cavity inside the spinal cord that can form near a tumour or other spinal problem.
T1- and T2-Weighted Images: Two main MRI scan types. T1 shows body structure in detail, while T2 highlights fluid, swelling, or damage.
Tractography: An MRI technique that shows nerve pathways in the spinal cord to help surgeons avoid damaging them during surgery.
Von Hippel–Lindau Disease: A rare inherited disorder that causes tumours to grow in different parts of the body, including the spinal cord.
Disclaimer
The information presented in “How MRI Transforms the Detection and Diagnosis of Spinal Cord Tumours” by Open MedScience is intended solely for educational and informational purposes. It is not a substitute for professional medical advice, diagnosis, or treatment. Readers should not rely on the content of this article for personal health decisions and are advised to consult qualified healthcare professionals regarding any medical concerns or conditions.
While every effort has been made to ensure accuracy and relevance at the time of publication, Open MedScience does not guarantee the completeness or current validity of the information provided. The content may include general discussions of medical or imaging technologies that could evolve over time. Open MedScience and its contributors accept no responsibility or liability for any loss, injury, or damage resulting from reliance on the material contained herein.
All imaging descriptions and clinical discussions are for general understanding and should not be interpreted as recommendations for individual patient care or as a basis for clinical decision-making.
home » blog » medical imaging modalities »