Summary: Blastoma tumours are rare and typically affect children, requiring precise diagnosis and staging to optimise treatment outcomes. This article investigates the imaging techniques used to diagnose and stage blastoma tumours, including ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), and nuclear medicine techniques such as positron emission tomography (PET). It discusses the principles, advantages, and limitations of these modalities, as well as their role in guiding therapeutic decisions.
Introduction to Blastoma Tumours
Blastomas are rare malignancies originating from embryonal cells that fail to differentiate properly during development. Common types include neuroblastoma, nephroblastoma (Wilms’ tumour), and retinoblastoma. Diagnosing and staging these tumours accurately is critical to determining prognosis and tailoring treatment regimens. Imaging plays a pivotal role in assessing tumour size, location, metastasis, and response to therapy.
Ultrasound: A First-Line Tool
Ultrasound is often the first imaging modality used in children suspected of having a blastoma, due to its accessibility, non-invasive nature, and absence of ionising radiation.
Principles of Ultrasound in Blastoma Detection
Ultrasound employs high-frequency sound waves to generate real-time images of soft tissues. The echo patterns provide information on the size, location, and echogenicity of the tumour, which can help differentiate between cystic and solid masses.
Applications in Specific Blastomas
- Nephroblastoma: Ultrasound is particularly useful for identifying renal masses, which are characteristic of Wilms’ tumour. It can determine if the tumour is confined to the kidney or invading surrounding structures.
- Neuroblastoma: In cases of abdominal neuroblastoma, ultrasound can locate the adrenal gland origin and detect calcifications, a hallmark of this tumour.
- Retinoblastoma: Although ultrasound is not a primary tool for retinoblastoma, it is occasionally used to assess intraocular masses when MRI is unavailable.
Advantages and Limitations
- Advantages: Non-invasive, cost-effective, and safe for children.
- Limitations: Limited penetration in obese patients and operator-dependent accuracy.
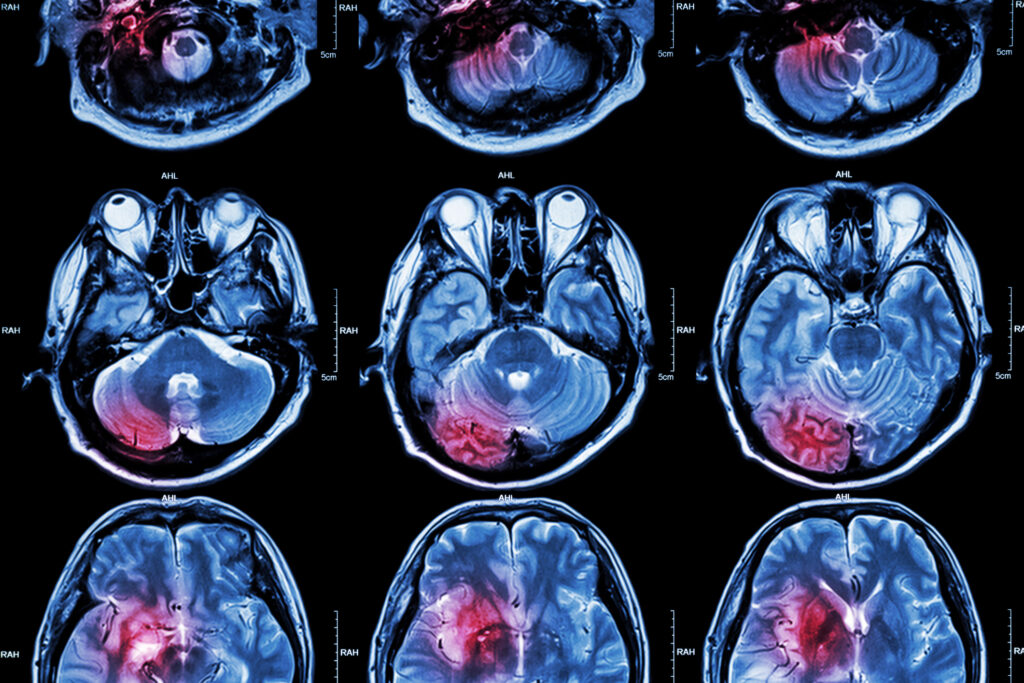
Computed Tomography (CT): Providing Detailed Anatomy
CT scanning is a mainstay in the evaluation of blastomas due to its ability to provide detailed cross-sectional images.
Principles of CT Imaging in Blastoma Tumours
CT uses X-rays to produce high-resolution, 3D images of internal structures. Contrast agents are often administered to enhance the visualisation of vascular and soft tissue components of the tumour.
Applications in Blastoma Staging
- Neuroblastoma: CT is critical for assessing tumour extension into the spinal canal or mediastinum and for detecting metastases in the liver, lungs, or bones.
- Nephroblastoma: CT is employed to evaluate the contralateral kidney, lymph node involvement, and any evidence of tumour rupture.
- Retinoblastoma: CT is useful for detecting calcifications within the tumour, a hallmark feature of retinoblastoma.
Advantages and Limitations
- Advantages: Rapid acquisition of images, superior resolution for detecting calcifications and metastases.
- Limitations: Exposure to ionising radiation and less sensitivity compared to MRI in detecting soft tissue infiltration.
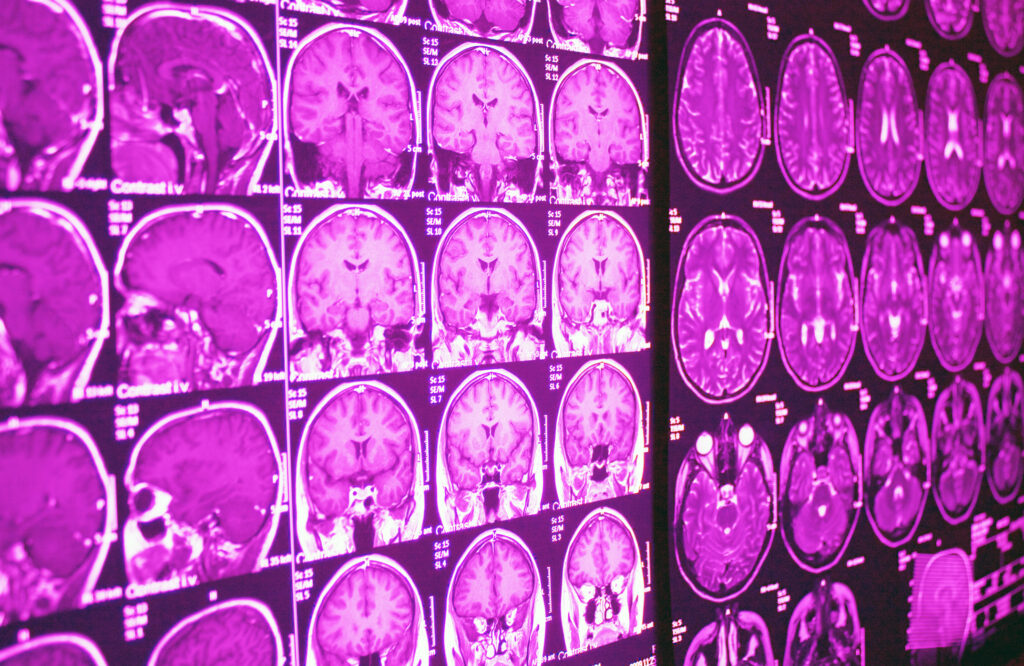
Magnetic Resonance Imaging (MRI): A Gold Standard in Soft Tissue Evaluation
MRI is often considered the gold standard for imaging soft tissues, particularly in staging and surgical planning for blastomas.
Principles of MRI
MRI employs a strong magnetic field and radio waves to create high-resolution images of tissues. It provides superior contrast resolution compared to CT, enabling detailed visualisation of tumour boundaries and surrounding structures.
Applications in Blastomas
- Neuroblastoma: MRI is preferred for evaluating spinal canal involvement and detecting metastases in the bone marrow.
- Nephroblastoma: It provides excellent visualisation of the renal capsule and helps differentiate between Wilms’ tumour and other renal masses.
- Retinoblastoma: MRI is crucial for assessing optic nerve invasion and extraocular spread.
Advanced MRI Techniques
- Diffusion-Weighted Imaging (DWI): DWI enhances tumour characterisation by measuring the diffusion of water molecules in tissues, aiding in distinguishing benign from malignant masses.
- Magnetic Resonance Spectroscopy (MRS): MRS analyses tumour metabolism and can provide non-invasive insights into tumour biology.
Advantages and Limitations
- Advantages: No radiation exposure, superior soft tissue resolution.
- Limitations: Higher cost, longer acquisition times, and the need for sedation in young children.
Nuclear Medicine: Functional Insights into Tumour Biology
Positron Emission Tomography (PET): A Functional Imaging Modality
PET imaging involves the use of radiotracers such as fluorodeoxyglucose (FDG) to assess metabolic activity. Malignant tumours often exhibit increased glucose uptake, which is detected by PET.
- Neuroblastoma: PET is highly sensitive for identifying bone marrow metastases and monitoring response to chemotherapy.
- Limitations: Limited sensitivity for detecting small or low-grade tumours.
Single-Photon Emission Computed Tomography (SPECT)
SPECT is a complementary technique to PET, providing functional imaging with different radiotracers. For instance, MIBG (metaiodobenzylguanidine) scintigraphy is specific to neuroblastoma cells, enabling accurate detection of primary and metastatic lesions.
Staging Blastomas with Imaging
Staging is a critical step in determining the extent of disease and guiding treatment. Imaging modalities play a pivotal role in identifying the tumour’s size, local invasion, and metastases.
International Neuroblastoma Staging System (INSS)
- Stage 1: Localised tumour, completely excised.
- Stage 2: Localised tumour with incomplete excision.
- Stage 3: Unresectable tumour crossing the midline.
- Stage 4: Disseminated disease involving distant lymph nodes, bone marrow, liver, or skin.
Wilms’ Tumour Staging
The staging of Wilms’ tumour (according to the National Wilms Tumor Study Group) includes:
- Stage I: Limited to kidney, completely excised.
- Stage II: Extends beyond kidney but is excisable.
- Stage III: Residual tumour post-surgery or positive lymph nodes.
- Stage IV: Distant metastases present.
Integrating Imaging into Treatment Planning
Preoperative Planning
Imaging defines tumour boundaries and aids in determining the feasibility of surgical resection while minimising risks to vital structures.
Assessing Treatment Response
Serial imaging allows clinicians to monitor tumour shrinkage and detect residual disease. PET and MRI are particularly valuable for evaluating metabolic and structural changes during therapy.
Long-Term Surveillance
Following treatment, imaging is employed to detect recurrence or late metastases. MRI is often preferred due to the absence of radiation.
Emerging Imaging Technologies
Artificial Intelligence (AI) in Imaging
AI algorithms are increasingly used to automate tumour detection, quantify tumour burden, and predict outcomes based on imaging data.
Hybrid Imaging Techniques
Hybrid modalities such as PET/MRI combine functional and anatomical imaging, offering comprehensive insights into tumour biology and its microenvironment.
Conclusion
Imaging is indispensable in the diagnosis and management of blastomas. Ultrasound, CT, MRI, and nuclear medicine techniques each play unique roles in evaluating tumour characteristics and guiding treatment decisions. Advances in imaging technology, including AI and hybrid modalities, promise to further enhance the accuracy and efficiency of blastoma diagnosis and staging. Collaborative efforts among radiologists, oncologists, and surgeons remain essential to achieving optimal outcomes for patients.
Disclaimer
The content provided in this article, Imaging Techniques Used to Diagnose and Stage Blastoma Tumours, is intended for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Readers are advised to consult qualified healthcare professionals regarding any medical condition or imaging-related decision. While every effort has been made to ensure the accuracy of the information at the time of publication, Open Medscience makes no warranties or representations regarding its completeness, reliability, or applicability in clinical practice. The views expressed are those of the authors and do not necessarily reflect those of Open Medscience or its affiliates. Use of any information contained in this article is at the reader’s own risk.
home » blog » medical imaging modalities »