Radiotheranostics change how you look at cancer because you don’t start with guessing, you start with seeing.
You use one radioactive compound to light up the exact cells you’re trying to treat and then use a paired version to hit those same cells with targeted radiation. This find-it-treat-it approach means that you can cut down on the uncertainty that, sadly, usually comes with oncology.
And this isn’t a niche idea anymore. Look at what the hospitals are already doing: they’re shifting toward treatments that show you, before anything is given, whether a tumour even has the right kinds of receptors to respond.
Researchers are moving away from old limits of prostate or neuroendocrine cancers and pushing radiotheranostics into breast, brain, and even blood cancers.
This field still isn’t polished, though, because you’re dealing with isotope shortages and long approval pipelines. Plus, many hospitals aren’t built for this kind of workflow.
But the momentum is real, and this change is happening right now.
Current Challenges That Limit Widespread Integration
When it comes to cancer care, radiotheranostics is the next natural upgrade.
However, the process of bringing it into everyday practice is much harder than it looks. There are infrastructure gaps standing in the way, as well as a shortage of medical staff all over the country. On top of that, the regulations are incredibly strict, and there are still issues with production.
You need facilities that many hospitals don’t have, like hot labs, cyclotron access, radiopharmaceutical prep rooms, and solid radiation-safety systems. Even centres that do have the space often don’t have anyone to run it.
Then there’s regulation.
Radiopharmaceuticals follow stricter and slower paths than standard drugs. On top of that, their short half-lives make production and transport a constant race against the clock.
And frequent shortages of key isotopes like 177Lu and 225Ac make an already hard situation seem impossible.
Key Radiotheranostics Data Points in 2025
These statistics hint at the future of radiotheranostics:
- The incidence/prevalence of neuroendocrine tumours (NETs) is on a continued increase; it has doubled over the last two decades
- The radiolabeled somatostatin analogue – Lutetium Lu-177-dotatate – is standard treatment for somatostatin receptor-positive GEP-NETs
- An integration of diagnostics and therapeutics is suggested to personalise cancer treatment, and if successful, the RRI and lutetium Lu-177-dotatate combination is believed to be promising for GEP-NETs
- The Radioligand Therapy Market is projected to reach $13 billion (USD) by 2030, a CAGR of ~5%
- The approval of drugs such as Lutathera (Lu-177-dotatate) for the treatment of NETs and Pluvicto (Lu-177-PSMA-617) for the treatment of prostate cancer was seen as a significant boost to the market
- The estimated global stock of health workers is currently 70+ million; a shortfall of 10 million health workers is projected globally by 2030
- A target has been set to substantially increase health financing (recruitment, development, training, and retention of the health workforce) in developing countries
- SSTR-PET/CT has shown a 10% higher detection rate compared to older imaging methods (e.g., planar/SPECT gallium-67 scan)
New Technologies and Opportunities in 2025
In 2025, the tools are getting sharper, so radiotheranostics is moving into new territory.
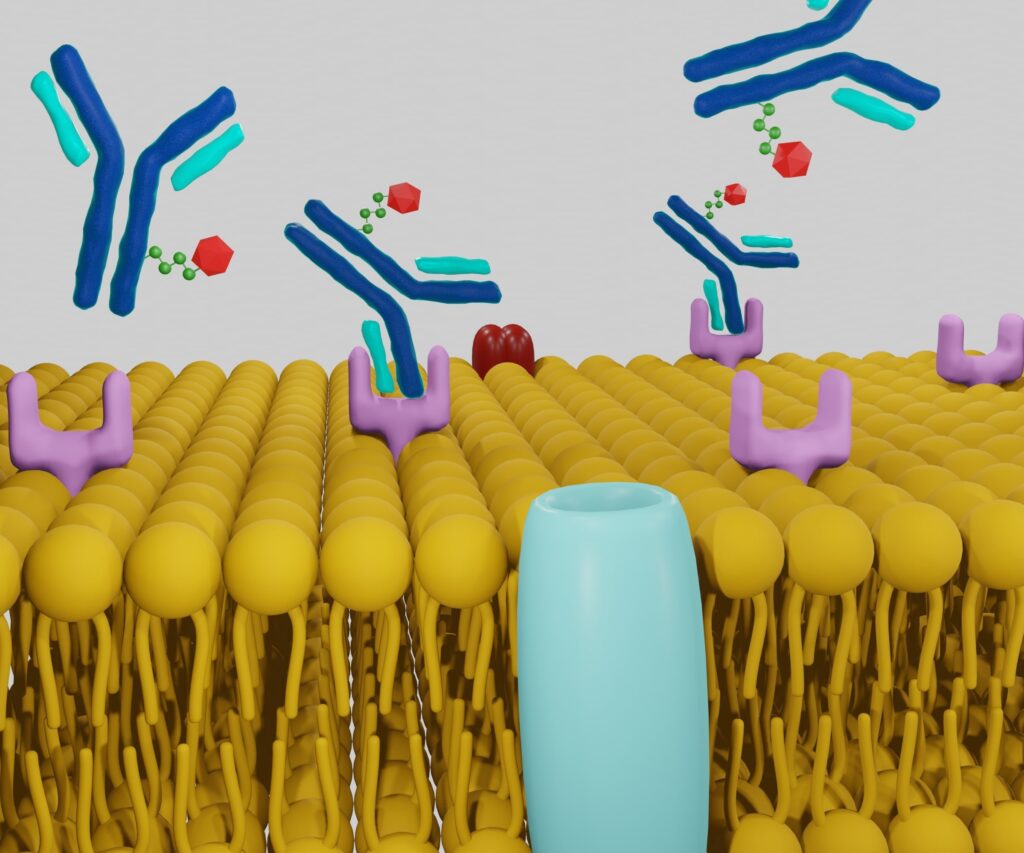
Targeting molecules are no longer limited to familiar peptides, and you now see antibody fragments, nanobodies, engineered peptides, and small molecules that easily reach tumours and reduce the amount of radiation healthy tissue gets.
Radionuclides are also getting more advanced.
Alpha emitters (e.g., 225Ac, 221At) provide control over tiny metastases, while optimised beta emitters (e.g., 177Lu, 161Tb) help balance power/safety.
AI is already playing an important role in all of this as it helps spot lesions earlier and read uptake more clearly (and with the semi-recent emergence of the technology, this is probably the start).
But this level of accuracy isn’t tied to just oncology; you can see the same thing in trauma care. Imaging for Chicago bicycle pelvic fractures can look very different from what you’d see in a place like Phoenix, simply because the volume of patients and hospital protocols don’t match (the higher the volume, the bigger the sample size). When you compare those two settings, it becomes obvious why technology plays such a huge part – it gives you more dependable information.
Implementation Strategies for Hospitals and Oncology Programs
For a hospital to be able to offer radiotheranostics, the whole process needs to be carefully planned.
Building Multidisciplinary Clinical Teams
You need several specialties working together from day one: nuclear medicine, oncology, radiology, radiation oncology, physics, nursing, and radiopharmacy.
Each group handles a different part of the patient’s care, so the real work is in how you communicate. If the information flows freely between teams, the treatment stays safe, and there are no delays.
Standardising Imaging and Dosimetry Protocols
Your scans need to look the same every time, which means matching PET and SPECT settings across the program.
Dosimetry should follow a simple, repeatable workflow so different members of the staff reach the same results. When the whole process is consistent, there are fewer mistakes, and it’s easier for multi-centre studies to join later.
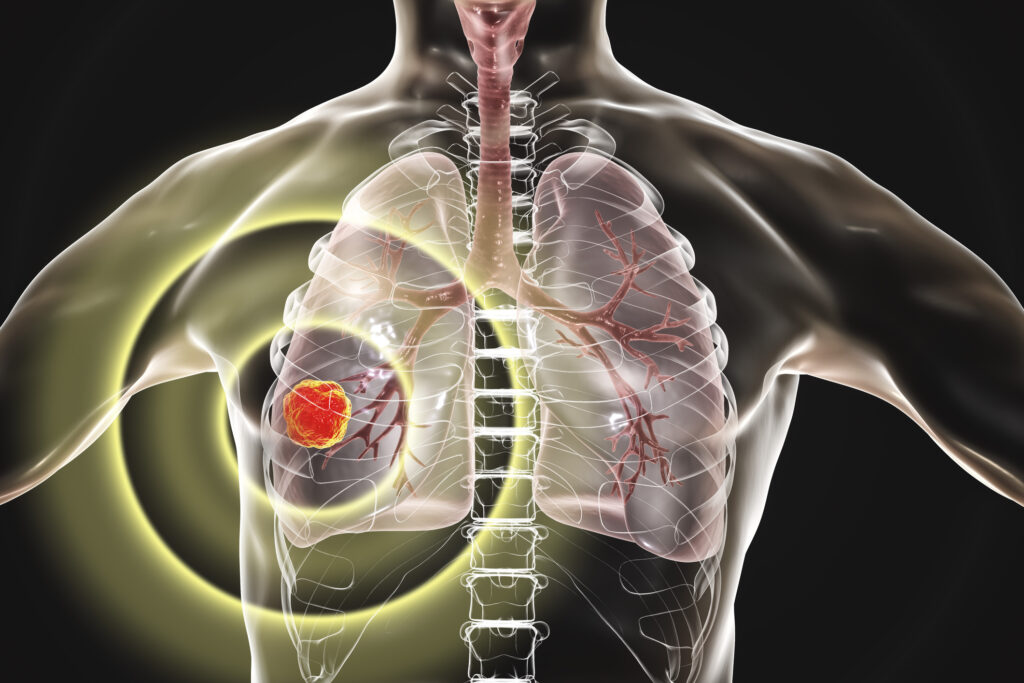
Biomarker-Driven Patient Selection
You choose patients based on multiple factors (e.g., receptor expression, where the cancer has spread, their health history, the treatments they’ve already had, etc.).
SSTR-PET and PSMA-PET are the types of tools that show whether you can target a tumour or not. While this might sound cold, it’s efficient, and it helps save lives. This is because you get to focus on the patient who will respond to the treatment, while you’re skipping those who won’t.
Safety, Monitoring, Follow-Up
For both staff and patients, there are strict safety procedures/measures when it comes to radiation. Even more so for staff, because they’re likely exposed much more frequently (e.g., on a daily basis) compared to the patient, who may be exposed only once in an entire lifetime.
After each treatment, it’s important to monitor kidney function, bone-marrow counts, salivary issues, and any other stomach-related side effects. Regular scans and biomarker checks help determine whether therapy is working and if any adjustments are necessary.
Conclusion
The oncology of ‘yesterday’ was treated first and confirmed later. While the oncology of ‘tomorrow’ is where you run both diagnostics and treatment at the same time. And it’s all made possible thanks to radiotheranostics.
So it’s unlikely it’ll go anywhere. But it is possible it’ll evolve into something new.
Sure, you’ll still deal with some of the messy parts (e.g., scarce isotopes, slow approval, etc.), but the direction oncology is going towards is obvious – forward.
Disclaimer
The information presented in Radiotheranostics in Oncology – Current Challenges and Emerging Opportunities in 2025 is intended for educational and informational use only. It should not be interpreted as medical advice, clinical guidance, or a substitute for consultation with qualified healthcare professionals. Radiotheranostic procedures, radiopharmaceutical use, imaging protocols, and oncology treatments involve risks, regulatory requirements, and clinical decisions that must be evaluated by licensed practitioners within appropriate clinical settings.
Open MedScience does not endorse any specific product, drug, therapy, radionuclide, or clinical approach referenced in this article. All data, projections, and market figures reflect sources available at the time of writing and may change as research develops. Readers should verify any clinical or technical information before applying it in practice.
Treatment eligibility, patient selection, safety procedures, and diagnostic pathways vary between institutions and jurisdictions. Any examples provided are illustrative and should not be used as direct clinical recommendations.
Open MedScience, its authors, and its partners accept no responsibility for any loss, harm, or consequences arising from the interpretation or application of the information contained in this article. Readers are strongly encouraged to seek specialist advice when making decisions related to radiotheranostics, oncology practice, or healthcare provision.
You are here: home » diagnostic medical imaging blog »