Targeted radionuclide therapy (TAT) was first used to treat cancer for an ‘over-active’ thyroid using radioactive iodine-131 seeds.
Targeting cancer cells with therapeutic bullets
Targeted radionuclide therapy (TAT), such as targeted alpha therapy, is a new approach in the treatment of cancer, and this blog article will provide a general overview of the current status. This kind of therapy was first used to treat cancer for an ‘over-active’ thyroid using radioactive iodine-131 seeds. These seeds concentrate in the thyroid gland and emit strong gamma and beta particle radiation to kill the cancer cells, leaving the healthy cells mostly intact.
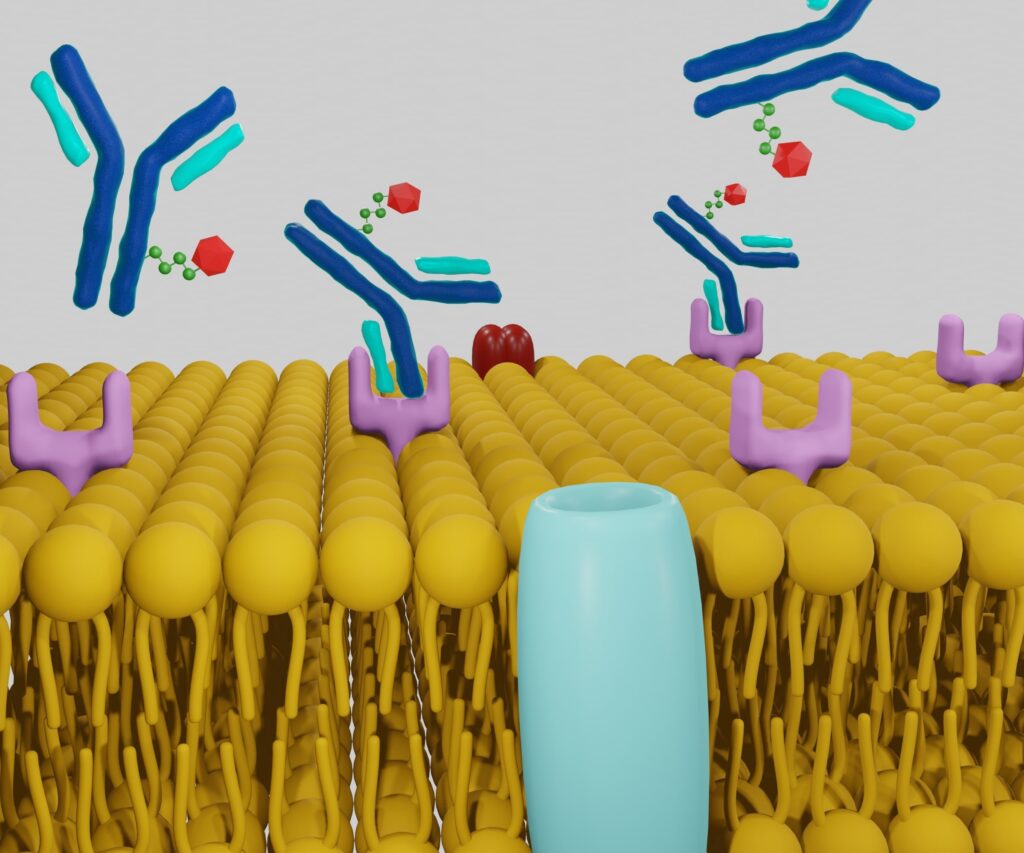
Over the past decade, there has been considerable interest in developing targeted radionuclide therapy to treat lymphoma and liver cancers. The radioactive source can be tagged to biological peptides, drug substrates and monoclonal antibodies. The activity is transported to the cancer site, killing the cancer cells.
Monoclonal antibodies have been used to treat lymphomas but are proving unsuccessful in treating solid tumours. To circumvent these issues, low-molecular-weight drug molecules have been designed to deliver high doses of radiation via emitting radiometals and also to recognise certain receptors on the surface of solid tumours. This has been successfully demonstrated with the use of somatostatin analogues to treat neuron-endocrine tumours and metastatic liver cancers where surgery is not viable.
Alpha particles
The therapeutic potential of several alpha particle-emitting radionuclides has been assessed to treat a range of cancers. Alpha particles are positively charged and have a mass of four units and a charge equal to that of the helium nucleus. The energy range for alpha particles is between 5 and 9 MeV. These highly charged particles can travel between 5 and 10 cell widths in living tissues. They travel in straight lines and leave about 80 to 100 keV/µm energy in their path. The maximum rate of energy increases to approximately 300 keV/µm at the end of each track.
When considering the use of alpha particles for cancer treatment, it is important to consider the molecular distance from the point source (the radionuclide) during the radionuclide decay from the tumour cell’s nucleus. Another factor is the interaction of the alpha particle when bound to the DNA in cancer cells.
Hence, when radionuclides decay, they emit a quantity of energy and accumulation in the tumour – which can result in the death of cancer cells – leaving the healthy cells with minimum damage. Therefore, to destroy a cancer cell, the high energy alpha-emitting particle must be contained within the volume of the tumour.
Linear energy transfer
In 1927, the researchers Regoud and Lacassagne used alpha-emitting radionuclides to target tumours due to their high linear energy transfer properties. When these alpha-emitting radionuclides are conjugated to carrier molecules such as drug substrates, peptides or monoclonal antibodies, they can deliver a radiation dose to tumour cells. The accumulation of radiation inside the tumour causes the cancer cells to die, leaving the majority of normal cells unable to function properly.
Various studies have shown that the ideal radionuclides for targeted radionuclide Therapy (TAT) must have all these basic characteristics:
- The energy emitted from the electrons of the radionuclide should be lower than 40keV
- The photon-to-electron emission ratio should be within 2 units.
- For practical and treatment purposes, the radionuclide’s half-life must be within the range of 30 minutes to 10 days.
- To generate ‘medical’ radionuclides, the daughter radionuclide must be stable with a half-life higher than 60 days
- The radiochemical transformations must incorporate the radionuclide into the carrier substrate efficiently and timely.
The critical factors that make an excellent radionuclide for selectively killing cancer cells are the linear energy transfer (LET) and relative biologic effectiveness (RBE) of the emitted particles. The property LET measures the number of ionisations taking place when a charged particle passes through a number of cell widths.
These doubly charged alpha particles have a high LET value of approximately 100 keV/µm compared to beta particles with a low LET value of 0.2 keV/µm. The other property RBE refers to is a measure of dose relating to x-rays and is called reference radiation; this is closely related to LET.
The extent of damage to cells varies between low and high LET radiation values. At high LET levels, double-stranded DNA tends to break down more than at low LET levels. It has been calculated that LET ranges are of the order of 100–200 keV/µm, causing maximum breaks in tumour DNA. This is because the ionisations equate to the distance between the double-stranded DNA.
Therefore, the advantage of using alpha emitters is that they do not destroy all the healthy cells in the vicinity of the cancer cells. For example, the alpha emitter bismuth-213 – coupled with the anti-CD33 monoclonal antibody – has been used to treat myeloid leukaemia.
Targeted alpha therapy
To develop targeted alpha therapy into a viable treatment for cancer, there is a need to supply the alpha emitter radionuclides at the site where the radioactive drugs are to be prepared and delivered. Over the last twenty years, the most popular radionuclide generator uses the actinium-225/bismuth-213 radionuclide combination.
Hence, bismuth-213 emits both alpha and beta particles and mostly decays to give the alpha emitter polonium-213. Pre-clinical trials using bismuth-213, which has an associated half-life of 46 minutes, and actinium-225, which has a half-life of 10 days, have been successful in treating a variety of cancers, including leukaemia, melanoma, and lymphoma.
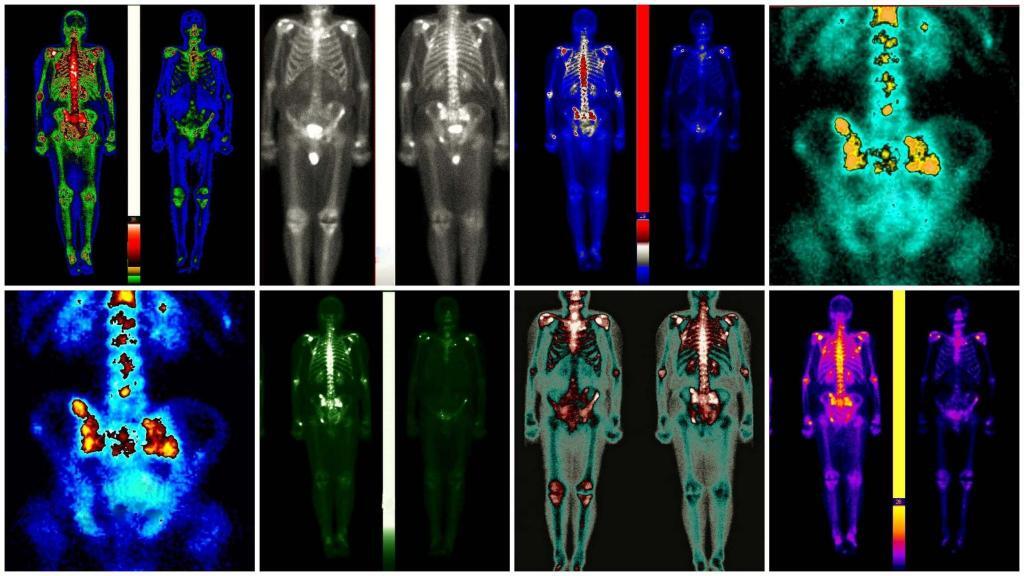
In various nuclear medicine departments, more than 130 patients have received this novel treatment, which targets alpha therapy by using the alpha emitter’s bismuth-213 or actinium-225 coupled to peptides and monoclonal conjugates.
A new radionuclide generator can produce 100 mCi of bismuth-213 from the parent actinium-225 to synthesise radionuclide-antibody conjugates. The generator’s setup contains a prefilled syringe of hydrochloric acid connected to an organic resin containing another syringe filled with actinium-225 and a hydrochloric acid mixture. This mixture produces the alpha emitter bismuth-213 under negative pressure and is able to generate six doses of bismuth-213 every 24 hours.
To prepare radioimmunopharmaceuticals, a source of the radiometal must be generated and have a realistic half-life. One of the best radiometals that fits this criterion is bismuth-213, which has a half-life of 46 minutes. This alpha-emitting radiometal is central to targeted alpha therapy and has been used in human clinical trials to kill leukaemia cells when conjugated with the monoclonal antibody HuM195.
These alpha-emitting particles possess cytotoxic properties and ‘selectively’ kill tumour cells due to their short-range and high LET value. Most importantly, they tend not to damage many of the surrounding normal functional cells. The generation of bismuth-213 and the preparation of the radiopharmaceutical are completed within 30 minutes (using an automated radiochemical synthesis set-up). During the synthesis of the radiopharmaceutical, the activity of bismuth-213 can be reduced by one-third.
To circumvent these large activity losses, a process has been developed where the activity is eluted off directly into the actinium-225/bismuth-213 generator and the ‘naked’ bismuth-213 is eluted off directly into the buffered antibody solution. The chelator DTPA is then added to both the bismuth-213 and the antibody. The whole process can take about 10 minutes, and after anion exchange purification, the radiopharmaceutical drug can be injected into the patient.
Metastatic melanoma
Targeted alpha therapy is used in the treatment of metastatic melanoma by using the monoclonal antibody 9.2.27. This monoclonal antibody is tagged to the chelator DTPA containing the alpha emitter bismuth-213. The resultant immuno-conjugate is then used to carry out an assessment of the patient by using tumour imaging-specific biomarkers to look at the changes in tumour growth.
A study of 22 patients with stage IV melanoma metastatic cancer was treated with a range of activities ranging from 55 MBq to 947 MBq. The RECIST criteria (Response Evaluation Criteria in Solid Tumours) assessed the cancers. The outcome of this therapy showed 14% of the patient group gave a partial response, with 30% leading to progressive disease.
However, the usage of tumour marker melanoma inhibitory activity protein (MIA) showed a reduction over a period of two months in most of the patients. This group of patients showed no toxic side effects, demonstrating that targeted alpha therapy could be a safe and effective treatment for metastatic melanoma.
Alpha emitting immuno-conjugate bismuth-213-DTPA-9.2.27 was assessed for its application in targeted alpha therapy to kill melanoma cancer cells. The radioconjugate, bismuth-213-DTPA-9.2.27 used in vitro and in vivo biological systems have been employed in a number of small clinical trials to study pharmacokinetics and toxicology profiles in the treatment of melanoma.
Melanoma, in its metastatic cancer state, has to develop through a number of stages. During the advanced stages of tumour development, cancer cells are diffused out of the tumour site into the lymphatic circulation system. These free-flowing cancer cells can then group together and infiltrate the body’s vital organs. On mass, they can then impede the functions of that particular organ and eventually lead to organ failure.
The key to understanding metastatic cancer is to work out the bio-mechanism of how antigens help the spread of cancer cells. Consequently, future radiopharmaceuticals can be designed to treat and target melanomas.
Targeting gliomas
Gliomas are associated with ‘adult’ brain tumours and stem from the glial part of the brain. They become malignant due to the high concentration of neurokinin type 1 receptors on the tumour. Brachytherapy is used to treat these gliomas by inserting radioactive iodine-125 seeds into the tumour site. This approach is very effective for low-grade gliomas. Unfortunately, for the treatment of high-grade gliomas, therapy is required to diffuse the activity onto the surface of the tumour. In order to circumvent these problems, it is necessary to design selective cytotoxic radiopharmaceuticals which can find and latch onto the neurokinin type 1 receptors.
Therefore, it was necessary to use the radionuclide bismuth-213, which has a half-life of 46 minutes. This alpha emitter was chelated and attached to a low molecular weight drug, which transported the activity to the surface of the tumour, where it spread out over the entire tumour volume to kill it. The radiopharmaceutical drug used in the study was [DOTAD-Phe-Tyr]—octreotide.
Previous studies have shown that the DOTAD moiety can chelate the radionuclides yttrium-90 and indium-111 and target somatostatin type 2 receptors in gliomas. This approach was taken further to design a novel peptide that can specifically target the neurokinin type-1 receptor in malignant gliomas.
The ligand used in this case was substance-P, which is based on a tachykinin neuropeptide. Interestingly, neurokinin type-1 receptors have also been located in the central nervous system and appear in lesions of patients with multiple sclerosis.
Consequently, the chelator (DOTAGA) was conjugated to the arginine amino acid residue of the eleven-unit peptide Substance-P to generate the (DOTAGA-Arg-Substance-P). This radiopharmaceutical peptide was then administered to 20 patients in a pre-clinical study to assess its effects on gliomas.
The study concluded that 13 patients showed tumour shrinkage, and further clinical trials were needed to evaluate the targeted alpha therapy approach for the treatment of advanced brain gliomas.
Conclusion
The incorporation of alpha particles into the design of the drug has many advantages, including short-range, high LET and high energy, leading to high radiobiological effectiveness (RBE). Therefore, bismuth-213, which has a 46-minute half-life, can be incorporated into radiopharmaceuticals due to its easy generation from the actinium-225/bismuth-213 generator, with a 10-day half-life. This allows actinium-225 to be transported to hospitals and research laboratories to allow radiochemists to design effective targeted alpha therapy drugs to kill melanoma and other types of cancer.
Q & A – Targeted radionuclide therapy (TAT)
Why are higher levels of LET >200keV/µm not good for the treatment of tumours?
The linear energy transfer (LET) of an alpha particle gives it the ability to interact with the surrounding cells leading to ionisations over a certain distance. Alpha particles – which are doubly positively charged – possess a high LET value of approximately 100keV/µm. The smaller beta particles can travel further but have decreased LET value of 0.2keV/µm.
Linear Energy Transfer (LET) generally increases with decreasing particle energy. For example, 2.5 MeV alpha particles are less efficient than 4.0 MeV alpha particles even though the particles have a higher LET, this phenomenon is due to overkill.
A higher LET value will normally lead to the double strands in the tumours’ DNA to break. The maximum DNA breakage occurs when the LET value is between 100–200 keV/µm. This LET range is significant due to the ionisations approximating to 2 nm, which corresponds to the diameter of the DNA double-stranded helix.
Does the ‘radiometal’ bismuth-213 emit gamma radiation?
Bismuth-213 does emit gamma radiation during its decay mode.
Do you have to target the tumour at the site, or can you inject it anywhere in the body?
Bismuth-213 – which is generated from the actinium-225/bismuth-213 generator – is used in the field of nuclear medicine because of a favourable 46-minute half-life and high energy alpha particle emission. Bismuth-213 can be used to treat patients with leukaemia, lymphomas and metastatic cancers. The bismuth-213 is carried to the tumour ‘volume’ by a monoclonal antibody. The radiometal is attached to the antibody by using a metal chelator and via a linker. Hence, the targeting agent can be injected into the bloodstream but it is better to inject directly into the tumour. The bismuth-213 decays with the release of alpha particles, which are able to target the cancer cells and kills them.
Why are alpha particles better than, say, beta particles?
Alpha particles are positively charged with a mass and charge equal to the helium nucleus. The emission leads to a daughter nucleus with two protons and two neutrons less. Hence, alpha particles are highly charged ionised particles, compared to beta particles, which are smaller and have less charge (negatively charged) and ionising properties. Therefore, beta particles interact less with cancer cells and have a longer range than alpha particles through various materials.
What are the safety implications in the preparation, handling and patient administration of targeted radionuclide therapy?
To date, approximately 130 patients have been treated with targeted alpha therapy. The information gathered from these clinical trials has enabled favourable safety profiles for the administration of alpha emitters in patients. In addition, as a result of these clinical trials, the correct dosage levels (activity levels) have been formulated to treat a number of specific cancers.
For targeted alpha therapy to be widely used in Nuclear Medicine further investigations will be required into more efficient and practical means to generate the radiometal to be incorporated into radiopharmaceutical drugs. It will be necessary for further research and development in chelation chemistry, design of drug substrates, further clinical trials for different variants of cancers and transporting the radiometal (alpha emitters) to the tumour site.
What is a typical dose size for targeted alpha therapy?
A study has been carried out to establish the effective dose of the alpha-immuno-conjugate bismuth-213-DTPA-9.2.27. In a study of 22 patients with melanoma, the treatment was of the activity range of 55 MBq to 947MBq. This dose size proved to be safe with no adverse side effects during the clinical trials.
Disclaimer
This article is intended for informational and educational purposes only. The content provided does not constitute medical advice, diagnosis, or treatment recommendations. Targeted radionuclide therapy (TAT), including targeted alpha therapy (TAT-A), is an area of ongoing clinical research and should not be interpreted as a guaranteed or standardised cancer treatment.
The procedures, radiopharmaceuticals, and radionuclides described are subject to regulatory approvals, safety protocols, and clinical evaluation. While preliminary studies and limited clinical trials have shown potential benefits, the safety, efficacy, and long-term outcomes of TAT continue to be evaluated. Medical decisions should only be made in consultation with qualified healthcare professionals.
Open MedScience does not endorse or recommend any specific medical treatments, diagnostic methods, pharmaceutical products, or healthcare providers. Any mention of clinical outcomes, dosages, or treatment protocols reflects information available at the time of publication (08 December 2018) and may no longer represent current standards or regulatory guidance.
Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or treatment approach. Never disregard professional medical advice or delay seeking it based on content published by Open MedScience.
You are here: home » diagnostic medical imaging blog »