Radiotherapeutics has entered a period of rapid scientific, clinical, and technological advancement. The combination of precision radiopharmaceuticals, adaptive external-beam radiotherapy, integrated imaging, and novel systemic agents is reshaping how clinicians diagnose and treat cancer. Over the past few years, this field has shifted from incremental change toward a more significant transformation driven by targeted radionuclide therapies, emerging isotopes, AI-assisted workflows, and new clinical evidence. This article examines these developments and explores what they signal for the future of cancer care.
Expansion of Radiopharmaceutical Therapy
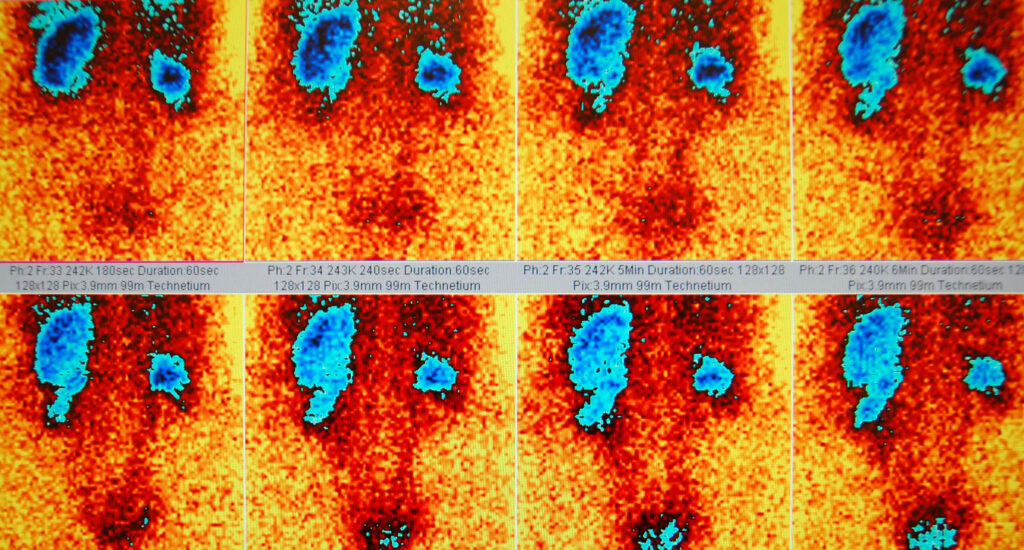
Radiopharmaceutical therapy (RPT) is experiencing a notable rise in both clinical use and the depth of research investment. Prostate cancer remains the most established indication, owing to the success of PSMA-targeted agents. The recent trial involving ¹⁷⁷Lu-PNT2002 in recurrent prostate cancer confirmed that introducing a PSMA-targeted lutetium therapy before stereotactic body radiotherapy can substantially prolong progression-free survival. Median progression-free survival nearly doubled, indicating that combining molecularly targeted radionuclides with local high-precision radiation could become a preferred approach.
Beyond prostate cancer, new RPT candidates are entering trials for neuroendocrine tumours, breast cancer, pancreatic cancer, and certain haematological malignancies. The phase 3 COMPETE trial, which evaluated ¹⁷⁷Lu-edotreotide for gastroenteropancreatic neuroendocrine tumours, continues to generate supportive data. These studies strengthen the position of lutetium-177 as a versatile therapeutic isotope with a favourable safety profile and predictable clinical behaviour.
At the same time, the industry is seeing an unusual level of activity in drug pipelines. Dozens of new radioligand therapies are being developed, many of which target biomarkers not previously exploited in cancer treatment. This growth reflects both scientific progress and expanding commercial confidence. It also signals that RPT is moving firmly into mainstream oncology rather than being confined to niche indications.
Growth in Novel Isotopes and Supply Chain Development
One of the most important areas of progress is the development of new therapeutic isotopes, particularly alpha emitters. Alpha-particle therapies have the potential to deliver high-energy, short-range radiation that produces lethal DNA damage within cancer cells while sparing surrounding tissue. Actinium-225 has emerged as a major focus because of its strong therapeutic potential, but reliable production remains a barrier. Recognising this, several collaborations and commercial partnerships have been announced recently to boost isotope supply. These include multi-isotope agreements between radiopharmaceutical developers and new accelerator-based suppliers.
Astatine-211 is also gaining attention. Research groups have been investigating strategies to stabilise astatine-labelled radiopharmaceuticals and expand their clinical viability. Progress in this area could provide the field with a new class of highly targeted alpha-emitting agents for indications such as breast cancer, glioma, and micro-metastatic disease.
In addition to alpha emitters, other isotopes, such as ⁶⁴Cu, ⁴⁷Sc, and radiocobalt variants, are being explored in theranostic frameworks. These isotopes offer dual imaging-and-treatment capabilities with physical characteristics that may suit specific tumour types.
Isotope supply is increasingly recognised as a strategic challenge. As demand rises, the global supply chain for key isotopes—including lutetium-177, actinium-225, and iodine-131—faces pressure. Investment in new production facilities, purification technologies, and waste-handling systems is now essential. Health systems and regulators are beginning to treat isotope supply as a component of national healthcare infrastructure rather than a niche scientific concern.
Advances in External-Beam Radiotherapy
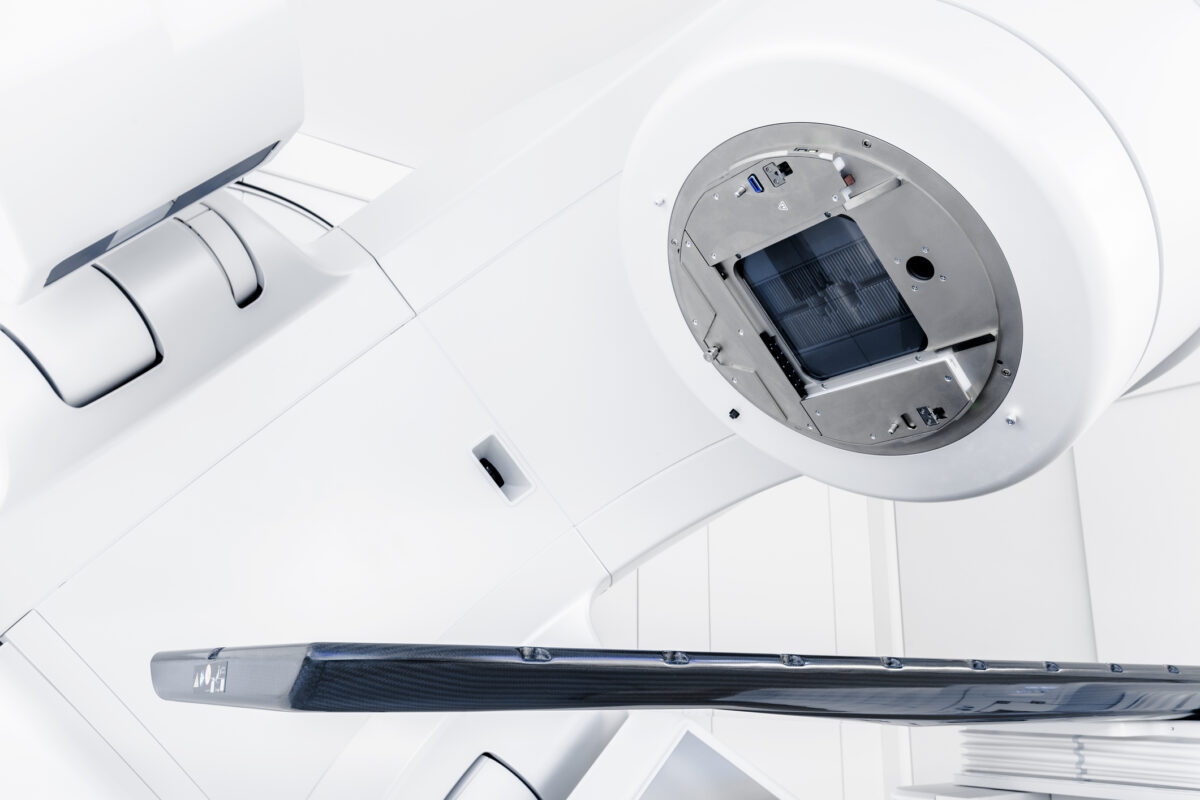
Although radiopharmaceuticals attract much attention, external-beam radiotherapy (EBRT) continues to innovate at a pace. The shift toward adaptive radiotherapy is one of the most influential recent developments. Adaptive radiotherapy involves adjusting a patient’s treatment plan based on daily imaging data, allowing clinicians to respond to anatomical changes or tumour shrinkage in near real time. Modern MR-guided systems are proving particularly valuable in lung, pancreatic, and pelvic cancers, where organ motion and tumour position vary significantly from day to day.
The integration of MR imaging into radiotherapy has led to more precise targeting and improved protection of healthy tissue. Recent studies in lung cancer illustrate how MR-guided radiotherapy can reduce toxicity without compromising tumour control. The adoption of five-dimensional CT (5D CT), which captures motion more comprehensively than earlier imaging methods, adds further accuracy. With enhanced data on tumour movement, clinicians can design treatment plans that anticipate breathing cycles and other physiological changes.
Proton therapy is another area benefiting from technological evolution. AI-supported workflows are beginning to streamline treatment planning, helping clinicians generate optimised proton plans more quickly. This improves workflow efficiency and may enhance plan quality, particularly in cases requiring highly conformal dose distributions.
Combination Therapies and Radiosensitisation
Combination treatments are becoming increasingly important as researchers seek to build synergistic effects between targeted radiation and systemic therapies. Radiotherapy can stimulate local and systemic immune responses, and there is growing interest in exploiting this interaction. In glioblastoma, for example, there is increasing exploration of radiotherapy combined with immunotherapy, including checkpoint inhibitors and cellular therapies. Although responses vary widely, the scientific rationale is strong, and research efforts continue.
New radiosensitising agents offer another promising avenue. These drugs are designed to make tumour cells more susceptible to radiation by interfering with DNA repair pathways, cell-cycle progression, or tumour hypoxia. Several candidates are in development, including molecules targeting the DNA damage response in cancer cells.
In addition, new antibody-radioconjugates are being engineered to bind to hypoxic regions within tumours. Hypoxia is a major cause of radiotherapy resistance, so agents that specifically target these areas could overcome a long-standing challenge in radiation oncology.
Combination therapy research also extends to radiopharmaceuticals. There is growing interest in pairing RPT with chemotherapy, immunotherapy, or radiosensitisers, especially for metastatic disease where systemic reach is essential. As clinical experience expands, this approach may reshape treatment algorithms for several cancers.
Implementation Challenges and Global Access
Rapid scientific progress does not automatically translate into widespread clinical availability. In radiotherapeutics, the gap between innovation and real-world implementation remains significant. Several barriers affect how quickly new treatments can reach patients. These include regulatory constraints, complex manufacturing needs, shortages of trained personnel, infrastructure gaps, and inconsistent reimbursement policies.
Radiotheranostics—where diagnostic imaging is paired with targeted therapy—requires seamless integration between nuclear medicine, radiology, oncology, radiopharmacy, and medical physics. Many healthcare systems still lack the necessary cross-disciplinary infrastructure. Training programmes for radiopharmaceutical handling, dosimetry, and safety are stretched, especially as new agents enter clinical practice at a steady pace.
On a global scale, disparities in access are stark. High-income countries are expanding radiopharmaceutical services, whereas many low- and middle-income nations lack basic radiotherapy infrastructure. International organisations are calling for expanded investment in treatment centres, isotope production, and specialist training. Without this, the benefits of the radiotherapeutic revolution will be unevenly distributed.
Artificial Intelligence and Personalised Dosimetry
Another major trend is the role of artificial intelligence. AI tools are being developed for dose prediction, image segmentation, treatment planning, and patient-specific dosimetry. In radiopharmaceutical therapy, dosimetry remains one of the most complex areas, as each patient’s metabolic and physiological characteristics influence absorbed dose. New AI-supported tools aim to simplify data processing, enabling more precise and personalised dose calculations.
Alongside AI, genomics is drawing interest. The concept of using genetic markers to predict tumour radiosensitivity—known as genomically adjusted radiation dose—could eventually help clinicians individualise treatment. Although this approach is still in its early stages, it highlights a growing shift toward biologically driven treatment decisions.
Outlook for the Future
Radiotherapeutics is evolving in several complementary directions. Radiopharmaceutical therapy is expanding into new tumour types with strong commercial and clinical momentum, while external-beam radiotherapy continues to benefit from advances in imaging, adaptive planning, and AI-driven optimisation. Novel isotopes are moving closer to mainstream use as supply-chain investment increases. Combination treatments offer fresh opportunities to address cancers that have long been difficult to manage through radiation alone.
At the same time, practical considerations cannot be overlooked. The field will only advance as quickly as its infrastructure allows. Workforce development, isotope availability, high-quality imaging, regulatory alignment, and interdisciplinary collaboration are essential components of progress. Organisations seeking to adopt new radiotherapeutic technologies must ensure they can support complex workflows safely and consistently.
Conclusion
The past few years have been marked by extraordinary progress across radiopharmaceuticals, imaging, computing, and external-beam radiotherapy. Together, these innovations are redefining the scope of radiotherapeutic medicine. The future will likely involve a more personalised, data-rich approach to treatment that combines targeted radionuclides, adaptive external-beam techniques, and systemic agents selected through biomarkers and genomic profiling. As this momentum continues, radiotherapeutics is poised to play an increasingly central role in modern oncology.
Disclaimer
This article is published for general informational and educational purposes only. It is intended to provide an overview of recent scientific, clinical, and technological developments in radiotherapeutics and does not constitute medical advice, clinical guidance, or a recommendation for any specific diagnostic or therapeutic approach.
The content reflects the state of research, clinical trials, and regulatory understanding at the time of publication. Radiotherapeutic agents, imaging techniques, combination strategies, and artificial intelligence tools discussed may be subject to ongoing investigation, regulatory review, or regional availability restrictions. Clinical outcomes, safety profiles, and best practices may vary depending on patient-specific factors, institutional expertise, and evolving evidence.
Healthcare professionals should rely on their own clinical judgement, current guidelines, and local regulatory approvals when making diagnostic or treatment decisions. Patients should consult qualified healthcare providers regarding any medical condition or treatment options.
Open MedScience makes no warranties regarding the completeness, accuracy, or applicability of the information presented and accepts no liability for actions taken based on this content.
home » blog » radiotherapeutics »