Summary: Artificial intelligence is transforming the way we view and interpret medical images. By identifying subtle patterns and microstructural changes that are invisible to the human eye, AI is enabling the earlier detection of cancers, neurodegenerative conditions, and cardiovascular disease. This article examines how these systems operate, provides real-world examples of their benefits, discusses their training and validation, and outlines the regulatory safeguards that ensure safe adoption. It also considers the importance of human–AI collaboration and the ethical principles needed to keep patient safety at the centre of innovation.
Keywords: Early disease detection, AI in medical imaging, Radiology AI, Regulatory frameworks, AI healthcare, Human-AI collaboration in diagnostics, Ethical AI in imaging.
The Next Frontier in Diagnosis
For decades, medical imaging has been the backbone of diagnosis and treatment planning. X-rays, CT scans, MRIs, and ultrasound allow clinicians to see what’s happening inside the body without making a single incision. However, with the aid of artificial intelligence, imaging is now entering an entirely new phase — one where algorithms can detect patterns far too subtle for the human eye, revealing signs of disease years before symptoms appear.
This is not science fiction. Across the UK and beyond, hospitals and research centres are integrating AI tools into radiology departments. The result is sharper detection, earlier intervention, and better chances of recovery.
Oncology — Seeing the Unseen
Cancer detection is one of the most active areas for AI in imaging. In breast screening, AI systems are trained to recognise microcalcifications and slight distortions in tissue structure that may signal early-stage tumours. These signs can be faint, sometimes blending into normal background tissue.
For example, in mammography, AI can work as a “second reader”, marking areas that deserve a closer look. In one UK hospital trial, the AI system identified a small group of microcalcifications that were missed during the initial human review. Subsequent testing confirmed it as an early carcinoma — caught early enough to allow for minimally invasive treatment.
Similar benefits are being seen in lung cancer detection, where AI reviews CT scans for small nodules. By comparing scans over time, it can detect tiny changes in size or density that might otherwise go unnoticed until much later.
Neurology — A New Weapon Against Alzheimer’s and Parkinson’s
Neurodegenerative diseases often develop silently for years. By the time symptoms like memory loss or movement difficulties appear, significant brain damage has already occurred. AI is helping to change that timeline.
Using advanced MRI analysis, AI can measure subtle changes in brain volume, the shape of the hippocampus, or even patterns of connectivity between brain regions. These changes can precede symptoms by several years.
Research projects in the UK are now combining AI analysis with large population datasets, enabling earlier risk identification. This could mean more time for interventions — whether lifestyle adjustments, medication, or experimental therapies — and, in the future, it might help select patients for clinical trials before disease symptoms develop.
Cardiovascular Imaging — Spotting Trouble Before It Strikes
Heart disease remains one of the biggest killers worldwide. AI-enhanced cardiovascular imaging is providing clinicians with a better opportunity to intervene before a crisis occurs.
In CT angiography, AI can measure vessel wall thickness and identify non-calcified plaque deposits, which can be a hidden risk for a heart attack. These plaques are often missed by traditional visual assessment, especially in busy clinical settings.
AI analysis of echocardiography (ultrasound of the heart) can also detect slight changes in heart muscle movement, which may indicate early cardiomyopathy or heart failure. By identifying these early, cardiologists can start treatments to slow progression and reduce the risk of sudden events.
How AI Learns to Read Images — Data, Validation, and Safety
Behind every successful AI imaging tool lies a large, carefully curated dataset. These datasets originate from multiple hospitals, scanners, and patient groups to ensure the system can accommodate variations in imaging quality, anatomy, and pathology.
The training process involves feeding the AI thousands of examples, each labelled by expert radiologists. Over time, the system learns the features that distinguish healthy from abnormal tissue.
Validation is critical. Once trained, the AI must be tested on completely new data — ideally from different hospitals — to prove it can work in unfamiliar settings. Some systems also undergo prospective clinical trials, where they are tested alongside standard care in real-time.
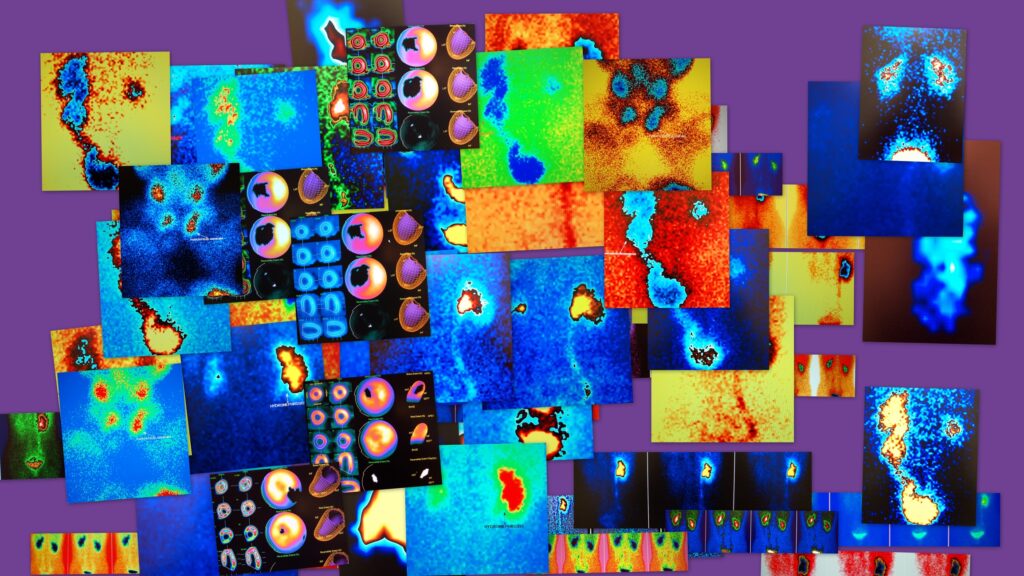
Importantly, interpretability tools, such as heatmaps or saliency maps, allow clinicians to see which part of the image influenced the AI’s decision. This transparency helps build trust and ensures AI is used responsibly.
Human–AI Collaboration — Why People Still Matter
Despite the power of AI, it is not a replacement for trained radiologists and clinicians. Instead, AI is most effective as a supportive tool — providing a safety net against human error, speeding up image review, and freeing up time for complex cases.
In breast screening programmes, for example, AI can filter out scans with no signs of disease, allowing radiologists to focus on the smaller percentage that may need more careful analysis. In emergency settings, AI can triage scans for suspected stroke, alerting doctors within minutes to cases needing urgent intervention.
When AI and human assessments differ, protocols are in place to review the case more closely, ensuring patient safety always comes first.
Regulation and Ethics — Keeping AI Accountable
In the UK, AI imaging tools are regulated as medical devices under the Medicines and Healthcare products Regulatory Agency (MHRA). Before they can be used in clinical practice, they must undergo safety and performance testing, and manufacturers must provide evidence of their effectiveness.
Regulation is not the only safeguard. Ethical principles are also crucial:
- Bias reduction — AI must perform effectively across diverse ethnicities, ages, and genders to mitigate health inequalities.
- Data protection — All patient data must be anonymised and stored securely, in compliance with the GDPR.
- Transparency — Patients and clinicians should be informed when AI is part of the diagnostic process.
- Responsibility — Clear accountability must be in place for decisions influenced by AI.
These measures ensure that innovation does not come at the expense of trust or patient welfare.
A Clearer View of the Future
AI in medical imaging is not just about faster diagnoses — it’s about finding problems before they become crises. From tiny breast cancer markers to early brain changes and hidden cardiovascular risks, AI is giving clinicians a sharper, earlier view of disease.
The success of this technology depends on three things: the quality of the data it learns from, the rigour of its testing, and its thoughtful integration into clinical workflows. When paired with the skill and judgement of human professionals, AI has the potential to reshape preventive healthcare, catching disease in its earliest stages and improving patient outcomes worldwide.
The future of imaging will not be AI alone — it will be AI working in tandem with expert clinicians, each enhancing the other’s capabilities. And as this partnership evolves, the focus will remain where it has always been: on delivering the best possible care to every patient.
Disclaimer
The information presented in Sharper Than Ever: How AI Is Transforming Early Detection in Medical Imaging is intended for general informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Readers should not rely solely on the content of this article when making decisions about their health or medical care. Always seek the guidance of a qualified healthcare provider with any questions regarding a medical condition or treatment options. References to specific technologies, products, or research studies do not constitute an endorsement by Open MedScience. While efforts have been made to ensure accuracy at the time of publication, Open MedScience makes no warranties regarding the completeness, timeliness, or reliability of the information provided. Use of any information from this article is at the reader’s own risk.