Elderly family members with limited English proficiency often struggle to communicate their symptoms, understand medical instructions, and receive appropriate care, putting their health at serious risk. This article examines the impact of language barriers on elderly healthcare, the consequences of miscommunication, and the strategies used to improve patient outcomes.
By exploring the challenges of implementing language solutions and potential policy improvements, this article provides insights that can help healthcare providers in continuing-care retirement communities offer better support for non-English-speaking senior residents. Understanding these issues can lead to more effective communication, reduced hospital readmissions, and improved quality of life for aging loved ones.
Keep reading to discover practical solutions that can help healthcare providers break language barriers and deliver safer, more inclusive healthcare.
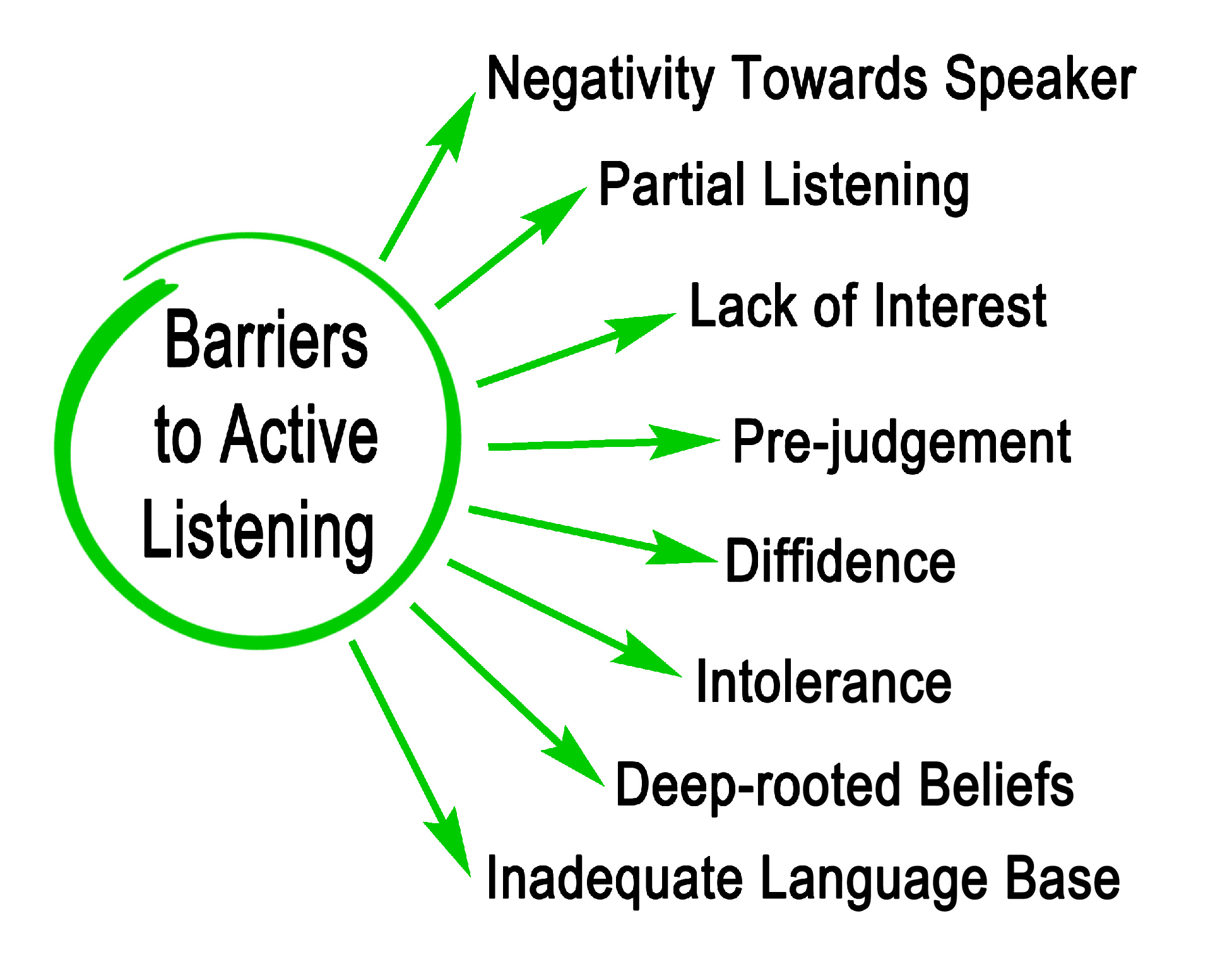
Understanding Language Barriers
Language barriers in senior healthcare occur when elderly patients with limited English proficiency struggle to communicate with medical providers, leading to misunderstandings about symptoms, treatments, and care instructions. Older adults face additional challenges, such as cognitive decline and hearing impairments, which make it even harder to learn a new language or use digital translation tools effectively.
Without clear communication, these non-English speaking seniors are at a higher risk of misdiagnosis, improper medication use, and increased hospital readmissions, ultimately compromising their overall health and well-being.
Consequences of Language Barriers
When elderly patients and healthcare providers cannot communicate effectively, it can lead to serious medical errors, delays in treatment, emotional distress, and worsening health outcomes.
Medical Errors and Misdiagnosis
Miscommunication can result in doctors misunderstanding symptoms, prescribing incorrect medications, or failing to diagnose serious conditions. Patients with limited English proficiency are more likely to experience medical errors because they struggle to describe their symptoms accurately or understand critical health information.
Delayed or Inappropriate Treatment
Without clear communication, medical treatment decisions may be delayed or based on incomplete or inaccurate information. This can lead to unnecessary procedures, ineffective medications, or missed opportunities to address urgent medical issues before they worsen.
Increased Patient Anxiety and Frustration
Elderly patients who can’t communicate effectively often feel excluded from their own care, leading to confusion, frustration, and stress. Over time, this can cause them to avoid seeking medical attention altogether, further deteriorating their health and increasing the risk of complications.
Higher Rehospitalization and Mortality Rates
Patients with language barriers face higher hospital readmission rates because they may not fully understand discharge instructions, medication regimens, or follow-up care. This lack of comprehension increases the likelihood of complications that require emergency care, ultimately raising mortality risks.
Difficulty in Managing Chronic Illnesses
Managing conditions like diabetes, heart disease, or hypertension requires clear instructions on medication use, dietary guidelines, and lifestyle changes. When language barriers prevent elderly patients from following their treatment plans correctly, their health conditions often worsen, leading to frequent hospital visits and lower quality of life.
Current Strategies for Overcoming Language Barriers
Healthcare providers use various strategies to improve communication with elderly patients who have limited English proficiency, but each approach comes with challenges that affect its effectiveness in different care settings.
Professional Medical Interpreters
Trained medical interpreters provide the most accurate and reliable communication between seniors and healthcare providers. Their knowledge of medical terminology ensures that symptoms, diagnoses, and treatment plans are conveyed clearly, reducing the risk of errors and misunderstandings.
Bilingual Healthcare Staff
Hiring bilingual doctors, nurses, and administrative staff allows healthcare or senior living facilities to provide immediate language support without relying on external interpreters. While this approach improves communication efficiency, it’s often limited by the availability of qualified professionals fluent in medical terminology and the senior’s native language.
Family Member Involvement
In many cases, elderly patients rely on family members to translate during medical visits, which can help bridge gaps when professional interpreters are unavailable. However, this approach carries risks, as family members may lack medical knowledge, omit critical details, or alter information based on personal interpretation.
Use of Digital Translation Tools
Translation apps and AI-driven tools offer on-demand language support, helping patients and providers communicate basic medical information. While these tools are improving, they still struggle with accuracy in complex medical discussions, making them an imperfect solution for critical healthcare decisions.
Challenges in Implementing Language Solutions
While various strategies help address language barriers in elderly healthcare, limited resources, lack of training, and concerns about accuracy make consistent and effective communication difficult.
Shortage of Qualified Interpreters
The demand for professional medical interpreters far exceeds the available supply, leaving many healthcare facilities and senior living communities without reliable language support. As a result, providers may have to rely on untrained staff or family members, increasing the risk of miscommunication with senior patients.
Limited Training for Healthcare Professionals
Many healthcare workers receive little to no training on how to communicate effectively with patients who have limited English proficiency. Without guidance on using interpreters, digital tools, or non-verbal communication strategies, providers may struggle to deliver accurate and patient-centered care.
Financial and Logistical Barriers
Hiring interpreters and bilingual staff requires funding that many healthcare facilities, especially smaller clinics and nursing homes, cannot afford. Additionally, scheduling professional interpreters or securing real-time translation support can be difficult, particularly in emergencies.
Reliability Concerns with Digital Translation Tools
While translation apps and AI-driven tools offer quick language support, they are not always accurate in translating, especially for medical terminology. Misinterpretations can lead to confusion about medications, procedures, or diagnoses, making these tools unreliable for critical healthcare decisions.
Future Directions and Policy Recommendations
Improving communication in elderly healthcare requires a combination of technological advancements, facility-based programs, policy changes, and provider education. The following solutions aim to address language barriers more effectively and create a safer, more inclusive healthcare system.
Advancing AI and Real-Time Translation Technology
AI-powered translation tools are improving, but they still struggle with medical terminology and contextual accuracy. Investing in more advanced real-time translation solutions, specifically made for healthcare settings, could help bridge communication gaps without relying solely on human interpreters.
Language Assistance Programs in Elderly Care Facilities
Continuing care retirement communities and nursing homes need dedicated language services to support residents with limited English proficiency. Implementing on-site interpreters, multilingual staff, and written resources in multiple languages can improve patient understanding and reduce medical errors.
Legislative and Policy Initiatives
Stronger policies can ensure healthcare facilities receive funding for interpreter services and language training programs. Expanding Medicare and Medicaid reimbursement for language assistance would make these services more accessible, particularly in underfunded healthcare settings.
Training on Cultural Competency
Healthcare providers need to also understand cultural differences that impact senior patient care. Training programs that focus on cultural competency can help providers navigate diverse healthcare beliefs, improving communication and patient trust.
Breaking Language Barriers to Improve Elderly Healthcare
Addressing language barriers in elderly healthcare is essential for reducing medical errors, improving patient outcomes, and ensuring seniors receive the care they need. Expanding interpreter services, integrating AI-driven translation tools, and implementing cultural competency training can help healthcare providers communicate more effectively with non-English-speaking patients.
By prioritizing these solutions, continuing-care retirement communities and healthcare facilities can create a safer, more inclusive environment where all seniors receive accurate, high-quality medical care.
Disclaimer
The content of this article is provided for informational purposes only and does not constitute medical, legal, or professional advice. Open Medscience makes every effort to ensure the accuracy and relevance of the information at the time of publication; however, healthcare practices and policies may vary and evolve over time. Readers are encouraged to consult qualified healthcare professionals regarding specific medical concerns or decisions. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any healthcare institution or regulatory body. Open Medscience does not accept responsibility for any loss or harm arising from reliance on the information presented.
home » blog » health and wellbeing »