Computed tomography (CT) has long been one of the most powerful diagnostic tools in modern medicine, enabling the visualisation of internal anatomy with remarkable detail. Yet, the technology is once again undergoing a significant shift. Hospitals and imaging centres across the world are now adopting advanced detector technologies, re-examining radiation risk, and rethinking how CT fits into a broader ecosystem of multimodal imaging and personalised care.
Recent developments in 2024 and 2025 highlight how far the modality has progressed — and how it continues to evolve in both clinical capability and safety.
From Energy-Integrating to Photon-Counting CT: A Technological Leap
For decades, CT scanners relied on energy-integrating detectors (EIDs), which measure the total energy of incoming X-ray photons. This method has proven highly effective, but it discards valuable information about individual photon energies. The emergence of photon-counting computed tomography (PCCT) represents a clear technological turning point.
Photon-counting detectors (PCDs) record each photon individually and measure its energy, allowing the scanner to distinguish between materials and tissues with far greater precision. Instead of integrating energy over a broad range, PCCT produces spectral or energy-resolved images directly from a single acquisition. The result is enhanced contrast resolution, reduced electronic noise, and improved differentiation between soft tissues and contrast agents.
In 2025, University Hospitals Health System in Cleveland became one of the first American institutions to install Siemens Healthineers’ Naeotom Alpha.Pro, a dual-source photon-counting CT system. Similar systems are now being tested in Europe and Asia, with several NHS Trusts reportedly evaluating PCCT as a potential replacement for older high-dose scanners.
These new systems are not only capable of producing higher-quality images at lower doses, but also allow clinicians to perform spectral imaging without switching protocols or performing dual-energy scans. The inherent energy discrimination of PCDs provides a continuous spectral range, simplifying workflows and reducing scan time.
For departments accustomed to hybrid imaging, such as PET/CT or SPECT/CT, photon-counting technology introduces exciting possibilities. It could allow better attenuation correction, more accurate tissue characterisation and, potentially, new radiopharmaceutical imaging methods that use CT-based spectral data for tracer mapping. For radiopharmacy teams, this might open opportunities to correlate CT-derived elemental data with molecular imaging, improving quantification and diagnostic reliability.
AI, Automation and Dose Optimisation
Artificial intelligence (AI) continues to reshape medical imaging, and CT scanning is among the fields most affected by its rapid advances. AI-driven dose modulation algorithms can now tailor the radiation output to each patient’s anatomy in real time, automatically adjusting tube current and voltage based on body size, region of interest, and diagnostic requirements.
These developments go beyond basic automatic exposure control. Modern AI systems learn from prior scans, build predictive models of optimal dose levels, and dynamically adapt reconstruction parameters during image acquisition. Combined with iterative and deep-learning-based reconstruction techniques, these tools maintain image clarity even when doses are significantly reduced.
Manufacturers such as Canon, GE HealthCare, and Siemens Healthineers have all incorporated AI-based dose management systems into their latest scanner models. The integration of machine learning into CT workflows also extends to automated organ segmentation, lesion detection and quality control, helping radiographers streamline their work and minimise rescans.
This is particularly relevant in an era of renewed scrutiny of radiation exposure. As recent studies suggest a measurable but modest increase in long-term cancer risk from CT imaging, dose optimisation is becoming a defining factor in scanner selection and protocol design.
Radiation Risk and the Push for Responsible Imaging
While the benefits of CT imaging are indisputable, the issue of radiation exposure continues to attract both scientific and public attention. A modelling study published in JAMA Internal Medicine in 2024 estimated that the 93 million CT exams performed annually in the United States could lead to approximately 103,000 future cancers if dose levels and utilisation remain unchanged. Though the figure represents a projection rather than a direct observation, it underscores the scale of the issue.
The study further estimated that CT-related cancers might account for up to five per cent of all new cancer cases if current trends continue. These findings have reignited calls for more judicious use of CT, especially in non-urgent or repetitive imaging where alternative modalities might suffice.
A separate investigation led by researchers at the University of Florida examined CT-related cancer risk in children and adolescents. It found a small but statistically significant increase in the incidence of blood cancers among those exposed to CT radiation during early life. However, the authors emphasised that for clinically justified scans, the diagnostic and therapeutic benefits outweigh the potential risks.
These findings have already influenced clinical and regulatory discussions. In the United States, new Medicare regulations require imaging centres to report radiation output data from their scanners, enabling greater transparency and benchmarking. The European Commission and the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) are also developing frameworks to harmonise dose-reporting standards and encourage dose tracking across institutions.
For imaging professionals, this means that justification, optimisation and dose recording are becoming as essential as image quality itself. Radiographers and medical physicists must now document radiation parameters, review multi-phase scanning practices, and ensure that each exposure is medically warranted.
Infrastructure Renewal and the Move Away from Mobile Units
Alongside technological advances, healthcare systems are investing heavily in infrastructure. In October 2025, the Queen’s Medical Center Wahiawa in Hawai‘i unveiled a new in-house CT suite, replacing a mobile unit that had served the community for years. This type of investment reflects a broader trend: moving from temporary or relocatable scanners to dedicated, high-performance CT rooms that can handle increased patient throughput and advanced protocols.
In the UK, similar projects are underway. Many NHS Trusts have begun replacing older CT systems with dual-source or spectral-capable units to expand capacity, particularly in cardiac and vascular imaging. Mobile scanning units still provide vital flexibility — especially for rural areas or during refurbishment — but the long-term goal is clear: permanent installations with modern shielding, ventilation, and workflow integration.
Upgrading CT equipment has operational consequences. Installation often requires architectural modification, new radiation protection assessments, and staff retraining. However, these investments yield tangible benefits in image quality, speed, and patient comfort. Faster rotation times and larger detectors enable full-body scans in seconds, reducing motion artefacts and improving diagnostic accuracy in emergency and trauma cases.
The Role of CT in Hybrid and Multimodal Imaging
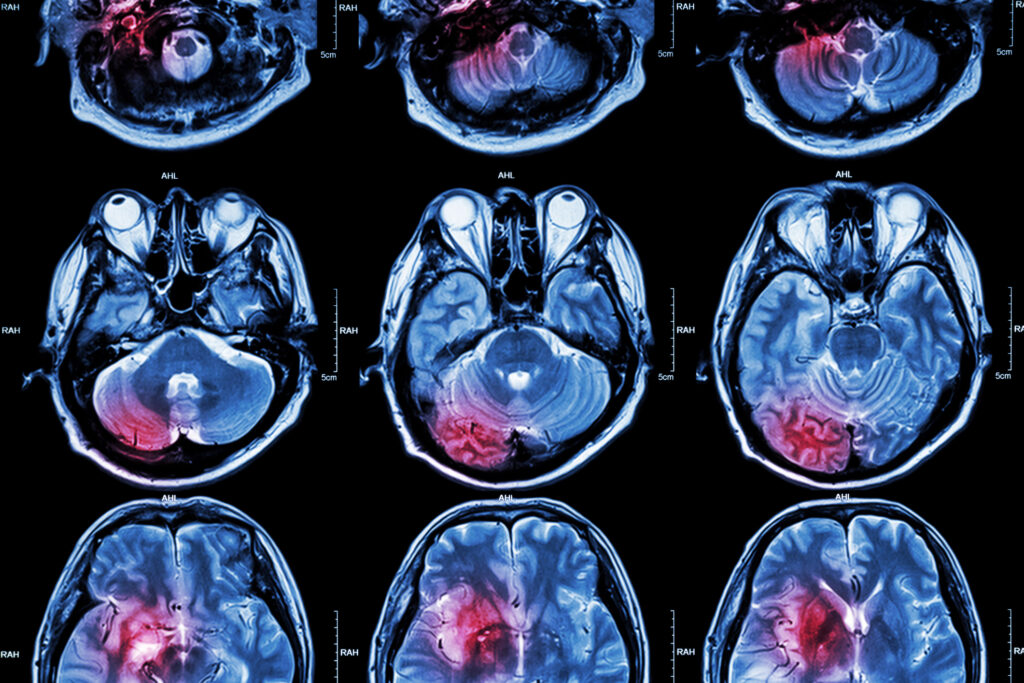
CT is no longer a stand-alone modality. In oncology, cardiology, and neurology, it forms part of multimodal systems that combine anatomical and functional information. PET/CT and SPECT/CT scanners are standard in nuclear medicine, while MR/CT fusion is increasingly used in radiotherapy planning.
As photon-counting and spectral imaging mature, CT may contribute even more precise attenuation correction and material discrimination in hybrid systems. This has implications for radiopharmaceutical design and image harmonisation — crucial factors when comparing PET/CT data across centres or trials.
Hybrid imaging also enables advanced theranostic approaches, where CT provides structural mapping for targeted radionuclide therapy. For instance, improved contrast differentiation could support dosimetry calculations by defining tumour boundaries with greater precision.
For laboratories involved in tracer development and molecular imaging research, understanding the evolving capabilities of CT is vital. The scanner is not merely a companion modality for attenuation correction; it is a data source in its own right, offering insights into tissue composition that complement radiopharmaceutical uptake patterns.
Training, Workflow and Quality Assurance
The adoption of next-generation CT scanners introduces both opportunities and responsibilities. Staff training must now include knowledge of spectral reconstruction, photon-counting detector principles, and AI-assisted workflow tools. Dose optimisation strategies must be revisited, especially when transitioning from legacy scanners with different calibration and performance profiles.
Quality assurance (QA) remains central to safe operation. Regular phantom testing, calibration, and image uniformity checks are essential to maintain diagnostic reliability. Facilities upgrading to photon-counting or dual-source systems will also need to update QA protocols to accommodate the spectral and high-resolution capabilities of these scanners.
Laboratory and hospital managers should also anticipate the need to revise standard operating procedures (SOPs), including documentation for dose benchmarking and cross-modality comparisons. Integration with hospital information systems and Picture Archiving and Communication Systems (PACS) must be verified to ensure seamless data transfer, particularly for research and multi-centre collaboration.
Addressing the Broader Implications
Beyond the technical and operational aspects, the evolution of CT technology has broader implications for healthcare policy and clinical decision-making. As imaging becomes faster, more detailed and more automated, there is a growing risk of overuse. Easy access to high-resolution imaging can lead to unnecessary scans that add little to patient management while contributing to cumulative dose exposure.
Balancing access with responsibility requires clear clinical guidelines, multidisciplinary collaboration, and continuous audit. National dose reference levels (DRLs), such as those maintained by Public Health England, play a vital role in maintaining safe practice. Hospitals should ensure that their mean CT doses remain within recommended ranges and review any outliers through regular audit cycles.
For researchers and publishers in medical imaging, these issues provide fertile ground for discussion. Topics such as dose justification, spectral imaging in oncology, and AI-assisted CT protocol design are likely to shape the next wave of academic and clinical discourse.
Looking Ahead
The pace of CT innovation shows no sign of slowing. Photon-counting technology is only the beginning; future systems may integrate quantum detectors, AI-driven real-time reconstruction, and ultra-fast gantry designs capable of continuous helical scanning at near-real-time speeds.
Manufacturers are already exploring how CT can contribute to precision medicine by quantifying tissue biomarkers and mapping perfusion or microcalcification patterns that were once invisible to conventional systems. In parallel, ongoing studies into radiation risk and optimisation are ensuring that these advances do not come at the cost of patient safety.
As imaging laboratories, hospitals, and regulatory bodies adapt, the focus will remain on achieving the best diagnostic yield at the lowest possible dose—an ethos that aligns perfectly with the broader goals of sustainable, patient-centred healthcare.
Conclusion
Computed tomography has entered a new phase defined by photon-counting detectors, artificial intelligence, and an unwavering emphasis on safety. The scanner room, once a static space filled with whirring machinery, is now a highly intelligent environment where every photon counts — literally and figuratively.
For clinicians, radiographers and imaging scientists, these developments signal a shift towards more precise, informative and responsible imaging. For radiopharmacy and molecular imaging professionals, they open doors to closer integration between anatomical and functional data. And for patients, they promise faster, safer and more accurate diagnosis.
CT has always been at the centre of diagnostic imaging. In 2025 and beyond, it will continue to redefine what “seeing inside the body” truly means — not just in sharper images, but in smarter, safer, and more meaningful scans.
Disclaimer
The content presented in The New Era of Computed Tomography: Photon-Counting, Precision and Patient Safety by Open MedScience is provided for general informational and educational purposes only. It does not constitute medical, scientific, technical, or professional advice, and should not be used as a substitute for consultation with qualified healthcare professionals, medical physicists, or imaging specialists.
Open MedScience makes no representations or warranties regarding the accuracy, completeness, or current validity of the information contained in this article. While every effort has been made to ensure factual accuracy at the time of publication, advances in technology and evolving clinical guidelines may render some information outdated or subject to change.
Any mention of manufacturers, institutions, or commercial systems, including but not limited to Siemens Healthineers, GE HealthCare, Canon Medical Systems, or specific healthcare facilities, is for illustrative purposes only and does not imply endorsement or affiliation.
Readers are advised to exercise their own professional judgement and to refer to official regulatory guidance, peer-reviewed research, and institutional protocols when interpreting or applying any information from this publication. Open MedScience and its contributors accept no responsibility for any loss, damage, or adverse outcome arising from reliance on material contained herein.
home » blog » medical imaging modalities »