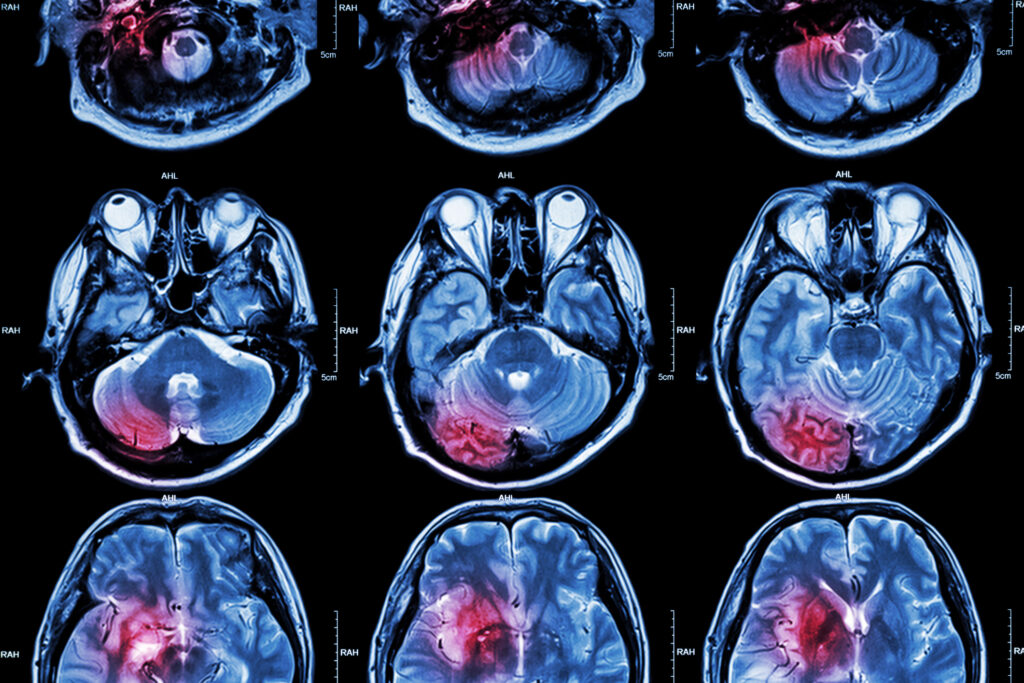
Summary: Magnetic resonance imaging (MRI) remains the cornerstone of diagnosing and monitoring multiple sclerosis (MS), a chronic inflammatory demyelinating disease of the central nervous system. Over the past two decades, advances in MRI sequences have transformed our understanding of disease mechanisms, improved diagnostic accuracy, and enhanced the monitoring of disease progression and treatment response. New imaging techniques such as magnetisation transfer imaging, diffusion tensor imaging, susceptibility-weighted imaging, myelin water imaging, and ultra-high-field MRI have enabled detailed visualisation of microstructural and biochemical changes beyond conventional T1- and T2-weighted imaging. These developments offer deeper insights into demyelination, neurodegeneration, and remyelination, contributing to more precise disease characterisation and potentially guiding personalised therapeutic strategies. This article explores how advanced MRI sequences have reshaped clinical and research approaches to MS, their diagnostic and prognostic value, and their implications for future practice.
Keywords: Multiple sclerosis, magnetic resonance imaging, demyelination, neurodegeneration, diffusion tensor imaging, magnetisation transfer imaging.
Introduction
Multiple sclerosis (MS) is a chronic, immune-mediated disease characterised by inflammation, demyelination, axonal injury, and neurodegeneration within the central nervous system (CNS). It is the most common non-traumatic neurological cause of disability in young adults, affecting more than 2.8 million people globally. The disease course is heterogeneous, often beginning with a relapsing-remitting phase before progressing to secondary progressive MS, although some patients exhibit a primary progressive course from onset. Early diagnosis and effective disease monitoring are essential for optimising therapeutic outcomes and improving long-term prognosis.
Magnetic resonance imaging (MRI) has revolutionised the clinical management of MS since its introduction in the 1980s. Conventional MRI sequences, including T1-weighted, T2-weighted, proton density, and fluid-attenuated inversion recovery (FLAIR) imaging, remain fundamental for detecting focal white matter lesions and fulfilling diagnostic criteria. However, these sequences provide limited information on the pathological substrates underlying lesion formation, tissue repair, and neurodegeneration. They also correlate poorly with clinical disability, a phenomenon known as the “clinico-radiological paradox”.
In response, a range of advanced MRI techniques has been developed to probe microstructural, biochemical, and functional changes in MS beyond what is visible on standard imaging. These novel approaches are reshaping the understanding of disease mechanisms, enhancing diagnostic specificity, and offering biomarkers for disease activity and progression, while also highlighting their growing importance in diagnosis, disease monitoring, and future clinical applications.
Limitations of Conventional MRI in Multiple Sclerosis
Conventional MRI sequences remain indispensable for identifying demyelinating lesions and guiding clinical decisions, yet they are constrained by several limitations. T2-weighted imaging is highly sensitive to white matter lesions but lacks specificity for underlying pathology, as hyperintensities can represent inflammation, demyelination, oedema, gliosis, or axonal loss. T1-weighted imaging can detect chronic “black holes” associated with severe tissue damage but provides limited sensitivity for early changes or subtle tissue injury.
Another significant limitation is the inadequate characterisation of grey matter pathology. While MS has historically been regarded as a white matter disease, grey matter demyelination and neuronal loss are now recognised as key contributors to disease progression and disability. Conventional MRI is poorly suited to detecting cortical lesions, which are often small, subtle, and lack the inflammation and blood–brain barrier disruption seen in white matter lesions.
Furthermore, standard imaging metrics such as lesion load correlate only modestly with clinical outcomes. Many patients with substantial lesion burden remain relatively asymptomatic, while others with fewer lesions experience severe disability. This discrepancy underscores the need for imaging approaches that capture the full spectrum of MS pathology, including diffuse microstructural damage, neurodegeneration, and remyelination.
Magnetisation Transfer Imaging: Probing Myelin Integrity
Magnetisation transfer imaging (MTI) is an advanced technique that measures the exchange of magnetisation between protons bound to macromolecules, such as myelin, and free water protons. The resulting magnetisation transfer ratio (MTR) reflects the density of macromolecules and is particularly sensitive to myelin content.
MTI has provided critical insights into demyelination and remyelination processes in MS. Lesions typically exhibit reduced MTR values compared with normal-appearing white matter (NAWM), indicating myelin loss. Moreover, MTR can detect subtle changes in NAWM and grey matter that appear normal on conventional MRI, revealing diffuse pathology and helping to explain clinical disability beyond focal lesion burden.
Importantly, MTI is sensitive to remyelination. Increases in MTR over time suggest myelin repair, offering a non-invasive biomarker for remyelination and therapeutic response. This feature has significant implications for evaluating emerging remyelinating treatments and assessing disease modification beyond anti-inflammatory effects.
While MTI is not yet part of routine clinical practice due to technical complexity and variability in acquisition protocols, ongoing research aims to standardise its use and validate it as a biomarker for clinical trials and patient monitoring.
Diffusion Tensor Imaging: Mapping Microstructural Integrity
Diffusion tensor imaging (DTI) is a powerful technique that quantifies the diffusion of water molecules within tissue, providing information about microstructural organisation. Metrics such as fractional anisotropy (FA) and mean diffusivity (MD) reflect axonal integrity and myelination, making DTI highly relevant to MS pathology.
DTI has revealed extensive microstructural damage in both lesions and normal-appearing tissue. Reductions in FA and increases in MD within white matter lesions reflect demyelination, axonal injury, and gliosis. In NAWM, DTI abnormalities correlate with cognitive impairment and disability progression, suggesting that diffuse damage beyond focal lesions contributes significantly to clinical outcomes.
Moreover, DTI has demonstrated its value in assessing grey matter pathology. Cortical and deep grey matter structures, including the thalamus and hippocampus, show altered diffusion metrics in MS, correlating with cognitive decline and disease progression. These findings underscore the importance of grey matter involvement in MS and highlight the potential of DTI as a biomarker for neurodegeneration.
DTI also offers insights into treatment effects. Studies have shown stabilisation or improvement of diffusion metrics following disease-modifying therapies, suggesting that DTI could serve as a marker of treatment response and neuroprotection.
Despite these advantages, DTI is sensitive to motion and distortion artefacts and requires careful standardisation for clinical application. Advances in acquisition and post-processing techniques are improving its robustness and reliability, bringing it closer to routine clinical use.
Susceptibility-Weighted Imaging: Visualising Iron Deposition and Veins
Susceptibility-weighted imaging (SWI) exploits differences in magnetic susceptibility between tissues to enhance contrast and detect paramagnetic substances such as iron. It is particularly useful for visualising veins, microbleeds, and iron accumulation — features increasingly recognised as relevant to MS pathology.
One of the most significant contributions of SWI is the identification of the “central vein sign”, a small vein visible within white matter lesions. This sign reflects the perivenular inflammation characteristic of MS. It has emerged as a potential diagnostic biomarker to distinguish MS from mimicking conditions such as small vessel disease or neuromyelitis optica spectrum disorders. The presence of a central vein in more than 40% of lesions is highly suggestive of MS, and ongoing research is exploring its integration into diagnostic criteria.
SWI also provides insights into iron accumulation in deep grey matter structures, including the basal ganglia and thalamus. Abnormal iron deposition is associated with neurodegeneration and disease progression, although its precise role remains under investigation. Quantitative susceptibility mapping (QSM), an extension of SWI, offers more precise quantification of susceptibility changes and is being explored as a biomarker for neurodegeneration and treatment response.
The ability of SWI to capture vascular and iron-related changes adds an important dimension to MS imaging, potentially enhancing diagnostic specificity and providing new markers of disease activity.
Myelin Water Imaging: Direct Assessment of Myelin Content
Myelin water imaging (MWI) is an emerging MRI technique that directly measures the fraction of water trapped between myelin bilayers, known as the myelin water fraction (MWF). This measure provides a more specific indicator of myelin content than indirect methods such as MTI or DTI.
MWI has shown strong potential in characterising demyelination and remyelination in MS. Lesions exhibit significantly reduced MWF, and partial recovery over time suggests remyelination. Importantly, MWI can detect changes in NAWM and grey matter, indicating widespread myelin loss beyond visible lesions.
One of the strengths of MWI is its quantitative nature, offering a direct measure of myelin content that can be tracked longitudinally. This capability is valuable for assessing disease progression, evaluating therapeutic efficacy, and exploring the dynamics of myelin repair.
While technical challenges, including long acquisition times and complex data analysis, have limited its widespread adoption, advances in acquisition protocols and reconstruction algorithms are improving feasibility. As these developments mature, MWI is likely to become an important tool for studying myelin dynamics and guiding remyelination therapies.
Ultra-High-Field MRI: Enhancing Sensitivity and Resolution
The advent of ultra-high-field MRI (7 Tesla and above) has opened new possibilities for MS imaging by providing increased signal-to-noise ratio and spatial resolution. These improvements enable the detection of subtle lesions, microstructural changes, and cortical pathology that are invisible at conventional field strengths.
Ultra-high-field MRI has significantly improved visualisation of cortical lesions, which are often under-detected on 1.5T or 3T scanners. Enhanced resolution allows for a more accurate assessment of cortical demyelination, which is closely associated with cognitive impairment and progressive disease. This improved detection capability contributes to a more comprehensive understanding of MS pathology and may inform prognosis and therapeutic decisions.
Additionally, ultra-high-field MRI enhances the visibility of the central vein sign and iron deposition, improving diagnostic specificity and enabling more detailed investigation of vascular and neurodegenerative changes. It also facilitates advanced quantitative imaging techniques, including QSM, MTI, and MWI, with greater precision and sensitivity.
Despite its promise, ultra-high-field MRI faces practical challenges, including cost, availability, and regulatory approval. Safety considerations, particularly in patients with implants, and technical issues such as increased susceptibility to artefacts, must also be addressed. Nevertheless, as technology advances and becomes more widely accessible, ultra-high-field MRI is expected to play an increasing role in both research and clinical practice.
Integration of Advanced MRI Sequences in Clinical Practice
Although advanced MRI techniques offer significant promise, their integration into routine clinical practice remains limited. Technical complexity, variability in acquisition protocols, and the need for specialised post-processing present barriers to widespread adoption. Moreover, standardisation across centres is essential for reliable interpretation and clinical utility.
Efforts are underway to address these challenges. International collaborations and consensus initiatives aim to develop standardised protocols and establish normative data for advanced imaging metrics. Incorporating these techniques into multicentre clinical trials will further validate their utility and accelerate translation into clinical practice.
Advanced MRI also has the potential to inform personalised treatment strategies. Imaging biomarkers that reflect demyelination, neurodegeneration, or remyelination could guide therapeutic decisions, monitor treatment response, and identify patients at risk of progression. Combining advanced MRI data with other biomarkers, such as neurofilament light chain or optical coherence tomography, could further enhance disease characterisation and management.
Artificial intelligence (AI) and machine learning are expected to play a crucial role in this transition. Automated analysis tools can process complex imaging data, extract quantitative metrics, and identify imaging patterns associated with clinical outcomes. These developments will help bridge the gap between research and clinical application, enabling advanced MRI to become an integral part of MS care.
Future Directions and Emerging Techniques
The field of MRI in MS continues to evolve rapidly, with ongoing research focused on refining existing techniques and developing new approaches. Multiparametric imaging, which combines complementary MRI metrics, offers a comprehensive assessment of tissue pathology and may improve diagnostic accuracy and prognostic power.
Advanced diffusion models beyond DTI, such as neurite orientation dispersion and density imaging (NODDI), provide more specific information about axonal architecture and dendritic complexity. Similarly, MR spectroscopy offers insights into metabolic changes associated with neuroinflammation and neurodegeneration, while functional MRI explores alterations in brain connectivity and network dynamics.
Integration of MRI with other imaging modalities, such as positron emission tomography (PET), is another promising direction. Hybrid PET-MRI systems enable simultaneous assessment of structural, functional, and molecular changes, offering a more complete picture of MS pathology.
As imaging technology continues to advance, these innovations will deepen understanding of MS pathophysiology, improve early diagnosis, and guide the development of targeted therapies.
Conclusion
Advances in MRI technology have transformed the landscape of multiple sclerosis imaging, expanding the capabilities of clinicians and researchers beyond the limitations of conventional sequences. Techniques such as magnetisation transfer imaging, diffusion tensor imaging, susceptibility-weighted imaging, myelin water imaging, and ultra-high-field MRI offer powerful tools for probing myelin integrity, axonal structure, vascular pathology, and neurodegeneration with unprecedented sensitivity and specificity.
These developments have enriched our understanding of MS as a complex disease involving inflammation, demyelination, and neurodegeneration in both white and grey matter. They also hold significant potential for improving diagnosis, monitoring disease activity, and assessing therapeutic response. While technical and logistical challenges remain, ongoing efforts to standardise protocols, validate biomarkers, and harness computational tools are paving the way for broader clinical adoption.
As the field progresses, advanced MRI is poised to become a central component of personalised MS care, guiding treatment decisions and enabling early interventions that improve patient outcomes. The continued evolution of imaging technology promises not only to enhance clinical practice but also to unlock new insights into the pathophysiology of multiple sclerosis, ultimately advancing the quest for more effective therapies and, ultimately, a cure.
Disclaimer
The information presented in The Role of Advanced Magnetic Resonance Imaging Sequences in Multiple Sclerosis is provided for educational and informational purposes only. It is not intended to replace professional medical advice, diagnosis, or treatment. Clinicians should rely on their own expertise and clinical judgement when interpreting imaging findings and making decisions about patient care. Patients should always seek the advice of qualified healthcare professionals regarding any medical condition or treatment. Open MedScience makes no representations or warranties about the accuracy, completeness, or applicability of the information contained in this article and accepts no liability for any loss, injury, or damage arising from its use.