This article explores the transformative impact of AI in radiology. It discusses how AI technologies enhance diagnostic accuracy, improve workflow efficiency, and contribute to personalised patient care. The discussion includes the integration of AI in image analysis, the challenges faced during its implementation, and the future potential of AI-driven innovations in this medical field. Overall, this analysis highlights the significant benefits AI brings to radiology, alongside the ethical considerations and the need for ongoing professional development to optimise its use.
1. Introduction to AI in Radiology
Artificial Intelligence (AI) has become a cornerstone of innovation across multiple sectors, fundamentally altering industries’ operations. Nowhere is this more evident than in healthcare, where AI has ushered in a new era of enhanced efficiency, accuracy, and patient outcomes. Among the various specialties within healthcare, radiology stands out as a prime beneficiary of AI advancement. This section will explore the role of AI in radiology, illustrating how it has redefined the landscape of diagnostic medicine and patient care management.
Radiology, fundamentally reliant on imaging to diagnose and manage patient treatment, has historically been at the forefront of adopting technological innovations. The advent of AI in radiology marks a critical evolution, enhancing both the capabilities and the reach of radiologic practices. AI algorithms, designed to process and interpret vast amounts of imaging data with precision, assist radiologists by highlighting areas of concern and reducing the likelihood of human error. This capacity not only speeds up diagnosis but also significantly increases diagnostic accuracy.
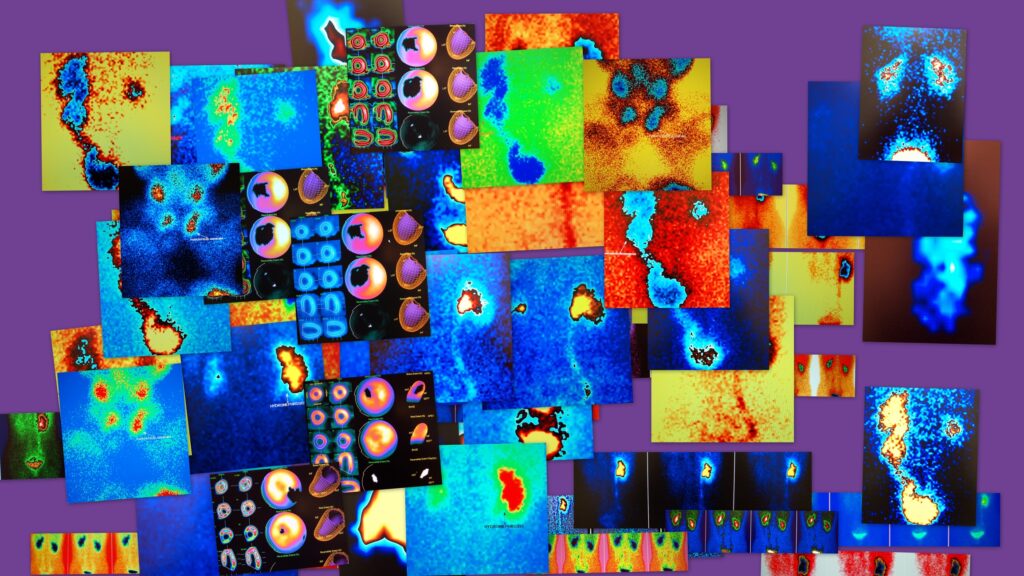
The integration of AI into radiology can be seen in various forms. One of the most significant applications is in the analysis of imaging, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans. AI systems equipped with deep learning algorithms excel in detecting patterns and anomalies that may be invisible to the human eye. For instance, in cases of subtle fractures or early signs of malignancy, AI can provide a second, highly reliable opinion, ensuring that no pathological detail is overlooked.
Furthermore, the impact of AI on radiology extends beyond diagnostic accuracy. It plays a crucial role in improving workflow efficiency within radiological departments. Through automation of routine tasks such as sorting and annotating images, AI frees up radiologists to concentrate on more complex cases and direct patient interactions. This optimisation of workflow not only enhances productivity but also reduces the waiting times for patients, thereby improving the overall patient experience.
AI also contributes to the standardisation of diagnostic practices in radiology. By providing consistent readings, AI minimises the variability that can occur with different radiologists’ interpretations. This standardisation is crucial for ensuring that patients receive the same quality of care regardless of who reads their images. It also aids in training and educating new radiologists, offering them a reliable benchmark against which to measure their interpretations.
Moreover, the role of AI in radiology is not static but continually evolving. As AI technologies advance, they are increasingly integrated into more complex diagnostic tools, such as predictive analytics, which forecast potential health outcomes based on imaging data. This capability enhances the proactive management of diseases and tailors treatment plans to individual patients, thereby advancing personalised medicine.
Therefore, the introduction of AI into radiology represents a transformative shift with far-reaching implications. As AI continues to evolve, its potential to further enhance diagnostic accuracy, workflow efficiency, and personalised patient care remains vast. This opening discussion sets the stage for a deeper examination of the role of AI in transforming radiology. This exploration is essential for understanding how technology is reshaping healthcare delivery. The following sections will look into specific applications, challenges, and the future prospects of AI in radiology, providing a comprehensive overview of this dynamic field.
2. Enhancing Diagnostic Accuracy
Artificial Intelligence (AI) has proven to be a powerful tool in the field of radiology, particularly in enhancing diagnostic accuracy. The core strength of AI lies in its superior pattern recognition capabilities, which allow it to detect subtle anomalies in medical images that the human eye might miss. By integrating AI tools into radiological practices, the accuracy and reliability of diagnoses are significantly improved, leading to better patient outcomes.
AI algorithms are particularly adept at analysing images from X-rays, CT and MRI scans. These tools apply complex mathematical models and learning algorithms to large datasets of imaging files to study and predict patterns associated with specific diseases. For example, in the case of chest X-rays, AI has been trained to identify signs of conditions such as pneumonia, tuberculosis, and lung cancer with a level of precision that matches or exceeds that of experienced radiologists.
One of the landmark studies in this area demonstrated that an AI system could detect breast cancer from mammography scans with greater accuracy than human radiologists. The system reduced false negatives, where cancer is present but missed by the radiologist, and also decreased false positives, where cancer is not present but is reported as such. These improvements are crucial as they potentially lead to earlier interventions and reduce unnecessary anxiety and procedures for patients wrongly diagnosed.
The capabilities of AI extend beyond common diseases; for example, in neurology, AI algorithms are used to interpret brain MRIs to detect and characterise strokes, brain tumours, and neurodegenerative diseases. For instance, AI systems can quantify changes in brain volume and structure faster and more accurately than traditional methods, aiding in the early diagnosis and monitoring of diseases such as Alzheimer’s and Parkinson’s.
Furthermore, AI enhances diagnostic accuracy through its application in cardiology. AI-powered tools analyse cardiac imaging to detect abnormalities such as myocardial infarctions (heart attacks) and heart failure. These tools can evaluate heart function by measuring ejection fraction, wall motion, and other parameters more consistently than even the most trained eyes.
The precision of AI in oncology, particularly in detecting and staging various cancers, has also been groundbreaking. AI algorithms analyse images to detect tumours, define their boundaries, and accurately assess the affected tissues. This precision is vital for diagnosis and planning treatment strategies, such as surgery or radiation therapy, where understanding the exact location and extent of the tumour is critical.
The integration of AI in radiology also addresses some of the inherent limitations of human diagnostics, such as fatigue and variability in diagnostic performance. AI systems maintain the same level of performance regardless of the time of day or the number of images they have analysed, providing a consistent quality of review that augments the radiologist’s capabilities.
Regardless of these advancements, the implementation of AI in enhancing diagnostic accuracy is not without challenges. Issues such as data privacy, the need for extensive datasets for algorithm training, and the integration of AI systems into existing healthcare workflows must be addressed. Additionally, there is a need for continuous validation and monitoring of AI tools to ensure their efficacy and safety in clinical settings.
Therefore, the role of AI in enhancing diagnostic accuracy in radiology is profound and expanding. As AI tools become more refined and widely adopted, they promise not only to improve the accuracy of diagnoses but also to revolutionise the way radiological healthcare is delivered, making it safer, faster, and more patient-centric. The following sections will explore how AI impacts other aspects of radiology, such as workflow efficiency and personalised patient care.
3. Improving Workflow Efficiency
In the fast-paced environment of medical diagnostics, the efficiency of radiology departments is crucial to hospital operations and patient care. Artificial Intelligence (AI) has emerged as a key enabler in optimising these workflows, significantly reducing the time from imaging to diagnosis and allowing radiologists to focus on more complex and critical tasks. This section looks into the various ways AI streamlines operations in radiology, demonstrating its profound impact on reducing diagnostic delays and enhancing patient throughput.
One of the primary ways AI improves workflow efficiency is through the automation of routine tasks. For example, image sorting and preliminary analysis are time-consuming activities that AI can manage swiftly and accurately. AI systems are trained to organise and prioritise imaging studies based on urgency and complexity. This means that cases requiring an immediate attention, such as potential strokes or fractures, are quickly escalated to the top of the work queue. This prioritisation ensures that critical cases are attended to promptly, improving outcomes for patients with urgent needs.
Moreover, AI enhances the efficiency of image analysis itself. Advanced algorithms can first review the scans, flag potential abnormalities and annotate key features. This preliminary analysis assists radiologists by highlighting areas of interest, thereby reducing the time they spend on each scan. For example, in mammography, AI algorithms can detect microcalcifications and masses, drawing the radiologist’s attention directly to these areas. This speeds up the review process and reduces fatigue-related errors, as the radiologist does not need to scan the entire image extensively.
The impact of AI on workflow efficiency extends beyond image analysis. AI tools also contribute to report generation, another time-intensive aspect of radiology. Natural language processing (NLP) applications within AI systems can help draft radiology reports by extracting key findings from the annotated images and integrating them into a structured report format. The radiologist can then review and finalise these draft reports, significantly cutting down report turnaround times and allowing for faster communication with referring physicians.
The role of AI in improving workflow efficiency also includes the management of follow-up tasks. Systems can be programmed to track and schedule follow-up imaging for patients, ensuring continuity of care and adherence to treatment protocols. By automating these administrative tasks, radiologists and other staff are freed up to concentrate on direct patient care activities, enhancing the overall efficiency and effectiveness of the service provided.
The introduction of AI-driven workflow enhancements also has broader implications for departmental management and resource allocation. With AI handling routine and repetitive tasks, radiology departments can optimise their staffing models. Radiologists can manage larger volumes of cases without compromising the quality of care, leading to better resource utilisation and potentially reducing wait times for patients.
However, the integration of AI into radiology workflows is not without its challenges. Issues such as interoperability with existing hospital information systems, data security, and the initial cost of implementation must be addressed. Additionally, radiology staff must train and adapt to work effectively with AI systems.
Even with these challenges, the benefits of AI in enhancing workflow efficiency are clear and impactful. By reducing the time from imaging to diagnosis, AI improves the operational efficiency of radiology departments and significantly enhances patient care by ensuring timely and accurate diagnostic services.
The contribution of AI to improving workflow efficiency in radiology is a testament to its potential to transform healthcare delivery. As technology continues to evolve, the role of AI in radiology is expected to expand further, driving efficiencies and improving outcomes across the healthcare spectrum. The following sections will further explore how AI facilitates personalised patient care and the ethical considerations surrounding its use in clinical settings.
4. Facilitating Personalised Patient Care
The integration of Artificial Intelligence (AI) into radiology goes beyond improving diagnostic accuracy and workflow efficiencies; it extends significantly into enhancing patient care through personalisation and precision medicine. The ability of AI to analyse vast datasets enables it to predict disease progression and response to treatments, paving the way for highly individualised patient management plans. This detailed exploration will illustrate the pivotal role of AI in revolutionising personalised healthcare within radiology.
Precision medicine is a medical model that proposes the customisation of healthcare, with medical decisions, practices, and products being tailored to the individual patient. In this context, AI tools in radiology can interpret complex medical data to identify unique patterns that pertain to individual patients’ prognoses or therapeutic responses. This capability is critical in diseases where imaging plays a key role in diagnosis and monitoring, such as oncology, neurology, and cardiovascular diseases.
In oncology, AI enhances personalised patient care by enabling more precise tumour detection, characterisation, and tracking. AI algorithms can analyse imaging scans to detect early signs of cancer, define the boundaries of a tumour, and identify the tumour’s subtype by recognising patterns that are often invisible to the human eye. Moreover, AI can predict the aggressiveness of the tumour and the likely prognosis by comparing the imaging data with historical data from similar cases. This helps craft a personalised treatment plan that may include targeted therapy and helps radiologists and oncologists anticipate potential complications or relapses.
The role of AI in personalised patient care is also evident in its ability to monitor treatment efficacy. For instance, in the treatment of cancer, AI systems can analyse sequential imaging studies to detect minute changes in tumour size and characteristics, providing real-time feedback on the effectiveness of the chosen treatment regimen. This immediate insight allows for timely adjustments to the treatment plan, such as escalating, de-escalating, or changing therapeutic approaches, thus optimising patient outcomes.
In the field of neurology, AI contributes to personalised care by facilitating the early detection and classification of neurological disorders through imaging. AI models trained on brain MRI data can identify early signs of diseases such as Alzheimer’s or Parkinson’s before significant symptoms manifest, enabling early intervention strategies. Additionally, AI can monitor the progression of these diseases by analysing changes over time in brain structure and function, aiding neurologists in adjusting treatments to the patient’s evolving condition.
Cardiovascular diseases similarly benefit from AI, which can assess heart function by analysing echocardiograms or MRIs to detect heart failure at an early stage. AI algorithms can measure and track cardiac outputs, ejection fractions, and other critical parameters more accurately and consistently than traditional methods. This capability ensures that treatment can be tailored based on the patient’s specific needs and response patterns, leading to better management of the disease.
The data-driven nature of AI also supports the development of predictive models in radiology that can forecast health outcomes based on a patient’s specific characteristics and their disease’s imaging features. These models can be used to personalise follow-up schedules and preventive measures, potentially reducing the overall healthcare costs and improving quality of life by preempting severe complications.
However, the application of AI in personalised patient care must navigate several challenges, including ethical issues related to patient data privacy and the need for robust, diverse datasets to train AI systems effectively. Furthermore, there is a need for a collaborative approach involving radiologists, clinicians, and AI experts to ensure that AI tools are used optimally and ethically.
Despite these challenges, the potential of AI in facilitating personalised patient care within radiology is immense. By providing tools that can predict, personalise, and promote health care tailored to individual needs, AI stands as a cornerstone of modern medical radiology, transforming it from a largely reactive discipline to a proactive and patient-centred one.
Therefore, the role of AI in radiology extends significantly into enhancing personalised patient care through precision medicine. By leveraging the power of AI to analyse and interpret large sets of medical imaging data, radiologists can offer more precise diagnoses, predict disease progression, and tailor treatment plans to each patient’s individual needs, thereby elevating the standard and effectiveness of medical care.
5. Ethical Considerations and Challenges
The integration of Artificial Intelligence (AI) into radiology, while heralding numerous advancements, also presents a range of ethical, legal, and professional challenges. As AI technologies become more pervasive in the healthcare sector, particularly in radiology, it is crucial to address these concerns to maintain trust and ensure the responsible use of AI.
Data Privacy and Security
One of the most pressing issues in the implementation of AI in radiology is the protection of patient data privacy. AI systems require access to vast amounts of medical images and associated data to train and refine their algorithms. This data often contains sensitive personal information that could be at risk of exposure, mainly if data breaches occur. Ensuring the security of this data and complying with regulations such as the General Data Protection Regulation (GDPR) in the EU or the Health Insurance Portability and Accountability Act (HIPAA) in the US is imperative. Healthcare providers must implement robust cybersecurity measures and data governance policies that protect patient data while enabling the benefits of AI.
Algorithmic Bias
Another significant challenge is algorithmic bias, where AI systems might display prejudices based on the data with which they were trained. If an AI system is trained primarily on datasets that lack diversity, its diagnostic suggestions may not be accurate for populations not well-represented in the training data. This can lead to misdiagnoses or suboptimal care for underrepresented groups, exacerbating existing healthcare disparities. To counteract this, training AI models on diverse datasets that accurately reflect the variety of patient populations that radiologists serve is essential.
Job Displacement and Role Reconfiguration
The fear of job displacement is common in discussions about AI. In radiology, while AI can enhance diagnostic accuracy and efficiency, there is concern that AI might replace human jobs. However, the reality is more nuanced. AI is generally seen as a tool that augments the capabilities of radiologists rather than replacing them. It can free radiologists from routine and repetitive tasks, allowing them to focus on more complex cases and patient interaction. Nonetheless, the role of radiologists will likely evolve, requiring ongoing education and adaptation to new technologies. Institutions must address these changes proactively through training programs and by redefining job descriptions to incorporate new AI-driven responsibilities.
Ethical Decision-Making
AI in radiology also raises questions about decision-making authority. When an AI system recommends a diagnosis or treatment plan, the human radiologist’s ultimate responsibility remains. This raises ethical questions about the extent to which clinicians should rely on AI recommendations. Developing clear guidelines on how to use AI advice responsibly and determining the liability in cases of AI errors are crucial steps in addressing these concerns.
Consent and Transparency
Finally, transparency and informed consent are fundamental in the use of AI in healthcare. Patients must be informed about how AI is used in their diagnosis and treatment, including the benefits and risks associated with AI technologies. Ensuring that patients understand and consent to the use of AI in their medical care respects their autonomy and rights.
While AI presents significant opportunities for enhancing the practice of radiology, addressing the associated ethical, legal, and professional challenges is essential. By fostering an environment of transparency, continuous learning, and ethical responsibility, the radiology community can harness the benefits of AI while mitigating its risks. This will improve patient care and sustain the trust and integrity essential to healthcare.
6. The Future of AI in Radiology
The future of Artificial Intelligence (AI) in radiology appears promising and is poised to redefine the boundaries of the field. As AI technologies continue to evolve, their integration with radiology is expected to deepen, bringing about more sophisticated diagnostic tools, enhancing patient care, and revolutionising training and professional development for radiologists.
AI in Radiology Training and Continuous Professional Development
As AI becomes more ingrained in radiology, it is also set to become a standard part of the radiology curriculum and ongoing professional development. AI can support the training of radiologists by providing simulation-based learning environments where trainees can interact with a wide range of virtual scenarios and receive instant feedback on their diagnostic decisions. This could significantly enhance learning outcomes by allowing trainees to gain experience with rare conditions that they might not encounter during their actual training.
Moreover, AI-driven analytics can help identify learning needs and knowledge gaps among practicing radiologists, facilitating tailored continuing professional development. AI can monitor performance trends and outcomes to recommend specific educational modules or practice areas that need attention, ensuring that radiologists remain at the cutting edge of their field.
Predictive Analytics and Personalised Medicine
Looking further into the future, AI is likely to expand its role from diagnostic support to become a pivotal tool in predictive analytics. AI systems could analyse historical and real-time radiology data to predict disease progression and patient outcomes, facilitating earlier interventions and more tailored treatment plans. This approach has the potential to improve healthcare outcomes and reduce costs by preventing disease progression and avoiding unnecessary treatments.
Ethical and Regulatory Evolution
As AI tools become more common and their impact more significant, there will also be a need for the evolution of ethical standards and regulatory frameworks. These frameworks will need to address the nuances of AI in practice, ensuring that these technologies benefit patients without compromising privacy, autonomy, or equity. Radiologists and other healthcare professionals will play a crucial role in shaping these standards, advocating for regulations that promote innovation while protecting patient welfare.
Therefore, the future of AI in radiology is marked by its potential to merge with other technologies, enhance educational paradigms, and advance into predictive analytics, significantly impacting how radiological services are provided and perceived. As we stand on the brink of this technological revolution, continuous evaluation and adaptation will be key in harnessing the full potential of AI to transform radiology.
7. Conclusion
The integration of Artificial Intelligence (AI) in radiology has undeniably transformed the field, offering profound advancements in diagnostic accuracy, workflow efficiency, and personalised patient care. As AI continues to evolve, its potential to further enhance these aspects is immense, indicating a future where radiology is more efficient, effective, and patient-centric.
The capability of AI to analyse and interpret vast quantities of imaging data with superior accuracy has significantly reduced diagnostic errors, providing clinicians with reliable tools to aid in decision-making. By automating routine tasks, AI has streamlined radiological workflows, allowing radiologists to focus on more complex diagnostic challenges and direct patient interactions. This shift not only boosts productivity but also enhances the quality of care delivered to patients. Furthermore, the role of AI in facilitating personalised patient care—through precise disease detection, treatment planning, and monitoring—exemplifies its capacity to tailor healthcare to individual patient needs, promoting better outcomes and patient satisfaction.
However, the road to fully integrating AI into radiology is laden with challenges that must be meticulously addressed. Ethical concerns such as data privacy, algorithmic bias, and the potential displacement of jobs require thoughtful consideration and action. It is crucial that these issues are navigated with a balanced approach that respects patient rights and promotes fairness and transparency.
Moreover, as AI reshapes the landscape of radiology, it is imperative to ensure that radiologists are adequately prepared to work alongside these advanced technologies. This involves initial training and continuous professional development that keeps pace with technological advancements.
While the impact of AI on radiology is groundbreaking, its successful integration depends on the careful management of ethical challenges and proactive educational strategies. By addressing these critical aspects, the radiology community can fully leverage AI to enhance service delivery, improve patient outcomes, and usher in a new era of medical imaging.
Disclaimer
The information provided in this article, “The Role of AI in Radiology: Transforming Healthcare,” is intended for general informational and educational purposes only. It does not constitute medical, clinical, or legal advice and should not be relied upon as a substitute for consultation with qualified professionals in these fields.
Open Medscience does not guarantee the accuracy, completeness, or currency of the content, and makes no warranties or representations of any kind concerning the results that may be obtained from using the information provided.
Any views or opinions expressed are those of the author(s) and do not necessarily reflect the official policy or position of Open Medscience. The inclusion of specific technologies, products, or services does not imply endorsement.
The development and application of Artificial Intelligence in healthcare, including radiology, remain subject to ongoing research, regulatory review, and ethical debate. Readers are advised to seek professional guidance before applying any insights or technologies discussed herein to clinical practice or policy development.
Open Medscience accepts no responsibility for any loss or damage resulting from reliance on the material contained in this publication.
You are here: home » diagnostic medical imaging blog »