Radiopharmaceuticals are a crucial component in the field of nuclear medicine, particularly for heart imaging. These substances, which include radioactive isotopes, are used to diagnose and monitor various cardiac conditions such as coronary artery disease, myocardial infarction, and heart failure. This article looks into the different types of radiopharmaceuticals used in heart imaging, their mechanisms of action, the imaging techniques employed, and the clinical applications of these methods. Furthermore, it discusses this area’s advancements and future prospects, along with the safety and regulatory considerations that ensure their effective use.
Introduction to Radiopharmaceuticals
Radiopharmaceuticals are radioactive compounds that emit radiation that is detectable by imaging devices when introduced into the body. These compounds consist of a radioactive isotope and a pharmaceutical agent, which directs the radioisotope to specific tissues or organs. The primary role of radiopharmaceuticals in heart imaging is to provide detailed images of the heart’s structure and function, aiding in diagnosing and treating various cardiac conditions.
Types of Radiopharmaceuticals in Heart Imaging
Several radiopharmaceuticals are utilised in heart imaging, each with unique properties and specific clinical applications. The most commonly used radiopharmaceuticals include:
- Technetium-99m (Tc-99m) Sestamibi: This agent is widely used for myocardial perfusion imaging (MPI). Tc-99m sestamibi accumulates in the heart muscle, allowing for the assessment of blood flow and identification of ischemic areas.
- Thallium-201 (Tl-201): Once the gold standard for MPI, Tl-201 is still used, particularly in stress tests to evaluate myocardial perfusion and viability. It mimics potassium and is taken up by viable myocardial cells.
- Technetium-99m (Tc-99m) Tetrofosmin: Similar to Tc-99m sestamibi, Tc-99m tetrofosmin is used in MPI for the evaluation of coronary artery disease. It provides high-quality images and is preferred for its faster clearance from non-cardiac tissues.
- Fluorine-18 (F-18) Fluorodeoxyglucose (FDG): FDG is primarily used in positron emission tomography (PET) imaging to assess myocardial viability and detect metabolic activity in heart tissues.
- Nitrogen-13 (N-13) Ammonia: Employed in PET imaging, N-13 ammonia is useful for myocardial perfusion studies, providing high-resolution images of blood flow.
Mechanisms of Action
The effectiveness of radiopharmaceuticals in heart imaging lies in their ability to target specific physiological processes within the heart. For instance, Tc-99m sestamibi and Tc-99m tetrofosmin are lipophilic cations that penetrate myocardial cells and accumulate in proportion to blood flow. This accumulation allows for the visualisation of perfusion patterns and the identification of ischemic regions.
Tl-201, on the other hand, is a potassium analogue that enters myocardial cells via active transport. Its distribution within the heart reflects myocardial tissue’s viability and perfusion status. FDG, a glucose analogue, is taken up by metabolically active cells, making it valuable for assessing myocardial viability, particularly in patients with heart failure or previous myocardial infarction.
Imaging Techniques
Various imaging techniques are employed to capture the distribution of radiopharmaceuticals within the heart, each offering distinct advantages:
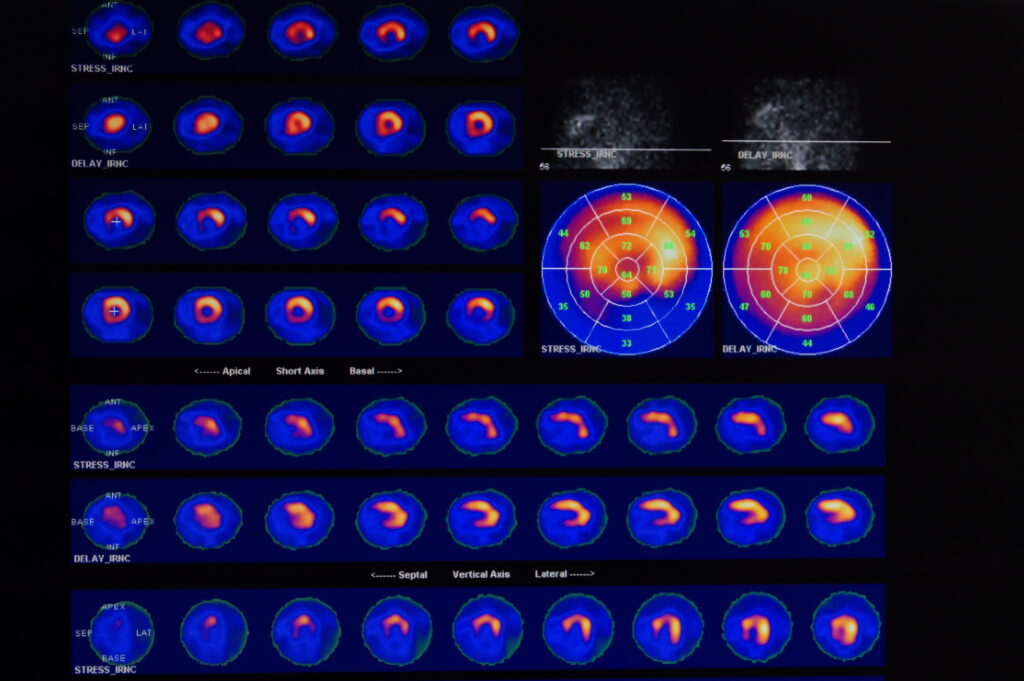
- Single Photon Emission Computed Tomography (SPECT): SPECT imaging involves the use of gamma cameras to detect the radiation emitted by radiopharmaceuticals. It provides three-dimensional images of myocardial perfusion and is widely used for diagnosing coronary artery disease.
- Positron Emission Tomography (PET): PET imaging uses radiopharmaceuticals like F-18 FDG and N-13 ammonia to produce high-resolution images of metabolic and perfusion processes in the heart. PET is particularly valuable for assessing myocardial viability and detecting hibernating myocardium.
- Planar Scintigraphy: This older technique involves capturing two-dimensional images of radiopharmaceutical distribution. While less commonly used today, it can still be useful in specific diagnostic scenarios.
Clinical Applications
Radiopharmaceuticals in heart imaging have several critical clinical applications:
- Diagnosis of Coronary Artery Disease (CAD): MPI with Tc-99m sestamibi or Tc-99m tetrofosmin is essential for identifying areas of reduced blood flow indicative of CAD. Stress tests combined with these agents help determine the extent and severity of ischemia.
- Assessment of Myocardial Viability: PET imaging with F-18 FDG is crucial for evaluating myocardial viability in patients with heart failure or previous myocardial infarction. This information helps guide decisions regarding revascularisation procedures.
- Evaluation of Myocardial Perfusion: Both SPECT and PET imaging are used to assess myocardial perfusion, providing detailed maps of blood flow distribution within the heart. This evaluation is vital for diagnosing and managing various cardiac conditions.
- Detection of Cardiac Sarcoidosis: FDG PET imaging is increasingly used to detect inflammation in patients with suspected cardiac sarcoidosis, a condition characterised by the formation of granulomas in heart tissue.
Advancements and Future Prospects
The field of radiopharmaceuticals in heart imaging continues to evolve, with several advancements on the horizon:
- Novel Radiopharmaceuticals: Research is ongoing to develop new radiopharmaceuticals with improved specificity and imaging characteristics. These agents aim to provide more accurate and detailed cardiac function and pathology information.
- Hybrid Imaging Techniques: Combining PET and magnetic resonance imaging (MRI) or PET and computed tomography (CT) allows for the simultaneous acquisition of anatomical and functional information, enhancing diagnostic accuracy.
- Quantitative Imaging: Advances in imaging technology and software are enabling more precise quantification of myocardial perfusion and metabolism. This quantitative approach aids in the early detection and management of cardiac conditions.
- Artificial Intelligence (AI): The integration of AI in image analysis is poised to revolutionise heart imaging. AI algorithms can assist in the interpretation of complex imaging data, improving diagnostic accuracy and reducing the workload on clinicians.
Safety and Regulatory Considerations
The use of radiopharmaceuticals in heart imaging is subject to stringent safety and regulatory guidelines to ensure patient safety and the effectiveness of the procedures. Key considerations include:
- Radiation Exposure: Minimising radiation exposure to patients is a primary concern. Advances in radiopharmaceuticals and imaging techniques aim to reduce the dose while maintaining image quality.
- Quality Control: Strict quality control measures are in place to ensure radiopharmaceuticals’ purity, sterility, and proper functioning. Regular testing and adherence to guidelines are essential.
- Training and Certification: Healthcare professionals involved in nuclear medicine and radiopharmaceuticals must undergo specialised training and certification to ensure proficiency in handling these substances and interpreting the imaging results.
- Regulatory Oversight: Regulatory bodies such as the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK and the Food and Drug Administration (FDA) in the US oversee the approval and use of radiopharmaceuticals. Compliance with their regulations ensures the safe and effective use of these agents.
Conclusion
Radiopharmaceuticals play a pivotal role in the field of heart imaging, providing valuable insights into the structure and function of the heart. Through techniques such as SPECT and PET, radiopharmaceuticals enable the diagnosis and management of various cardiac conditions, from coronary artery disease to myocardial viability assessment. The continuous advancements in this field, including the development of novel agents and the integration of AI, promise to enhance the accuracy and effectiveness of heart imaging further. As safety and regulatory measures continue to evolve, the use of radiopharmaceuticals in heart imaging will remain a cornerstone of modern cardiology, contributing to improved patient outcomes and the advancement of cardiac care.
Disclaimer
The information presented in this article is intended solely for educational and informational purposes. Open Medscience does not provide medical, diagnostic, or therapeutic advice and this content should not be interpreted as such. Radiopharmaceuticals used in heart imaging are highly specialised substances that must only be administered and interpreted by qualified healthcare professionals within properly regulated clinical settings.
While every effort has been made to ensure the accuracy and reliability of the information at the time of publication, Open Medscience makes no representations or warranties of any kind, express or implied, regarding the completeness, accuracy, suitability, or availability of the information contained herein. Any reliance placed on such information is strictly at the reader’s own risk.
This article does not substitute for professional medical advice, diagnosis, or treatment. Patients or readers concerned about cardiac conditions or imaging procedures should consult a licensed medical practitioner or nuclear medicine specialist.
Additionally, the use of radiopharmaceuticals is subject to regulatory requirements and clinical governance, which may vary depending on the country or region. Readers are encouraged to refer to local and international regulatory authorities, such as the MHRA (UK) or FDA (US), for the most up-to-date guidance and regulations regarding the clinical use of these agents.
Open Medscience and its contributors shall not be liable for any loss, injury, or damage arising from the use of the information provided in this article.
You are here: home » diagnostic medical imaging blog »