The ultrasound cart rolls in, and the screen wakes up before the first sterile pack opens. Nurses confirm depth, vessels, and landmarks while the patient settles into a steady position for comfort. That quick scan often shapes the plan more than another round of palpation alone in practice.
People with lasting back, neck, or joint pain want steps that match what hurts and when. Image-guided procedures can target a nerve or joint with less guessing during needle placement. Clinics like Closter pain management doctors often show patients how imaging supports safer choices and tighter targeting.
Imaging Turns Anatomy Into A Clear Target
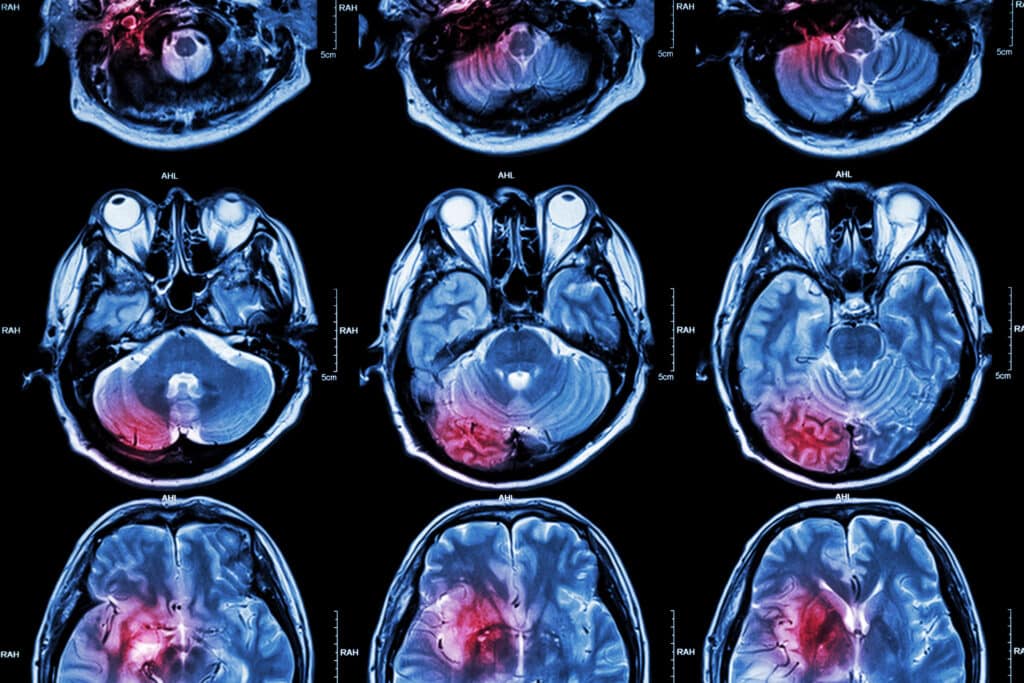
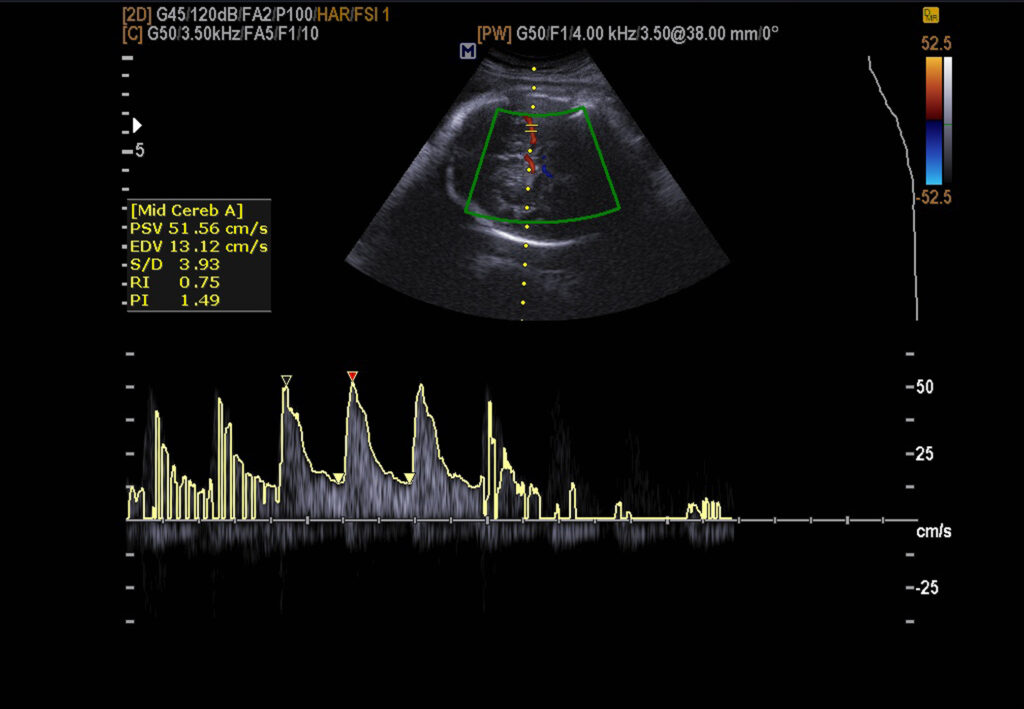
Many pain injections depend on placing medicine within a narrow space beside a nerve or joint. Ultrasound shows fascia planes, tendons, and vessels that hands cannot map well enough during procedures. Fluoroscopy confirms bony landmarks when bone offers the clearest reference for precise level and angle.
Modern ultrasound also includes Doppler views that highlight nearby blood flow in real time quickly. That matters because small vessels can sit close to nerves inside tight anatomical corridors quite often. When flow is visible, clinicians can choose a path that avoids it with less hesitation.
Imaging helps when anatomy varies, which is common in real clinics, not only in textbooks. Prior surgery, arthritis, and body mass can change angles, depth, and access points during placement. With live images, the clinician can adjust angle and depth without repeated needle passes across attempts.
Imaging can also confirm that medicine reached the intended plane, not a nearby pocket by mistake. Under fluoroscopy, contrast shows spread along a joint line or nerve root sleeve for confirmation. Under ultrasound, the clinician watches fluid separate tissue layers during injection and adjusts pressure gradually.
Smarter Fluoroscopy And Ultrasound Reduce Unneeded Exposure
Fluoroscopy remains common because it verifies level, needle position, and contrast spread within seconds. Radiation exposure is the tradeoff, so technique now centers on shorter runs and tighter beams. Many systems also record dose and time, which supports review and safer habits across teams.
The FDA provides patient focused guidance on medical imaging radiation and basic safety considerations for patients. It explains why dose varies and how collimation, distance, and time can reduce exposure substantially.
Ultrasound can replace fluoroscopy for many peripheral joints and several soft tissue targets in practice. That switch removes ionizing radiation for both patient and staff during those visits and repeat sessions. It also supports more comfortable positioning for patients who cannot lie flat for long periods.
Teams often combine tools, choosing the lowest exposure method that still confirms placement with confidence. In some spinal procedures, ultrasound helps with entry planning, while fluoroscopy confirms the final level. The point is enough imaging to guide care, not extra images for their own sake.
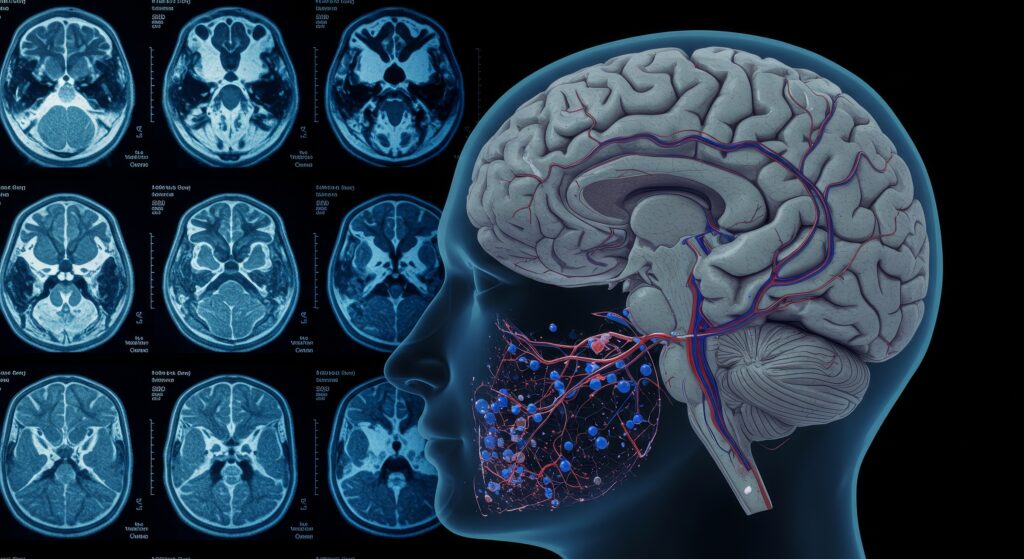
Fusion Imaging Links Diagnostic Scans With Procedure Day Decisions
MRI and CT often explain persistent symptoms, such as foraminal narrowing, facet arthritis, or a focal disc issue. In earlier workflows, those findings lived on separate screens or in printed reports during the visit. Newer fusion tools can align prior scans with live fluoroscopy views during procedures on the table.
This matters when landmarks are subtle, or when hardware changes the normal look of bone. A fused overlay can guide angle choice, expected depth, and a safer trajectory toward the target. Contrast checks still matter, yet planning becomes less uncertain at the start of the procedure.
In practical terms, fusion features help clinicians in three ways during complex cases with challenging anatomy.
- They match a prior MRI level to the correct fluoroscopy level during careful setup checks.
- They suggest an expected needle depth, which reduces over advancement when tissues resist unexpectedly today.
- They shorten the first minutes of the case, when staff confirm laterality and target alignment.
Fusion imaging also helps communication, because the team can point to one shared view together. Patients can see why a target level was chosen, and why another level was not chosen. That clarity can reduce surprise when results are partial and more testing is needed later.
Imaging Helps Match The Procedure To The Pain Source
A procedure works best when it matches the symptom map, exam findings, and activity limits. Imaging can rule out red flags like fracture, infection, or a mass effect on nerves. It can also show changes that guide which joint or level to test first during evaluation.
Many clinicians use diagnostic blocks to test a suspected pain generator before longer-lasting treatments. If pain drops in the expected window, the team has stronger evidence for that target. If pain does not change, they can adjust without repeating the same approach at the next visit.
Imaging also supports safer decisions around medication choice and injection volume during these procedures today. For example, real time spread can guide how much solution is needed for adequate coverage on screen. Clear placement can reduce the urge to use higher doses to compensate for uncertainty during treatment.
Documentation improves when imaging, technique notes, and outcomes are recorded together for later clinical review. A note with level, approach, and contrast pattern helps interpret later pain diaries more accurately. That record supports safer follow up decisions across multiple visits and across different clinicians over time.
Follow Up Imaging And Monitoring Close The Feedback Loop
After a procedure, the useful question is whether function changes across sleep, work, and movement. Many practices use simple outcome scales plus short activity notes to track response over time. Imaging is used more selectively, usually when new symptoms change the plan or raise concern.
When imaging is needed, the tool should match the question and the body region being assessed. Ultrasound can check for a superficial hematoma or fluid collection near an injection site quickly. MRI can help assess new weakness, progressive numbness, or a new pain pattern after treatment.
MedlinePlus notes that epidural injections for back pain are often guided with real time x-ray imaging. It also describes the sequence, including numbing medicine and steroid placement near irritated nerves under guidance.
Before scheduling, it helps to ask direct questions, then write down the answers for later. Which imaging method will be used, and what does it show in your case today? How will the team measure improvement during the next two weeks after treatment in your routine?
The practical takeaway is that imaging advances support better targeting, safer technique, and clearer follow-up. When the plan is tied to images and outcomes, it feels less vague and more grounded. That is often what patients want when pain keeps returning despite good effort and careful habits.
Disclaimer
The information provided in 5 Ways Imaging Advances Interventional Pain Care is for general educational and informational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. Content published by Open MedScience reflects current knowledge at the time of writing; however, medical practices, technologies, and clinical guidance may change over time.
Readers should not rely on this material to make decisions about their health or treatment plans. Always seek advice from a qualified healthcare professional regarding any medical condition, symptoms, or procedures. Imaging techniques, interventional pain treatments, and clinical outcomes vary between individuals, and results cannot be guaranteed.
Open MedScience does not accept responsibility for any loss, injury, or damage arising from the use or interpretation of information contained in this article. References to external clinics, organisations, or healthcare providers are for informational purposes only and do not constitute endorsement.
home » blog » radiology »