Selective Internal Radiotherapy (SIRT) targets liver cancer by delivering precise radiation doses via microspheres, offering effective, minimally invasive treatment.
Introduction to Radiotherapy
Radiotherapy, or radiation therapy, is a medical treatment that utilises ionising radiation to control or kill malignant cells. It is a cornerstone in treating various cancers, offering a curative or palliative approach. The primary objective of radiotherapy is to damage the DNA of cancer cells, thereby inhibiting their ability to reproduce and grow. Traditional radiotherapy involves external beam radiation therapy (EBRT), where high-energy rays are directed at the tumour from outside the body. However, advancements in medical science have introduced more targeted forms of radiotherapy, such as Selective Internal Radiotherapy (SIRT).
What is SIRT?
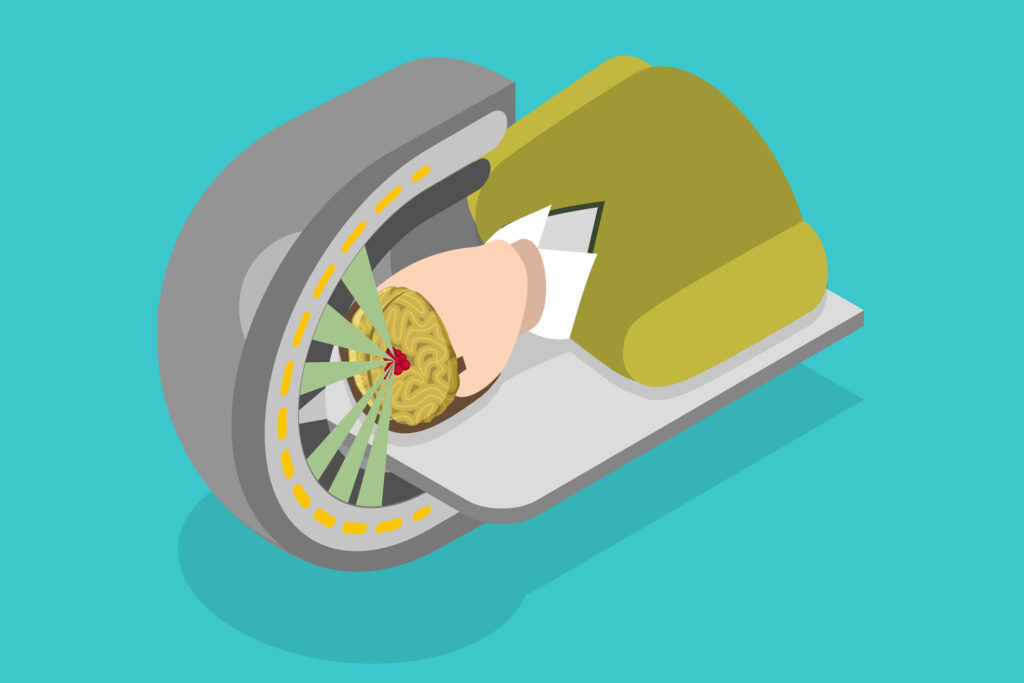
Selective Internal Radiotherapy (SIRT), also known as radioembolisation, is a minimally invasive procedure used primarily to treat liver cancers, including hepatocellular carcinoma (HCC) and metastatic liver disease. SIRT involves the delivery of radioactive microspheres directly into the liver tumours via the hepatic artery. These microspheres, typically containing the radioisotope Yttrium-90 (Y-90), emit beta radiation, which destroys the cancer cells from within the liver.
Mechanism of Action
The fundamental principle of SIRT is to deliver a high dose of radiation directly to the tumour while sparing the surrounding healthy liver tissue. This targeted approach is achieved through the following steps:
- Pre-procedure Planning: Prior to SIRT, a thorough assessment of the patient’s liver anatomy and tumour characteristics is conducted. This involves imaging techniques such as CT scans, MRI, and angiography to map out the liver’s vascular structure for radiation therapy planning.
- Angiography and Catheter Placement: Under local anaesthesia, a catheter is inserted into the femoral artery and guided into the hepatic artery, which supplies blood to the liver. This process is monitored using fluoroscopy, a type of real-time X-ray imaging.
- Injection of Microspheres: The radioactive microspheres are injected into the hepatic artery once the catheter is in place. The microspheres travel through the blood vessels and become lodged in the capillaries surrounding the tumour. The Y-90 emits high-energy beta particles, delivering a concentrated dose of radiation to the cancer cells.
- Post-procedure Monitoring: After the procedure, patients undergo imaging studies to confirm the microspheres’ distribution and assess the tumour’s initial response to the treatment. Follow-up appointments are scheduled to monitor the patient’s progress and manage any side effects.
Advantages of SIRT
SIRT offers several advantages over traditional forms of radiotherapy and systemic chemotherapy, particularly for liver cancer patients:
- Targeted Therapy: The precision of SIRT allows for the delivery of a high radiation dose directly to the tumour, minimising damage to surrounding healthy liver tissue. This targeted approach can be especially beneficial in patients with multiple liver tumours or tumours that are difficult to access with surgery.
- Minimally Invasive: SIRT is performed through a catheter-based technique, making it less invasive than surgical options. This reduces the risk of complications and shortens recovery time.
- Combination with Other Treatments: SIRT can be used in conjunction with other treatments such as chemotherapy, surgery, or systemic radiotherapy, providing a multifaceted approach to cancer management.
- Palliative Care: For patients with advanced liver cancer who are not candidates for surgery, SIRT can provide palliative benefits by reducing tumour size, alleviating symptoms, and potentially extending survival.
Clinical Applications
SIRT has shown efficacy in treating various liver cancers, both primary and secondary:
- Hepatocellular Carcinoma (HCC): HCC is the most common type of primary liver cancer. SIRT is particularly useful for patients with intermediate or advanced HCC who are not suitable candidates for surgical resection or liver transplantation. Studies have demonstrated that SIRT can improve these patients’ overall survival and quality of life.
- Metastatic Liver Disease: The liver is a common site for metastases from cancers such as colorectal, breast, and neuroendocrine tumours. SIRT can be an effective treatment option for patients with liver-dominant metastatic disease, providing tumour control and symptom relief.
- Cholangiocarcinoma: This rare cancer originates in the bile ducts. SIRT has been used as part of a multidisciplinary approach to manage unresectable cholangiocarcinoma, often in combination with chemotherapy.
Side Effects and Complications
While SIRT is generally well-tolerated, it is not without potential side effects and complications. Common side effects include:
- Post-embolisation Syndrome: Patients may experience flu-like symptoms, such as fever, fatigue, nausea, and abdominal pain, for several days following the procedure. These symptoms are typically mild and self-limiting.
- Liver Toxicity: In some cases, the radiation delivered by the microspheres can cause liver inflammation or damage. This risk is higher in patients with pre-existing liver conditions, such as cirrhosis.
- Radiation Pneumonitis: Although rare, the inadvertent delivery of microspheres to the lungs can result in radiation pneumonitis, a condition characterised by inflammation of the lung tissue.
- Gastrointestinal Ulcers: If the microspheres inadvertently lodge in the stomach or intestines, they can cause radiation-induced ulcers, which can lead to pain and bleeding.
Patient Selection and Contraindications
Patient selection is critical for the success of SIRT. Candidates for SIRT are typically evaluated based on several factors, including tumour size and location, liver function, and overall health status. Contraindications for SIRT include:
- Severe Liver Dysfunction: Patients with significantly impaired liver function or liver failure may not tolerate the additional stress of radiation therapy.
- Portal Vein Thrombosis: The presence of a blood clot in the portal vein, which supplies blood to the liver, can complicate the delivery of microspheres and increase the risk of complications.
- Extrahepatic Disease: Patients with extensive disease outside the liver may not benefit from a liver-directed therapy such as SIRT.
- Previous Radiotherapy: Prior radiotherapy to the liver can increase the risk of liver toxicity and other complications.
Advances and Future Directions
SIRT is an evolving field, with ongoing research to improve its efficacy and expand its applications. Some areas of active investigation include:
- Dosimetry and Imaging: Advances in imaging techniques and dosimetry (the calculation of radiation doses) enhance SIRT’s precision. Techniques such as PET/CT and MRI are being used to improve the assessment of tumour response and optimise treatment planning.
- Combination Therapies: Researchers are exploring the combination of SIRT with other treatments, such as immune checkpoint inhibitors and targeted therapies, to enhance the anti-tumour effects.
- New Radioisotopes: While Y-90 is the most commonly used radioisotope in SIRT, other isotopes, such as Holmium-166, are being investigated for their potential advantages, including different radiation properties and imaging capabilities.
- Expansion to Other Cancers: Although primarily used for liver cancers, SIRT is being studied for its potential use in treating other cancers, such as pancreatic and renal cell carcinoma, where traditional treatment options are limited.
Conclusion
Selective Internal Radiotherapy (SIRT) represents a significant advancement in the field of radiotherapy, offering a targeted and minimally invasive treatment option for patients with liver cancer. By delivering high doses of radiation directly to the tumour while sparing healthy tissue, SIRT provides an effective means of tumour control, symptom relief, and potentially improved survival. As research continues to advance our understanding of this technique, SIRT is poised to play an increasingly important role in the multidisciplinary management of cancer. While not without its challenges, the potential benefits of SIRT make it a valuable addition to the arsenal of cancer therapies, offering hope to patients with limited treatment options.
Disclaimer
The information provided in this article is intended for educational and informational purposes only and does not constitute medical advice, diagnosis, or treatment. Open Medscience makes no representations or warranties regarding the accuracy, completeness, or currency of the content. Selective Internal Radiotherapy (SIRT) is a complex medical procedure that may not be suitable for all patients. Any medical decisions or treatment plans should be made in consultation with qualified healthcare professionals based on individual medical history and condition. Readers should not disregard professional medical advice or delay seeking it based on the information contained in this article. Open Medscience disclaims any liability for any direct, indirect, or consequential loss or damage incurred by readers relying on the information herein.