Radiotherapy machines are advanced tools that deliver high-energy radiation to treat cancer. From linear accelerators to cyberKnife and tomotherapy, these machines constantly evolve with new technological advancements.
Understanding Radiotherapy Machines as a Cancer Treatment
Radiotherapy machines use high-energy X-rays or other types of radiation to destroy cancer cells by damaging their DNA.
External beam radiation therapy is the most common type of radiotherapy, and it involves directing a beam of high-energy radiation from a machine outside the body towards the tumour. The radiation is targeted to ensure that it affects only the cancer cells and limits damage to the surrounding healthy tissue as possible. This type of radiotherapy is usually delivered over several weeks, with each treatment session lasting only a few minutes.
Internal radiation therapy, or brachytherapy, involves placing a small radioactive source inside the body near the tumour. This allows a higher radiation dose to be delivered directly to the cancer cells while limiting damage to surrounding healthy tissue.
Radiotherapy may be used alone or with other cancer treatments, such as chemotherapy or surgery. The treatment plan doctors will depend on the type and stage of cancer, the patient’s overall health and other medical conditions.
Linear Accelerators: A Vital Tool in Radiation Oncology
Linear accelerators (LINACs) are one of the most commonly used radiotherapy machines to treat cancer. They use electricity to accelerate electrons to very high speeds and collide them into a heavy metal target, creating high-energy X-rays. These X-rays are then shaped into a beam directed at the cancerous cells.
LINACs offer several advantages over other types of radiotherapy machines. They can deliver radiation with high precision, allowing doctors to target cancerous cells while reducing damage to nearby healthy tissue. Linear accelerators can deliver different types of radiation, including photons, electrons, and protons, depending on the type of cancer and the treatment plan. The radiation is delivered quickly and is important for patients receiving radiation as part of their primary cancer treatment. In addition, LINACs are non-invasive and, therefore, can reduce the risk of infection and other complications. In general, LINACs are an essential tool in the fight against cancer, and they continue to be a key component of many cancer treatment plans.
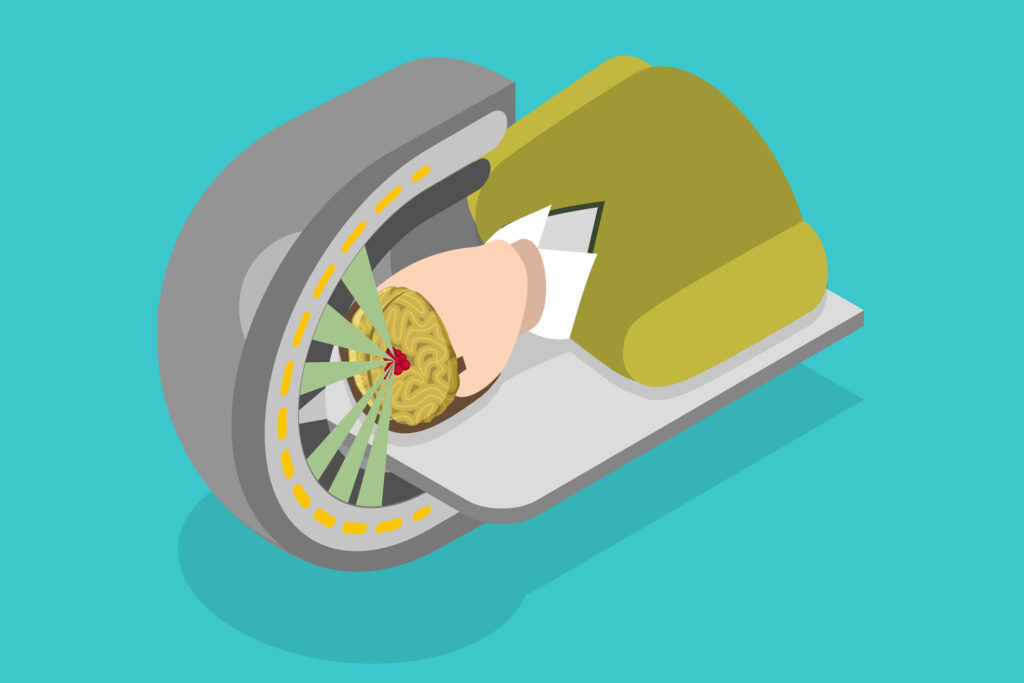
Gamma Knife Radiosurgery: An Advanced Technique for Treating Brain Tumours
Gamma Knife is a type of radiosurgery machine that uses gamma rays to treat tumours in the brain. It uses multiple sources of gamma radiation to deliver a highly focused dose of radiation to the tumour while minimising radiation exposure to the surrounding healthy tissue.
The Gamma Knife machine has a frame attached to the patient’s head to keep it still during the procedure. The head frame is attached to a machine that delivers a precise radiation dose to the tumour site. The machine uses 192 individual beams of gamma radiation to target the tumour from different angles while limiting exposure to the surrounding healthy tissue. The entire procedure is typically completed in a single session, and the patient can usually go home the same day.
Gamma Knife is particularly effective for treating tumours in the brain that are difficult to remove surgically or for patients who are not good candidates for surgery due to other health issues. It can also be used to treat tumours that have recurred after previous treatment or as a primary treatment option for small tumours.
Proton Therapy: A Powerful Tool for Fighting Cancer
Proton therapy machines use protons to deliver radiation therapy. Protons are positively charged particles that can be directed to the tumour site with greater precision than X-rays. This results in less damage to healthy tissue surrounding the tumour.
Proton therapy machines use a particle accelerator to generate high-energy protons, which are then directed at the tumour using a system of magnets. The protons penetrate the tumour and deposit their energy directly into the tumour cells, causing damage to the DNA and ultimately killing the cancer cells.
One of the key advantages of proton therapy is that it delivers radiation with a high degree of precision, which allows doctors to target the tumour while reducing exposure to healthy tissue. This is because protons have a characteristic depth-dose curve, meaning they deposit most of their energy at a specific depth in the tissue. By adjusting the energy of the protons, doctors can control the depth at which the energy is deposited, allowing them to target the tumour precisely.
Proton therapy is beneficial for treating tumours that are located near sensitive structures, such as the spinal cord, brainstem, or eyes. It can also be used to treat tumours in children, as it has been shown to cause less damage to surrounding tissues than traditional radiation therapy.
There are several types of proton therapy machines, including cyclotron-based and synchrotron-based machines. These machines differ in how they generate and accelerate the protons, but they all work using a system of magnets to direct the protons to the tumour.
Proton therapy is a safe and effective treatment option for many patients with cancer, and it offers several advantages over traditional radiation therapy.
Cyberknife Radiosurgery: A Non-Invasive Treatment for Cancer and Tumours
CyberKnife is a type of radiosurgery machine that uses advanced robotics technology to treat tumours in the brain and other parts of the body. It uses a combination of advanced imaging technology and robotics to deliver a highly precise dose of radiation to the tumour while minimising radiation exposure to the surrounding healthy tissue. The machine uses a small linear accelerator that can move in multiple directions, allowing it to target the tumour from various angles.
One of the key advantages of CyberKnife is that it can adjust for small movements of the patient during treatment. This is particularly important when treating tumours in the brain, as even small movements of the patient’s head can cause the tumour to move relative to the treatment beam. CyberKnife uses advanced tracking technology to monitor the position of the tumour during treatment continuously, and it adjusts the position of the treatment beam in real-time to ensure that the tumour is always in the target zone.
Tomotherapy: A Unique Approach to Radiation Therapy for Cancer Treatment
Tomotherapy is a radiation therapy machine that combines a linear accelerator with a computed tomography (CT) scanner. This allows for highly targeted radiation delivery while reducing exposure to healthy tissue.
Tomotherapy is a type of radiation therapy used in cancer treatment. It is a specialised form of intensity-modulated radiation therapy (IMRT) that combines CT scanning and radiation therapy delivery to target cancer cells while precisely limiting damage to healthy tissue.
During tomotherapy, the patient lies on a table that moves slowly through a CT scanner while a radiation beam is directed at the tumour from multiple angles. The CT images are used to create a 3-D of the tumour and surrounding tissue, allowing the radiation oncologist to tailor the radiation dose to the specific shape and size of the tumour.
One of the advantages of tomotherapy is its ability to deliver high doses of radiation to the tumour while sparing nearby healthy tissue. This is particularly important in treating tumours in areas such as the brain, spine, and lungs, where minimising damage to healthy tissue is critical.
While tomotherapy is generally safe and effective, it can cause side effects such as fatigue, skin irritation, and nausea. Patients may also experience long-term side effects such as scarring and tissue damage. Therefore, patients must discuss the potential risks and benefits of tomotherapy with their doctor before undergoing treatment.
Brachytherapy: Delivering Radiation Therapy from the Inside Out
Brachytherapy is a type of radiation therapy used in cancer treatment that involves placing radioactive sources directly into or near the tumour. Several types of brachytherapy machines are used in this treatment and include:
- High-Dose Rate (HDR) Brachytherapy Machine delivers a high dose of radiation to the tumour for a short period of time. The machine contains a tiny radioactive source inserted into a catheter or applicator placed near the tumour. The radioactive source is moved to different positions to deliver the radiation dose in a precise manner. HDR brachytherapy is commonly used to treat cervix, prostate, and breast cancers.
- Low-Dose Rate (LDR) Brachytherapy Machine delivers a continuous low dose of radiation to the tumour over a more extended period of time. The machine contains tiny radioactive seeds implanted directly into the tumour or surrounding tissue. Depending on the specific treatment plan, the seeds release radiation over several weeks or months. LDR brachytherapy is commonly used to treat prostate cancer.
- Electronic Brachytherapy Machine delivers low-energy X-rays to the tumour through a small applicator. The portable machine can be used in a doctor’s office or outpatient setting. Electronic brachytherapy is commonly used to treat skin cancers.
- Pulsed-Dose Rate (PDR) Brachytherapy Machine delivers radiation to the tumour in pulses, with short periods of high radiation followed by extended periods of no radiation. The machine contains a radioactive source that is placed near the tumour and is moved to different positions to deliver the radiation dose in a precise manner. PDR brachytherapy is commonly used to treat gynaecological cancers.
Brachytherapy is a highly effective cancer treatment that can provide targeted radiation therapy to the tumour while reducing damage to surrounding healthy tissue. The specific type of brachytherapy machine used will depend on the type and location of the tumour being treated.
The Future of Radiotherapy Machines: Trends, Challenges, and Opportunities
The future of radiotherapy machines in cancer treatment is promising, as new technologies and advancements in existing technologies are being developed to improve the effectiveness and efficiency of cancer treatment.
One of the most significant advancements in radiotherapy technology is the development of intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT). Both use advanced computer algorithms and software to deliver highly targeted radiation to cancer cells while minimising damage to surrounding healthy tissues. This allows higher doses of radiation to be delivered to the tumour, resulting in better patient outcomes.
Another promising technology is proton therapy, which uses protons instead of photons to deliver radiation to cancer cells. Protons have a unique energy deposition profile that allows for more precise targeting of cancer cells while sparing surrounding healthy tissue. Proton therapy is beneficial for treating tumours in sensitive areas such as the brain, spine, and prostate.
There are also emerging technologies such as carbon ion therapy, which is even more precise and powerful than proton therapy but is currently only available in a few specialised centres worldwide.
In addition to these technological advancements, there is a growing trend towards personalised medicine, where treatment plans are tailored to individual patients based on their genetic and molecular characteristics. This approach is expected to become more common and will likely lead to better patient outcomes.
Disclaimer
The content provided in this article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy and relevance of the information presented, Open Medscience makes no warranties or representations regarding its completeness, reliability, or applicability to individual circumstances.
Radiotherapy and other cancer treatments should always be discussed with a qualified healthcare professional who can assess each patient’s unique medical history and condition. Technologies and methods referenced in this article, including linear accelerators, Gamma Knife, CyberKnife, proton therapy, tomotherapy, and brachytherapy, may not be suitable or available for all patients.
Readers should not rely solely on the information presented here when making decisions about cancer treatment. Any medical concerns should be addressed promptly with a licensed healthcare provider.
Open Medscience accepts no liability for any loss or damage resulting from the use of or reliance on the information in this article.
You are here: home » diagnostic medical imaging blog »