Summary: Auger electron-emitting radionuclides have generated growing interest in nuclear medicine for their unique ability to deliver highly localised damage to malignant cells. This article focuses on several radionuclides that release Auger electrons, including In-111, I-123, I-125, Pt-193m, Pt-195m, Sn-117m and Pd-103. Their shared characteristics, potential advantages, and clinical applications will be discussed alongside current challenges and prospects for using Auger electron therapy in diverse cancer settings.
Keywords: Auger electron-emitting radionuclides; In-111 targeted therapy; I-123 radiopharmaceuticals; I-125 brachytherapy applications; Pt-193m and Pt-195m radiotherapeutics; Sn-117m bone metastases treatment.
Background on Auger Electron-Emitting Radionuclides
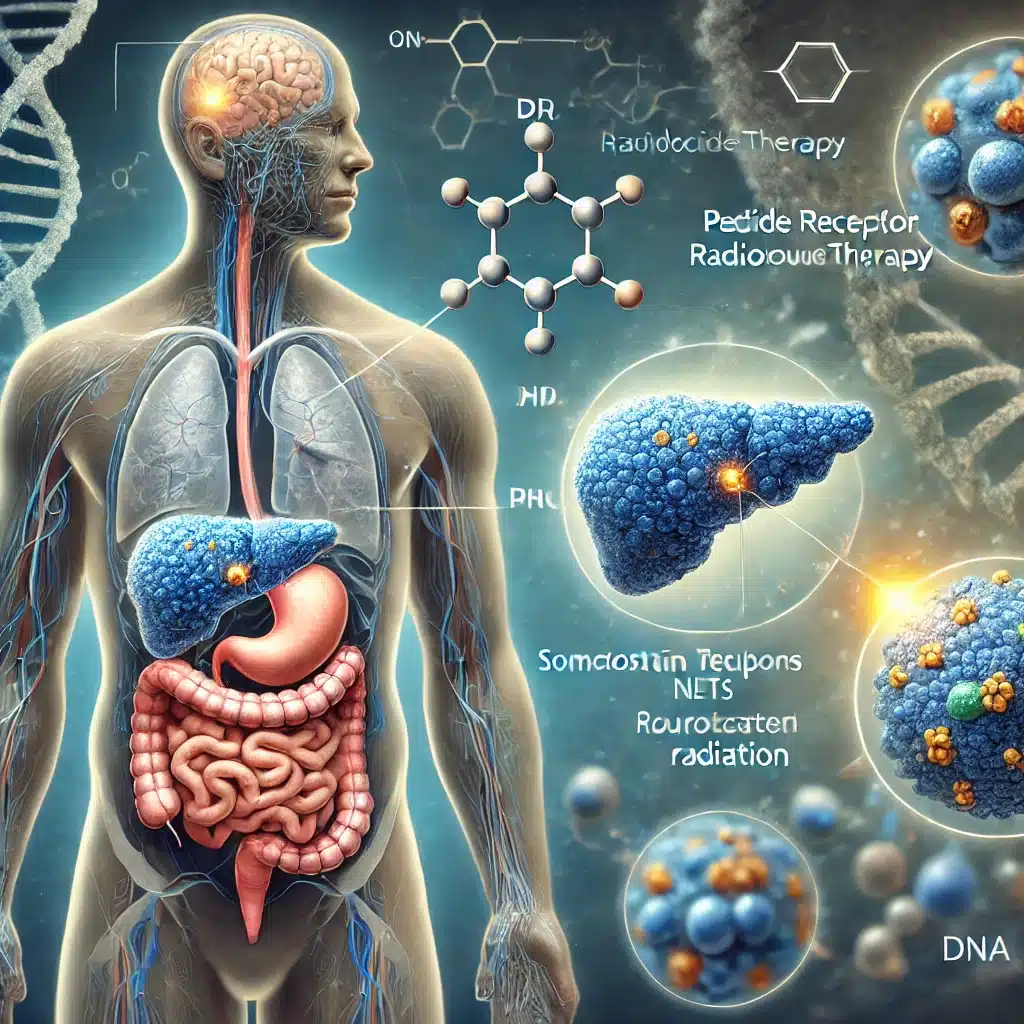
Therapeutic nuclear medicine aims to harness the properties of radionuclides to treat cancer and other conditions that require precise and targeted approaches. Auger electrons have gained significant attention among the different types of radioactive emissions used in therapy. These low-energy electrons produce high linear energy transfer (LET) near their emission site, potentially causing substantial damage to cancer cells at the DNA level when the radionuclide is delivered inside or very close to the cell nucleus. Such targeted destruction can reduce off-target toxicity, which is crucial for patients undergoing cancer therapy.
The Auger effect involves an atom undergoing ionisation, typically in an inner shell. When an electron from a higher shell fills the vacancy, the energy released can eject another electron from the same atom. These emitted electrons are known as Auger electrons and usually possess energies in the low keV range. In nuclear medicine, if the radionuclide undergoes electron capture or internal conversion, Auger electrons can be released in multiple cascades, causing extremely localised radiation damage. This damage is most potent if the emitting radionuclide is located within or near the cell nucleus.
One of the main attractions of Auger electrons lies in their short-range—often only a few nanometres to micrometres in tissue. This confers the advantage of sparing neighbouring cells while precisely destroying the targeted cancer cells. The outcome can be improved tumour control, less damage to healthy tissue, and more tolerable side effects for patients. However, successful therapy requires that these radionuclides be transported into or near the nucleus of malignant cells. Researchers have been working on conjugating these radionuclides into molecules that can penetrate cancer cells and localise within or near the nucleus.
In-111 for Therapeutic Use
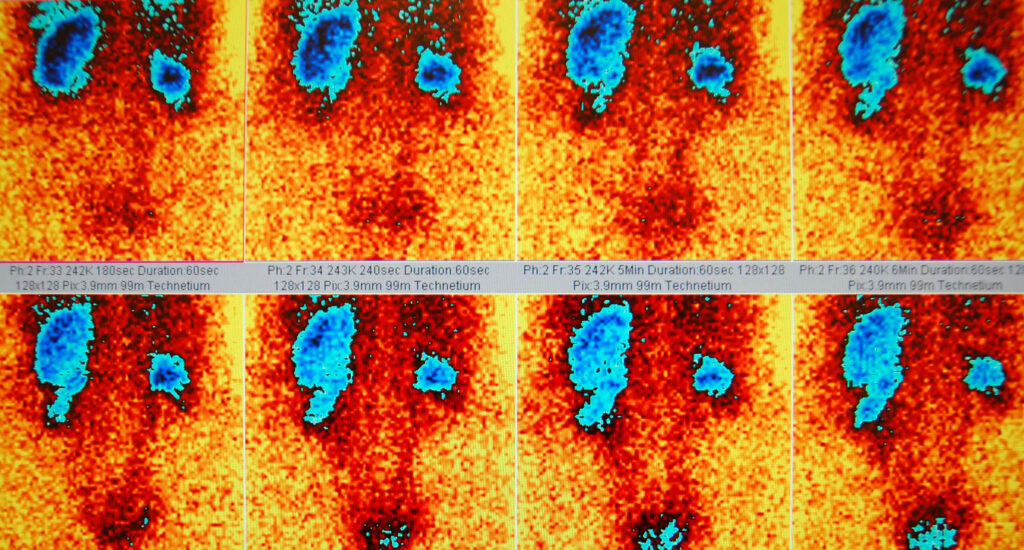
In-111 has been widely used in diagnostic imaging, particularly for scintigraphy. However, it also releases Auger electrons, making it interesting for targeted therapy. The half-life of In-111 is approximately 2.8 days, enabling practical radiolabelling and transport to treatment facilities. Researchers have conjugated In-111 to monoclonal antibodies and peptides to guide this radionuclide to cancer cells that overexpress specific antigens.
In certain studies, In-111 has shown the capacity to eradicate tumour cells when delivered in adequate amounts. Clinical research is investigating the possibility of using it in combination with DNA-binding agents, thereby directing its Auger electrons closer to the critical nuclear region. If these strategies achieve consistent nuclear localisation, In-111 could become an important tool in treating microscopic malignant foci.
The radiolabelling chemistry for In-111 relies on chelators such as diethylenetriaminepentaacetic acid (DTPA) or newer bifunctional chelators. These chelators help maintain stability, ensuring that the radionuclide remains attached to its targeting vector before and after administration to a patient. Continued optimisation of conjugates is expected to enhance In-111’s efficacy in delivering Auger electron therapy.
I-123: Diagnostic Workhorse with Therapeutic Potential
I-123 is primarily known for its use in diagnostic imaging of the thyroid gland and for imaging certain tumours that express specific receptors. However, I-123 also emits Auger electrons. Its half-life of around 13 hours is relatively short, which can be a limiting factor for therapeutic use but may be beneficial in situations that call for rapid clearance and lower overall radiation exposure to healthy tissues.
Various research groups have examined ways to incorporate I-123 into targeted molecules, including peptides and antibodies, to harness Auger electrons. When appropriately localised within tumour cells, I-123 can deliver lethal damage. An example is using I-123-labelled monoclonal antibodies directed at tumour-specific antigens on neuroendocrine or breast cancer cells. Moreover, the short half-life could prove helpful for repeated administrations if needed. Advances in microfluidics and small-scale radiopharmacy are also expected to improve the availability of I-123 for therapeutic protocols, provided that reliable supply chains are established.
One of the important considerations is the capacity of I-123 to produce adequate levels of Auger electrons during its decay scheme. Cell death can occur with a lower probability of harming healthy tissues if these electrons can be deposited close to the DNA. Clinical trials exploring I-123-based targeted therapies continue monitoring toxicity, tumour shrinkage, and overall survival outcomes while recording any adverse effects.
I-125: Long Half-Life and DNA-Targeting Strategies
I-125 has a significantly longer half-life of about 59.4 days. This property has made it useful for brachytherapy, particularly in managing prostate cancer, where small “seeds” are implanted. Brachytherapy with I-125 usually depends on gamma emissions for therapy. Still, its emission of Auger electrons can also be harnessed when the radionuclide is brought into close proximity to the tumour’s DNA.
Because of its extended half-life, I-125 can be used in studies that require lengthier observation periods or in situations where production and transport logistics are more complicated. Researchers have explored the conjugation of I-125 to nucleic acid-binding compounds, ensuring that the Auger electrons are released precisely where they can have maximum effect. The challenge lies in refining delivery vectors so that healthy tissues remain unscathed.
Clinical evidence suggests that I-125 seeds may deliver localised therapy for weeks or even months when placed in or near malignant tissues. While many procedures rely on its gamma emissions for local irradiation, there is increasing interest in capitalising on Auger electron emissions. Ongoing research explores how to exploit these emissions more fully, perhaps by designing custom vehicles that incorporate I-125 directly into the nucleus of cancer cells.
Pt-193m and Pt-195m: Platinum-Based Auger Therapy
Platinum compounds, such as cisplatin, are already used in chemotherapy. Radioisotopes of platinum offer potential synergy, allowing dual mechanisms of tumour cell destruction. Pt-193m and Pt-195m emit Auger electrons upon decay, which may intensify the local cytotoxic effects when these isotopes are delivered alongside DNA-binding platinum complexes.
Although the chemistry of radioplatinum is more challenging to handle than radioiodine, there is a growing interest in these isotopes for nuclear medicine. Pt-193m has a half-life of around 4.33 days, while Pt-195m has a half-life of roughly 4.02 days. These timelines provide a window for accurate tumour targeting. Research has investigated ways to stabilise Pt-193m and Pt-195m within chelators or incorporate them into analogues of platinum drugs such as cisplatin or carboplatin.
When Pt-193m and Pt-195m are transported directly into the nucleus, the emitted Auger electrons may interact with DNA to produce lethal lesions. This localised approach minimises the damage to non-target cells, potentially enhancing the tolerability of platinum-based radiotherapeutics. Although early results appear promising, clinical translation remains challenging, requiring advanced purification, chelation methods, and reliable supply. Nevertheless, continuing research on Pt-193m and Pt-195m is helping pave the way for platinum-based Auger therapy.
Sn-117m: Tin Isotope with Therapeutic Utility
Sn-117m (tin-117m) has shown potential for pain palliation in bone metastases, particularly when used as Sn-117m-DTPA or other complexes. This radionuclide emits both conversion electrons and gamma photons. Its electron emissions include Auger electrons that can be exploited for localised therapy. The half-life of around 13.6 days provides sufficient patient scheduling and transportation time.
There is active research into combining Sn-117m with tumour-targeting ligands, hoping to direct its Auger electrons to specific cancer cells. For instance, radiolabelling bisphosphonates with Sn-117m allows targeted deposition in areas of high bone turnover, such as those in metastatic prostate or breast cancer. Because of its favourable emission characteristics, Sn-117m could be incorporated into various radiopharmaceuticals designed for both palliation and direct anticancer effects.
The production process for Sn-117m typically involves reactors or cyclotrons, and consistent supply remains a concern. Researchers are also exploring improved chelation chemistry to ensure that Sn-117m remains tightly bound to the targeting agent during distribution in the body. Ongoing clinical trials and observational studies are expected to shed more light on the true capabilities of Sn-117m in delivering Auger electron therapy.
Pd-103: Palladium and the Promise of Localised Treatment
Pd-103 has long been known for its use in brachytherapy seeds, especially in treating prostate cancer. These seeds emit low-energy photons as they decay, allowing local radiation without extensive damage to surrounding tissues. Less frequently highlighted is the fact that Pd-103 can also emit Auger electrons. While the photon emissions are often sufficient for local tumour control, the potential contribution of Auger electrons in cellular-level destruction is an area of increasing interest.
The half-life of Pd-103 is roughly 17 days, offering a window that supports the slow release of radiation in brachytherapy settings. When the seeds are implanted into cancerous tissue, the continuous emission of radiation over several weeks leads to tumour cell death. For the Auger electrons to have an even stronger impact, some scientists are looking at ways to integrate Pd-103 into molecules that specifically enter the nucleus. However, most current clinical applications rely on the well-established brachytherapy approach.
Researchers investigating the potential of Pd-103 as an Auger Electron-Emitting Radionuclides emphasise the synergy of photon and electron emissions. The combination might allow for multi-targeted cellular damage, covering both local tumour sites and microscopic disease pockets that might otherwise evade treatment. Over the coming years, new delivery strategies could highlight the Auger electron contribution more effectively, improving patient outcomes in prostate cancer and potentially other malignancies.
Targeting Mechanisms and Delivery Vectors
The effectiveness of Auger electron therapy hinges on delivering the radionuclide into or near the cell nucleus. Various strategies include:
- Monoclonal Antibodies: Engineered to recognise tumour-associated antigens, these antibodies can be labelled with In-111, I-123, I-125, Pt-193m, Pt-195m, Sn-117m, or Pd-103. Once bound, they are internalised, bringing the radionuclide closer to the nucleus.
- Peptides and Proteins: Certain cancers overexpress receptors that can be targeted by peptides. These smaller molecules may show improved tumour penetration. Radiolabelling peptides with In-111 or I-125 have been studied for neuroendocrine tumours.
- Nucleic Acid-Binding Molecules: Some agents can enter the nucleus and bind DNA directly, including oligonucleotides, anthracyclines, or platinum complexes. Incorporating I-125 or Pt-195m within these compounds could amplify the local effect.
- Nanoparticles and Liposomes: Nanotechnological approaches offer controlled release and the possibility of multifunctional platforms. Embedding Sn-117m or Pd-103 in nanoparticles could enable targeted delivery plus imaging capabilities.
Each approach must ensure that the Auger Electron-Emitting Radionuclides remain stable and reach the tumour with minimal loss of radioactivity. Additionally, the clearance of radiopharmaceuticals from healthy organs must be optimised to reduce collateral harm. As production methods improve and supply chains become more robust, there is potential for multiple approaches to converge, offering physicians a range of Auger electron therapies tailored to specific cancer types.
Challenges and Future Directions
Though Auger electron therapy offers a precise method for cell destruction, several hurdles must be overcome:
- Nuclear Localisation: Achieving effective nuclear uptake remains the primary challenge. Surface antigens or cytoplasmic targets may not bring the radionuclide close enough to DNA to maximise cell death.
- Radiopharmaceutical Chemistry: Many Auger Electron-Emitting Radionuclides require careful chelation or incorporation into functional molecules, which can be chemically demanding. In particular, work with Pt-193m or Pt-195m requires developing stable complexes that can be administered safely.
- Production and Availability: Some of these radionuclides, including Sn-117m and Pt-193m, may not be available in large quantities, limiting their widespread clinical adoption.
- Clinical Trial Data: Although preliminary studies with In-111, I-125, and Pd-103 are encouraging, more extensive trials are necessary to establish dosage regimens, side effect profiles, and long-term outcomes.
Looking ahead, research into targeted radiopharmaceuticals is advancing quickly. Combination therapies, where Auger emitters are coupled with other treatments such as chemotherapy or external beam radiation, could yield synergistic tumour kill. New developments in biotechnology, including advanced protein engineering and gene editing, might also improve nuclear targeting. Over time, a more refined understanding of integrating In-111, I-123, I-125, Pt-193m, Pt-195m, Sn-117m, and Pd-103 into therapy regimens should broaden the use of Auger electrons in cancer care.
Conclusion
Auger electron-emitting radionuclides hold promise in the fight against various cancers. By delivering potent radiation directly to a tumour’s DNA, they aim to improve therapeutic outcomes while maintaining a more acceptable toxicity profile. In-111, I-123, I-125, Pt-193m, Pt-195m, Sn-117m, and Pd-103 exhibit intriguing properties that can be harnessed for clinical benefit, provided that targeting and dosimetry challenges are successfully addressed.
Research has already shown positive indications for In-111-labelled antibodies, I-125 brachytherapy seeds, and Pd-103 implants. Work is expanding to explore novel applications, such as platinum-based Auger agents (Pt-193m and Pt-195m) and next-generation nanoparticle carriers for Sn-117m. Additional trials and technological innovations are needed before these approaches become routine. However, the outlook for Auger electron therapy in nuclear medicine remains positive.
Continued collaboration across disciplines—ranging from radiochemistry and molecular biology to oncology and medical physics—will drive the development of safer and more effective Auger electron-emitting radiopharmaceuticals. As we refine our understanding of delivering and sustaining Auger emissions within malignant cells, these radionuclides could become a powerful addition to the therapeutic armamentarium. Their capacity to achieve precision at the cellular level could transform cancer care, offering patients a targeted alternative that minimises harm to healthy tissues.
Disclaimer
The content provided in this article, Selected Auger Electron-Emitting Radionuclides for Therapeutic Nuclear Medicine, is intended for informational and educational purposes only. It does not constitute professional medical advice, diagnosis, or treatment. Open Medscience and its contributors do not endorse or recommend any specific radionuclide, treatment protocol, or medical approach discussed in this publication.
The information presented is based on current scientific understanding as of the date of publication and is subject to change as new research emerges. Readers are encouraged to consult qualified healthcare professionals or medical physicists before making any clinical decisions or pursuing any therapeutic interventions mentioned in this article.
Open Medscience makes no guarantees as to the accuracy, completeness, or suitability of the content for any particular purpose and disclaims all liability for any direct or indirect consequences arising from the use of this material. Mention of specific radionuclides, therapies, or research does not imply endorsement or certification of safety or efficacy.
You are here: home » diagnostic medical imaging blog »