Summary: This article examines the principles and methods involved in electron beam treatment planning within modern radiotherapy. It discusses core factors such as beam energy selection, patient positioning, dose calculation algorithms, beam modifiers, and quality assurance protocols. The aim is to highlight how thoughtful planning and technical refinements contribute to optimal treatment outcomes and improved patient safety.
Keywords: Electron beam therapy; Radiotherapy planning; Beam modulation; Quality assurance; 3D conformal radiotherapy; Dose calculation algorithms.
Introduction to Electron Beam Therapy
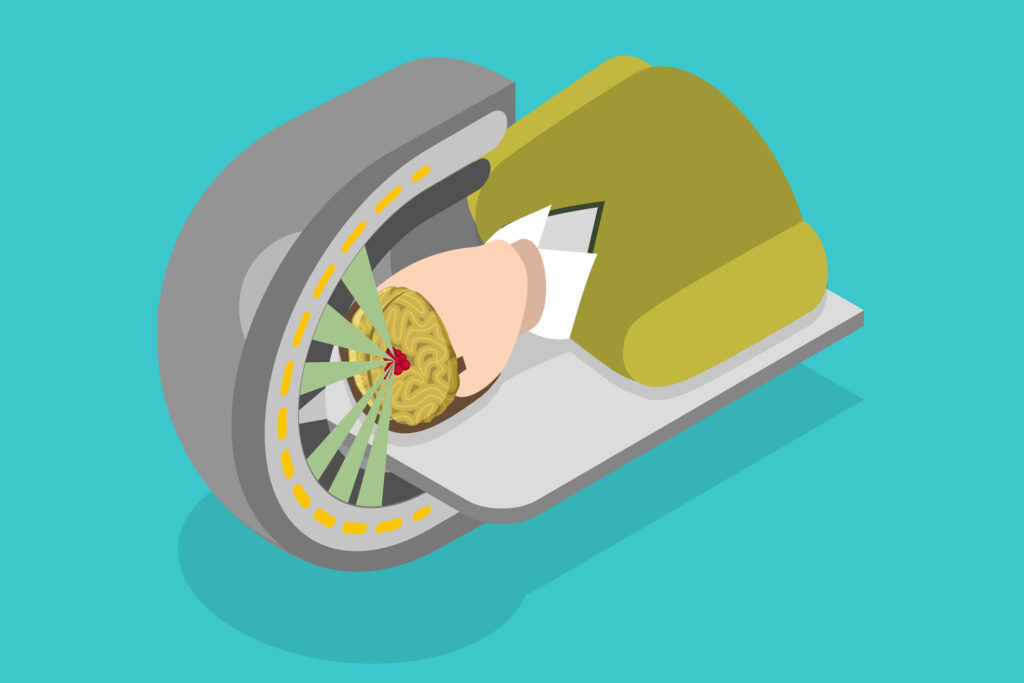
Electron beam therapy remains an important modality in cancer care, offering certain advantages over other radiation types. It is particularly beneficial for treating superficial tumours or clinical targets situated near the skin surface. Through the selection of appropriate beam energy and collimation, clinicians can achieve favourable dose distributions while sparing deeper tissues from unnecessary radiation. Advances in treatment planning systems, imaging techniques, and beam modifiers have further refined electron beam therapy, enabling precise dose placement and decreased toxicity.
Physical Principles of Electron Beam Therapy
Electron beams used in radiotherapy exhibit certain physical properties that differentiate them from photon beams. Electrons have a finite range in tissue, and the dose deposited typically increases to a certain depth (depending on energy) and then drops off sharply. This characteristic makes electron beams useful when the target volume is superficial, as practitioners can confine the highest dose to the tumour while reducing unwanted exposure to deeper tissues.
- Depth–dose relationship: The penetration of an electron beam depends on its energy. Lower-energy beams are more suitable for lesions located very close to the surface, while higher-energy beams can reach deeper targets. However, electrons of higher energy also have a broader penumbra and may introduce more side scatter.
- Electron scattering: Electrons readily scatter in tissue, a characteristic that complicates dose planning if the target has irregular contours or if there are tissue inhomogeneities. Careful attention to inhomogeneity corrections is vital for accurate dose calculation.
- Surface dose: Electron beams deposit a relatively high dose at or near the skin surface. This makes them particularly well-suited for treating skin tumours, post-surgical scars, or other targets requiring a sharp dose fall-off at depth.
Patient Positioning and Immobilisation
Effective treatment planning relies on consistent patient positioning throughout the treatment course. Any variation in patient setup can lead to a mismatch between the planned dose distribution and actual dose delivery. For electron beam therapy, this can be especially important when planning to treat small superficial targets.
- Immobilisation devices: Devices such as thermoplastic masks or customised cushions help restrict patient movement and maintain consistent target placement. A thermoplastic mask might be used for head and neck lesions. For chest wall or extremity lesions, foam-based systems can stabilise limbs in reproducible positions.
- Surface landmarks: Visualising and marking the tumour bed on the skin can help refine setup accuracy. Radiopaque markers can be placed on relevant anatomical features or scars to guide beam alignment during imaging and daily setup.
- Image guidance: Modern radiotherapy often incorporates tools such as cone beam CT or surface imaging for patient alignment. Although these may not be as common for purely superficial electron treatments, certain settings benefit from image guidance, particularly when critical structures lie near the target.
Selection of Beam Energy
Choosing the appropriate electron beam energy is one of the most crucial steps in treatment planning. The primary aim is to ensure adequate dose coverage of the target volume while minimising exposure to underlying tissues.
- Target depth: The planning team needs to carefully estimate tumour depth. The rule of thumb is that electrons should be chosen so that their practical range is slightly beyond the deepest extent of the lesion.
- Beam penetration: Clinicians should be mindful that higher energies produce a more penetrating beam, which may be useful for deeper targets but can also lead to increased dose to normal tissues below the target region.
- Dose build-up and skin-sparing: Electron beams generally deposit a large portion of their dose near the surface, which is beneficial for superficial lesions. However, when dealing with tumours that extend beyond a few centimetres in depth, combining photon and electron beams or using a higher electron energy may be considered.
- Bolus use: For superficial targets, a bolus material (such as a tissue-equivalent gel or wax) can be placed over the skin to shift the depth of maximum dose closer to the surface. Bolus selection depends on the thickness required to achieve the desired dose distribution.
Beam Modifiers and Shaping
The next step in electron beam treatment planning involves tailoring the beam to conform to the treatment site. Beam modifiers and shaping devices allow for more accurate dose placement.
- Customised cutouts: Metal cutouts, typically made from lead or Cerrobend, are inserted into the electron applicator to shape the beam to match the target’s projected contours. Precise cutout creation is important for achieving well-defined field edges and limiting beam spill into surrounding tissues.
- Bolus and thickness compensators: As mentioned, applying a bolus can help achieve the necessary build-up of dose for superficial targets. In some complex treatments, thickness compensators can be used to distribute dose more uniformly across uneven surfaces.
- Feathering fields: When treating larger areas with adjacent electron fields or combining electron and photon beams, field feathering techniques can minimise overlap regions and avoid areas of hot or cold spots.
- Intensity-modulated electron therapy (IMET): Although still less common than intensity-modulated photon therapy (IMRT), IMET employs multiple electron beam segments or intensity patterns. This approach aims to optimise the dose distribution around complex targets, potentially reducing high-dose volumes in healthy tissues. However, the delivery of IMET requires advanced equipment and more sophisticated planning algorithms.
Dose Calculation Algorithms and Treatment Planning Systems
The accuracy of electron beam treatment planning hinges on robust dose calculation algorithms within the planning system. Improvements in computational models have allowed greater precision in determining dose distributions, particularly in heterogeneous anatomical areas such as the sinus region, thorax, or pelvis.
- Pencil beam and Monte Carlo algorithms: Traditional planning systems often used pencil beam algorithms to compute electron dose distributions. However, Monte Carlo simulation is increasingly employed due to its ability to account for complex scatter patterns and tissue irregularities more accurately.
- Heterogeneity corrections: Whenever the beam passes through materials of differing densities (air cavities, bone, implants, or tissue of varying composition), the dose distribution may be altered significantly. Relying on planning algorithms that accurately correct for these inhomogeneities ensures a more reliable estimation of the dose delivered.
- Plan evaluation tools: Modern systems provide various visual and quantitative tools (dose-volume histograms, isodose overlays, 3D rendering of dose distributions) that allow planners to refine beam angles, energies, and field shaping. This iterative process is important to ensure coverage of the clinical target volume while respecting dose constraints for nearby normal tissues and organs at risk.
Quality Assurance and Verification
To maintain a high level of safety and efficacy, rigorous quality assurance (QA) protocols are applied to electron beam therapy. QA checks encompass both machine performance and patient-specific verification.
- Machine calibration: Linear accelerators (LINACs) must be calibrated at regular intervals to ensure the generated electron beams match the expected energy output and dose rates. Minor deviations in beam energy can significantly affect dose distributions in electron beam therapy, so careful routine checks are essential.
- Cutout and applicator QA: Each applicator used in electron beam therapy needs to be checked periodically for mechanical integrity and alignment. Any newly created custom cutout should also be verified to confirm that its shape aligns with the intended field outline.
- Patient-specific QA: Dose verification for especially complex plans can include phantom measurements or in vivo dosimetry. Thermoluminescent dosimeters (TLDs), diodes, or other measurement devices may be positioned on a phantom or directly on the patient’s skin to confirm the planned dose is being delivered accurately.
- Portal imaging: While electron beams are less commonly verified using portal imaging compared to photon beams, some centres still incorporate electronic portal imaging devices (EPIDs) or film-based methods to check field shape and placement before or during treatment.
Clinical Applications and Techniques
Electron beam therapy finds use across a range of clinical scenarios, each requiring specific planning approaches:
- Skin cancers: Electron beams are frequently employed for basal cell carcinoma, squamous cell carcinoma, and melanoma in situ, where superficial dose concentrations can destroy tumour cells while preserving deeper structures. Bolus application and accurate field shaping are typically involved.
- Post-mastectomy chest wall irradiation: In breast cancer, an electron boost may be delivered to the scar or chest wall area. Careful consideration of energy, bolus thickness, and field edges is key to avoiding underdosing the surface and overdosing deeper structures such as the lung and heart.
- Nodal areas: In specific cases, nodal basins that require a boost dose can be targeted with electron beams, particularly if they lie close to the surface. However, the presence of inhomogeneities, such as surgical scars or uneven tissue composition, must be accounted for when planning.
- Total skin electron therapy (TSET): This specialised approach is used in conditions such as mycosis fungoides. It involves delivering a uniform dose to the entire skin surface, typically using extended treatment distances and beam angles that sweep across the patient’s surface.
Emerging Technologies and Future Directions
The technological evolution of electron beam therapy continues to progress. Some new developments focus on refining dose distributions for targets that are not strictly superficial, bridging the gap between what traditional electron beams and photon beams can achieve.
- Magnetic fields: The integration of magnetic fields into treatment delivery can alter the path of electrons, possibly enhancing dose conformation. Research is ongoing to explore whether combined magnetic fields and electron beams might offer a clinically meaningful advantage for selected tumour sites.
- Scanning electron beam systems: Instead of a broad beam, scanning systems can direct small pencil beams in a raster-like pattern across the target. This technique could offer more control over dose distribution, though significant research is still needed to bring it into widespread clinical use.
- Hybrid therapies: In certain scenarios, there is a rationale for combining electron beams with advanced photon-based approaches to produce a more selective dose distribution. For instance, a photon IMRT plan might be complemented by an electron patch field to boost superficial regions that are at high risk of recurrence.
- Automation and artificial intelligence: Machine learning and algorithm-based optimisations are expected to facilitate more efficient and potentially more accurate planning. By analysing large datasets, AI-driven software can identify the most suitable beam configurations for specific tumour sites, potentially reducing planning time and improving consistency.
Practical Planning Considerations
When planning electron beam therapy, clinical teams should follow a systematic approach:
- Define the target: Through diagnostic imaging and clinical examination, carefully delineate the tumour volume or surgical bed. For superficial lesions, marking the surface location is crucial.
- Select beam parameters: Choose the optimum beam energy based on target depth and desired coverage. Then, determine appropriate beam angles and any additional measures required for beam shaping, such as cutouts or bolus layers.
- Verify dose distribution: Perform a thorough check of the planned dose distribution in the context of normal tissue tolerance. Adjust parameters as necessary to minimise hot or cold regions, especially where target boundaries or critical structures meet.
- Prepare for treatment delivery: Ensure that all necessary equipment, including applicators and cutouts, is ready and in good condition. Establish a reproducible patient setup and place any bolus or markings correctly each day.
- Monitor and adapt as needed: Throughout the course of treatment, monitor patient positioning and tumour response. If necessary, adapt the plan to accommodate any anatomical changes or shifting surface landmarks.
Conclusion
Electron beam therapy provides an effective solution for treating superficial tumours, thanks to its dose characteristics that concentrate radiation near the surface while sparing underlying structures. Through careful attention to beam energy selection, cutout shaping, bolus usage, and thorough QA procedures, clinicians can deliver highly targeted doses that address the tumour while reducing treatment toxicity.
Ongoing advances in treatment planning systems, imaging technologies, and beam delivery methods promise to enhance the precision and utility of electron beam therapy further. Researchers are working on adapting new ideas—including magnetic fields, scanning electron beams, and AI-driven planning—so that electron beams could serve a broader range of clinical scenarios.
In the clinical environment, it is essential to remain current with these developments and to integrate them thoughtfully into practice, always prioritising patient safety and outcome quality. Although electron therapy is sometimes overshadowed by other radiotherapy approaches, it remains a key option in the modern radiotherapy arsenal. By continuously refining electron beam treatment planning, practitioners can help ensure patients receive the safest, most accurate radiation treatments possible.
Disclaimer
The content presented in this article, Precision Techniques for Advanced Electron Beam Treatment Planning, is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment recommendations. Clinicians and medical professionals should rely on their own expertise, training, and clinical judgement when interpreting or applying the information provided. Readers are encouraged to consult relevant national and local guidelines, as well as peer-reviewed sources, before implementing any clinical or technical procedures discussed herein.
Open Medscience and the article’s contributors accept no responsibility for any consequences arising from the use or misuse of information contained in this publication. The views expressed are those of the author(s) and do not necessarily reflect those of Open Medscience or affiliated institutions.
You are here: home » diagnostic medical imaging blog »