Proton beam therapy represents a significant advancement in cancer treatment, offering a more targeted approach than conventional radiotherapy. This innovative therapy utilises protons to attack cancer cells precisely, minimising damage to surrounding healthy tissues and reducing side effects. The following article outlines the mechanism of proton beam therapy and its benefits, applications, and challenges in broader healthcare integration.
Introduction to Proton Beam Therapy in Cancer Care
Cancer, a multifaceted and often devastating disease, continues to stand as a significant global health challenge, leading to millions of deaths annually. The relentless pursuit of more effective, less harmful treatment options has propelled medical science into new areas of innovation and discovery. Among these advancements, proton beam therapy (PBT) has emerged as a beacon of hope, offering a sophisticated approach to cancer treatment that promises to improve outcomes while minimising adverse effects.
At its core, proton beam therapy is a form of radiotherapy that uses protons instead of X-rays to treat cancer. Unlike conventional radiotherapy, which uses photons to destroy cancerous cells, PBT harnesses the unique physical properties of protons—subatomic particles with a positive charge—to target tumours with unparalleled precision. This high degree of accuracy is pivotal in the treatment of cancer, particularly for tumours located near critical organs or within sensitive areas of the body where traditional radiotherapy risks significant collateral damage.
The inception of proton beam therapy is the result of scientific evolution, tracing back to the mid-20th century when the theoretical and practical foundations of using charged particles for medical treatment were laid. However, it wasn’t until the closing decades of the century that technological advancements made its application feasible in clinical settings. Today, PBT represents the confluence of physics and medical science, a testament to how interdisciplinary collaboration can yield revolutionary healthcare solutions.
The mechanism that sets proton beam therapy apart is the Bragg peak—a phenomenon wherein protons decelerate and deposit the bulk of their energy at a specific depth before coming to a stop. This allows oncologists to control where the radiation dose is delivered precisely, targeting the tumour with maximum intensity while sparing the surrounding healthy tissues. The significance of this cannot be overstated, as it reduces the likelihood of the side effects commonly associated with radiation therapy, such as fatigue, skin damage, and the risk of inducing secondary cancers.
Furthermore, proton beam therapy has the ability to minimise damage to non-cancerous cells and is particularly beneficial in treating cancers in paediatric patients, who are more susceptible to the long-term consequences of radiation exposure. It also presents a viable option for treating complex or recurrent cancers where other treatment modalities may have reached their limits of safety and efficacy.
Although it has potential, the adoption of proton beam therapy into mainstream cancer care faces obstacles. The high cost of constructing and operating PBT facilities and the need for specialised training for medical staff poses significant challenges. Moreover, the clinical benefits of PBT over conventional radiotherapy are still a subject of ongoing research, with the medical community seeking to establish more comprehensive evidence through clinical trials and comparative studies.
Proton beam therapy stands at the frontier of cancer treatment, embodying the progress and potential of modern medical science. As research continues to unlock its capabilities and technology evolves to make it more accessible, PBT could significantly alter the landscape of cancer care, offering patients treatment options that are more effective and kinder to the body. In this ongoing battle against cancer, proton beam therapy shines as a prime example of how innovation can lead to safer, more precise, and more compassionate medical treatments.
The Science Behind Proton Beam Therapy
The essence of proton beam therapy (PBT) lies in its innovative use of protons, the positively charged particles at the centre of every atomic nucleus. This advanced form of cancer treatment diverges significantly from traditional radiotherapy by utilising the intrinsic physical properties of these particles, marking a significant evolution in our approach to combating cancer. The science underpinning PBT is both fascinating and complex, involving principles of physics that allow for the targeted destruction of cancerous cells while preserving the surrounding healthy tissues.
Unlike the photons used in conventional radiotherapy, Protons possess mass and can be precisely manipulated to deliver energy to a specific depth within the body. This ability stems from a unique characteristic of protons known as the Bragg peak. The Bragg peak refers to the point at which protons decelerate rapidly and deposit the majority of their kinetic energy in a concentrated area. Beyond this peak, the protons release minimal additional energy, drastically reducing the dose received by tissues past the tumour. This sharply contrasts with traditional radiation, where photons continue to deposit energy as they exit the body, thereby increasing the risk of damage to healthy tissues and organs.
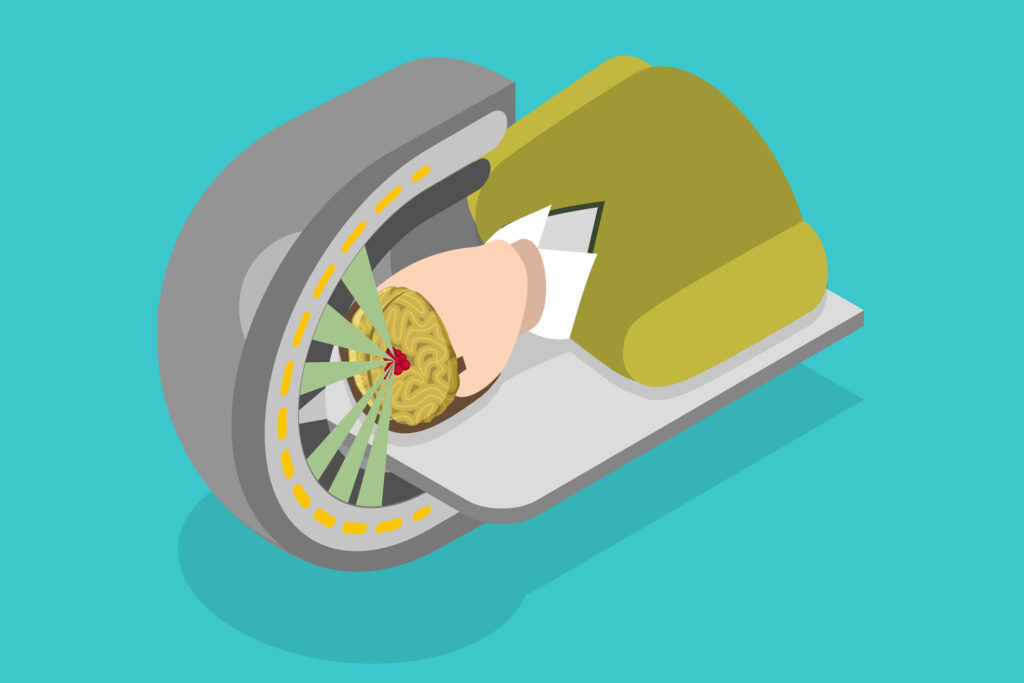
The journey of protons in PBT begins with their acceleration to high velocities using a cyclotron or synchrotron—complex machines that propel the protons to speeds close to that of light. Once accelerated, the protons are directed through a nozzle and precisely targeted at the tumour. Advanced imaging techniques, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), are used to determine the tumour’s exact location and shape, ensuring the proton beam is accurately focused.
The real magic of PBT lies in its ability to be tailored to the specific dimensions of a tumour. By adjusting the energy of the protons, oncologists can control the depth of the Bragg peak within the body, ensuring that the maximum energy dose is delivered directly to the cancerous cells. This level of precision is particularly advantageous for treating tumours that are near critical organs or structures, such as the brain, eyes, or spinal cord, where conventional therapy might risk significant collateral damage.
Moreover, the science of PBT opens up new possibilities for treating cancers that were previously considered difficult or even impossible to address with radiation. For example, paediatric cancers, where long-term side effects of radiation are a significant concern, can be treated more safely with protons due to the reduced risk of damaging developing tissues.
Despite its advantages, the application of PBT is not without challenges. The complexity of the technology involved translates into high operational costs and the need for specialised facilities and training. Additionally, the precise nature of proton therapy requires meticulous planning and execution to ensure that the treatment is delivered accurately and effectively.
However, the science behind proton beam therapy represents a remarkable fusion of physics and medicine, offering a sophisticated and refined approach to cancer treatment. By harnessing the unique properties of protons and the Bragg peak effect, PBT can target tumours with unprecedented precision, minimising harm to healthy tissues and opening up new avenues for treating a wide range of cancers. As research progresses and technological advancements continue, the potential of proton beam therapy to transform cancer care remains vast, promising a future where treatments are more effective and significantly less detrimental to the patient’s overall health.
Mechanism of Action of Proton Beam Therapy
Proton beam therapy (PBT) represents a pinnacle of precision in cancer treatment. It leverages advanced physics to target malignancies more accurately and with fewer side effects than traditional radiotherapy. The mechanism of action for PBT is a fascinating interplay of technology, physics, and biology, culminating in a treatment modality that can pinpoint cancer cells with remarkable precision.
The Role of Particle Accelerators
The journey of a proton in therapy begins in a particle accelerator, such as a cyclotron or synchrotron. These sophisticated machines accelerate protons to a significant fraction of the speed of light, imbuing them with the high energies necessary for penetrating the body and reaching tumours at varying depths. The choice between a cyclotron or synchrotron often depends on the specific requirements of the treatment plan, including the energy levels needed and the versatility required for different types of tumours.
Pathway of Protons to the Tumour
Once accelerated, these protons are meticulously steered towards the patient’s tumour using a series of magnetic fields. This guidance system is incredibly precise, allowing for adjustments in real-time to ensure that the proton beam remains on target. As the protons travel through the body, they interact minimally with the surrounding tissues. This starkly contrasts traditional radiation therapy, where photons scatter within the body, affecting both the tumour and surrounding healthy tissue.
Reaching the Target: The Bragg Peak
The hallmark of proton beam therapy’s mechanism of action is the utilisation of the Bragg Peak. This phenomenon occurs when the protons slow down as they penetrate deeper into the tissue, releasing the majority of their energy at a specific, predetermined depth. By controlling the energy of the protons, clinicians can adjust where this peak occurs, ensuring that the highest dose of radiation is delivered directly to the tumour. This precision reduces the radiation exposure of healthy tissues both before and beyond the tumour, a critical advantage over traditional methods.
DNA Damage and Cell Death
The energy released by the protons at the Bragg Peak induces direct and indirect damage to the DNA of cancer cells. The direct damage involves breaking the DNA strands, while the indirect damage is caused by the generation of free radicals within the cells. These radicals are highly reactive molecules that can also break DNA strands or cause mutations. Cancer cells are less effective at repairing this DNA damage than healthy cells, leading to their destruction. This targeted approach allows for the treatment of tumours with higher doses of radiation while minimising the risk to surrounding healthy tissues, ultimately leading to improved patient outcomes.
Beyond the Bragg Peak
Advanced delivery techniques, such as pencil beam scanning, further refine the proton therapy’s mechanism of action. This method allows for a more dynamic administration of the proton beam, “painting” the tumour with radiation and adapting to its shape and depth with even greater precision. This adaptability is especially beneficial for irregularly shaped tumours or those located near critical structures.
Therefore, the mechanism of action of proton beam therapy underscores its role as a groundbreaking treatment in oncology. Through the use of particle accelerators, precise targeting, and the unique advantages offered by the Bragg Peak, PBT delivers a potent combination of efficacy and safety. This sophisticated approach damages the DNA of cancer cells, leading to their destruction, and preserves the integrity and function of surrounding healthy tissues, heralding a new era in cancer treatment.
Benefits of Proton Beam Therapy
Proton beam therapy (PBT) represents a significant advancement in the field of oncology, offering a host of benefits over traditional radiation therapy. Its unique approach to targeting cancer cells provides patients with a treatment option that is not only effective but also minimises the potential for side effects and long-term complications. Here, we look into the primary advantages of proton beam therapy, including its reduced side effects, increased precision, and versatility, which collectively contribute to its growing recognition as a preferred treatment modality for various types of cancer.
Reduced Side Effects
One of the most significant benefits of proton beam therapy lies in its ability to minimise side effects. Traditional radiation therapy, which uses X-rays or gamma rays, can damage both cancerous and healthy tissues as the radiation passes through the body. In contrast, PBT employs protons that deposit the bulk of their energy at a specific depth (the Bragg peak) before stopping, thereby sparing the surrounding healthy tissues from unnecessary radiation exposure. This targeted approach significantly reduces the risk of side effects, such as skin irritation, fatigue, and the potential for secondary cancers, which are often associated with conventional radiotherapy. For patients, this means a treatment process that is less taxing on the body and allows for a quicker return to daily activities and an improved quality of life during and after treatment.
Increased Precision
The hallmark of proton beam therapy is its unparalleled precision in targeting tumours. By exploiting the properties of the Bragg peak, PBT can deliver high doses of radiation directly to the cancer cells while minimising the impact on adjacent healthy tissues. This precision is particularly advantageous when treating tumours located near critical structures or organs where the margin for error is minimal. For instance, in cases of brain cancer, paediatric cancers, or tumours near the spinal cord, PBT can effectively eradicate cancer cells without compromising the functionality of these vital areas. The ability to safely deliver higher radiation doses to the tumour may also enhance the overall effectiveness of the treatment, potentially leading to better outcomes for patients.
Versatility
Proton beam therapy’s versatility further underscores its benefits. Its applicability across a wide range of cancers, including those in challenging or sensitive locations, demonstrates its potential as a universal tool in the oncologist’s arsenal. PBT is particularly effective in treating paediatric cancers, where the long-term side effects of radiation exposure are a significant concern. Children’s growing tissues are more susceptible to radiation-induced damage, and the precision of proton therapy offers a safer alternative, reducing the risk of growth abnormalities and secondary cancers. Additionally, for cancers of the brain, spine, and eye, where preserving the surrounding healthy tissue is crucial, PBT provides an effective treatment solution that traditional radiotherapy cannot match.
The benefits of proton beam therapy mark a paradigm shift in cancer treatment. Its ability to minimise side effects and its increased precision and versatility make it an invaluable treatment modality. As technology advances and access to PBT expands, its role in providing more effective, less harmful cancer treatments is set to increase, offering hope to patients facing the daunting journey of cancer treatment.
Clinical Applications of Proton Beam Therapy
Proton beam therapy (PBT) has carved a niche for itself in the landscape of cancer treatment with its precision and efficacy, particularly for tumours that are challenging to treat with conventional radiotherapy. This advanced form of treatment has broadened the horizon of clinical applications, offering new hope to patients with complex cancer cases. Its ability to precisely target tumours while sparing nearby healthy tissues makes it an ideal choice for cancers located near vital organs or structures, paediatric cancers, and situations where the risk of collateral damage from conventional radiotherapy is unacceptably high.
Treating Cancers Near Critical Structures
One of the most compelling applications of proton beam therapy is in treating cancers situated close to critical structures. Traditional radiotherapy can inadvertently damage healthy tissues and organs adjacent to the tumour, leading to significant side effects and impacting the patient’s quality of life. PBT, however, with its targeted approach, allows for the delivery of high-dose radiation to the tumour with minimal impact on surrounding healthy tissues. This precision is particularly crucial in cases of brain tumours, where safeguarding the surrounding neural tissue and critical structures is essential for maintaining cognitive functions and quality of life. Similarly, in head and neck cancers, PBT can target the malignancy without damaging the salivary glands, spinal cord, or brain, reducing complications such as dry mouth, difficulty swallowing, and radiation-induced spinal cord injuries.
Paediatric Cancers
Children are especially susceptible to the adverse effects of radiation due to their developing bodies and the potential for long-term complications, including secondary cancers. The precision of proton beam therapy offers a significant advantage in treating paediatric cancers, as it reduces the exposure of healthy tissues to radiation, thereby minimising the risk of growth abnormalities and secondary malignancies. Paediatric brain tumours, for example, can be treated more safely with PBT, as it spares healthy brain tissue and reduces the risk of cognitive deficits. This targeted approach improves the immediate outcomes of cancer treatment and contributes to a better long-term quality of life for young patients.
Prostate Cancer and Other Applications
Prostate cancer represents another area where proton beam therapy has shown promising results. Given the prostate’s proximity to the bladder and rectum, traditional radiotherapy can lead to urinary and gastrointestinal side effects. PBT allows for precise targeting of the prostate, significantly reducing radiation exposure to adjacent organs and, consequently, the risk of these side effects. This precision does not compromise the treatment’s effectiveness against the cancer itself, making PBT a preferred option for many patients with prostate cancer.
Moreover, PBT’s clinical applications extend to various other cancers, including but not limited to lung, breast, and gastrointestinal cancers. In each case, the therapy’s ability to deliver high doses of radiation directly to the tumour while sparing healthy tissue offers a distinct advantage, potentially enhancing treatment outcomes and reducing the likelihood of complications.
The clinical applications of proton beam therapy are vast and varied, offering a safer and more effective treatment option for a wide range of cancers. Its precision and reduced risk of side effects make it particularly beneficial for tumours near critical structures, paediatric cancers, and cases where conventional radiotherapy’s risks outweigh its benefits. As technology advances and access to PBT improves, its role in cancer treatment is set to expand, providing hope and improved outcomes for patients facing this challenging disease.
Challenges and Limitations of Proton Beam Therapy
Proton beam therapy (PBT) stands out as a groundbreaking advancement in cancer treatment, promising improved precision and reduced side effects. However, several significant challenges and limitations hinder its integration into mainstream healthcare and accessibility to patients. The primary obstacles facing PBT today are the high establishment and operation costs, limited availability of treatment centres, and the need for comprehensive evidence and research to validate its long-term benefits over traditional therapies.
High Costs
Its cost is one of the most formidable barriers to the widespread adoption of proton beam therapy. The initial investment required to set up a proton therapy facility is substantial, often running into hundreds of millions of dollars. This expense is due to the sophisticated equipment needed, such as cyclotrons or synchrotrons, and the construction of specialised facilities capable of housing this technology. The high operational costs, including maintenance of the equipment and the need for highly specialised personnel to operate the machinery and plan treatments, further contribute to the overall expense. As a result, the cost of treatment with PBT can be significantly higher than that of conventional radiotherapy, making it less accessible to a broad segment of patients and challenging to incorporate into healthcare systems, especially in countries with limited healthcare funding.
Limited Availability
The availability of proton beam therapy is another significant challenge. Due to the high costs associated with establishing and operating PBT centres, their number is relatively small worldwide. This scarcity means that access to proton therapy is limited, with many patients unable to benefit from this treatment option unless they are willing to travel long distances, often at great personal and financial cost. The concentration of facilities in certain regions or countries further exacerbates disparities in access to advanced cancer treatments, leaving many patients with fewer options.
Evidence and Research
While proton beam therapy has shown promise in treating various types of cancer, there is still a need for more comprehensive evidence to support its efficacy and cost-effectiveness compared to traditional radiation therapies. The field requires ongoing research and well-designed clinical trials to fully understand PBT’s long-term benefits, potential limitations, and optimal applications. Comparative studies are particularly crucial to determine whether the advantages of proton therapy translate into significantly better treatment outcomes and justify the higher costs. Without robust data supporting its superiority or demonstrating significant improvements in patient outcomes, the adoption of PBT by healthcare providers and its coverage by insurance companies may be limited.
Furthermore, as PBT is a relatively new treatment compared to traditional radiotherapy, long-term data on patient outcomes, including survival rates and quality of life, are still being collected. This information is vital for evaluating the true benefit of proton therapy and guiding treatment decisions for various cancers.
While proton beam therapy offers a promising and technically advanced approach to cancer treatment, its widespread adoption is hindered by high costs, limited availability, and the need for more extensive research. Overcoming these challenges will require concerted efforts from the medical community, healthcare policymakers, and researchers to make PBT more accessible and to provide definitive evidence of its benefits. As the technology evolves and more data becomes available, the role of PBT in cancer care may become more clearly defined, potentially leading to broader implementation and improved outcomes for patients worldwide.
The Future of Proton Beam Therapy
The landscape of cancer treatment is on the cusp of a transformative shift with the evolution of proton beam therapy (PBT). As a highly precise and less invasive alternative to conventional radiotherapy, PBT has already marked its territory in the area of oncological advancements. The future of PBT shines brightly, driven by technological innovations, decreasing costs, and expanding research, which collectively promises to elevate its role in cancer care to new heights.
Technological Advances and Cost Reduction
A pivotal factor that will shape the future of proton beam therapy is the advancement in technology, particularly in making PBT more affordable and accessible. As the demand for PBT grows, there is a concerted effort within the industry to develop more compact and cost-effective proton therapy systems. These newer models, which are smaller and more efficient than their predecessors, are expected to significantly reduce the financial barriers associated with setting up and operating PBT facilities. This trend towards miniaturisation and increased efficiency makes PBT a more viable option for a wider range of healthcare settings and paves the way for a more extensive global footprint of proton therapy centres.
Expanding Clinical Applications Through Research
Ongoing research and clinical trials are pivotal in expanding the clinical applications of proton beam therapy. As we gain deeper insights into the comparative effectiveness of PBT against traditional therapies across various cancer types, its utility is likely to broaden. Research efforts are also focused on understanding the long-term outcomes of PBT, including survival rates, quality of life, and the incidence of secondary cancers, which are crucial metrics for evaluating any cancer treatment’s success. This growing body of evidence will be instrumental in establishing PBT as a standard treatment option for a wider array of cancers, including those for which its benefits are currently underexplored.
Innovations in Precision and Efficacy
Innovations such as pencil beam scanning (PBS) highlight the ongoing advancements in proton therapy technology. PBS, a method that allows for even more precise dose delivery by modulating the intensity of the proton beam across the tumour, exemplifies the cutting-edge research aimed at maximising the therapeutic potential of PBT. By enabling more accurate conformity to the shape of complex tumours and reducing radiation exposure to adjacent healthy tissues, PBS and similar technologies are set further to enhance the efficacy and safety of proton therapy.
Conclusion
Proton beam therapy stands at the frontier of oncological innovation, offering new hope for patients seeking effective and less harmful cancer treatments. Despite the hurdles of cost and accessibility, the trajectory of PBT points towards a future where these challenges are mitigated by technological progress and expanded research. As we move forward, integrating advanced imaging techniques, developing more compact proton therapy systems, and accumulating robust clinical data are expected to solidify PBT’s position as a cornerstone of modern cancer treatment.
Disclaimer
The content of this article, “Proton Beam Therapy: A New Horizon in Precision Oncology”, is intended for informational and educational purposes only and does not constitute medical advice, diagnosis, or treatment. Open Medscience makes every effort to ensure the accuracy of the information presented at the time of publication; however, advances in research, changes in medical guidelines, and individual clinical circumstances may affect the applicability of the content.
Readers are advised to consult qualified healthcare professionals for personalised medical advice and before making decisions regarding any medical treatment, including proton beam therapy. The article does not replace a consultation with a medical professional and should not be used as the basis for any healthcare decision.
Open Medscience, its authors, and contributors do not assume any liability for any direct, indirect, incidental, or consequential damages resulting from the use or interpretation of the information contained in this article.
You are here: home » diagnostic medical imaging blog »