Summary: FLASH radiotherapy is an exciting development in cancer care that delivers radiation at ultra-high speeds. Early research suggests that it can kill tumours effectively while causing significantly less harm to healthy tissues compared to standard radiotherapy. This article examines what FLASH radiotherapy is, how it works, where the current research stands, and what it may mean for future cancer patients.
Keywords: FLASH radiotherapy, cancer treatment, high dose rate, tumour control, radiotherapy innovation, side effects
What Is FLASH Radiotherapy?
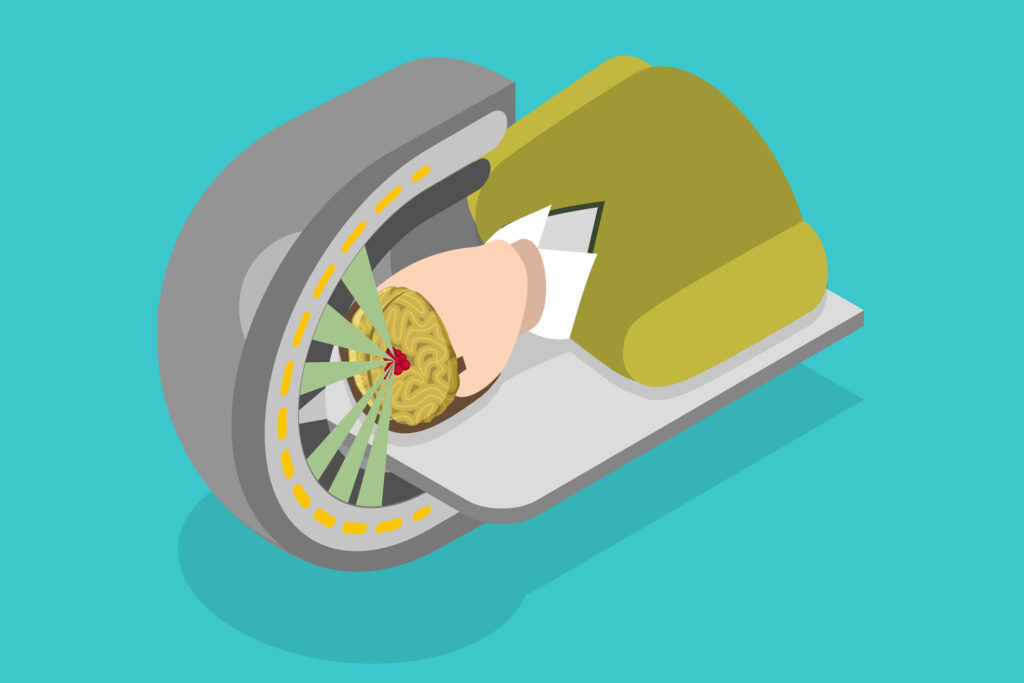
FLASH radiotherapy is a new type of cancer treatment that uses radiation—just like traditional radiotherapy—but does it at an incredibly fast speed. Standard radiotherapy gives small amounts of radiation over several minutes. FLASH, on the other hand, delivers the entire dose in less than a second.
This ultra-rapid method is currently being studied because it appears to have an unexpected benefit: it damages cancer cells just as well as normal radiotherapy, but causes significantly less harm to surrounding healthy tissue.
This surprising benefit is known as the “FLASH effect”, and it could mean fewer side effects and better quality of life for cancer patients.
How Does It Work?
Scientists are still figuring out exactly why FLASH works the way it does. But here are some of the main ideas:
- Oxygen levels: FLASH might use up oxygen in normal tissue so quickly that it temporarily becomes more resistant to radiation. Cancer cells, which are already low in oxygen, don’t get this protection.
- Lower inflammation: FLASH appears to trigger less inflammation and swelling in healthy tissues compared to standard radiotherapy.
- Faster repair in normal cells: Some studies suggest that healthy cells may be more effective at repairing themselves after FLASH treatment compared to cancer cells.
Although these theories are still being tested, the overall pattern is clear: FLASH has a unique way of protecting healthy tissue.
What Have Studies Shown So Far?
Most research on FLASH has been conducted in animals and has consistently shown:
- Less damage to the lungs, brain, and skin
- Fewer long-term side effects
- Just as much cancer control as conventional radiotherapy
One landmark study in France even used FLASH on a person for the first time in 2019 to treat a type of skin lymphoma. The treatment was effective, and the side effects were minimal.
Since then, early-stage trials have started in Europe and the US. Some are looking at using FLASH to relieve pain from bone cancer, while others are testing it on skin and breast tumours.
What Makes FLASH Different from Regular Radiotherapy?
Here are the key differences:
| Feature | Conventional Radiotherapy | FLASH Radiotherapy |
| Dose rate | ~0.01–0.1 Gy/second | ≥40 Gy/second |
| Treatment time | Several minutes | Less than 1 second |
| Effect on healthy tissue | More damage | Much less damage |
| Effect on the tumour | Strong | Equally strong |
| Current clinical use | Standard in hospitals | Still experimental |
Because FLASH delivers the dose in a tiny fraction of a second, patients may one day be able to undergo treatment in the time it takes to blink.
What Are the Challenges?
As promising as it sounds, FLASH radiotherapy isn’t yet ready for widespread use. Here’s why:
- Technology limits: Most hospital machines can’t deliver radiation that fast. Special equipment has to be developed or adapted.
- Only works for some tumours (for now): Currently, FLASH is primarily used for tumours near the surface, as the high-speed beams don’t penetrate deeply into the body. Researchers are working on FLASH using proton and X-ray beams, which can go deeper.
- Not fully understood: Scientists still need to figure out exactly when and why the FLASH effect happens, and whether it works for all types of cancers and tissues.
- Lack of long-term data: We currently lack information on the potential long-term side effects or the safety of this treatment over extended periods.
Despite these challenges, the momentum behind FLASH research is growing quickly.
What’s Happening Now?
Several clinical trials are currently underway worldwide. Here are a few examples:
- FAST-01 and FAST-02 (United States): Studying FLASH for easing bone pain in patients with cancer.
- FLASHKNiFE (France): Looking at FLASH for tumours close to the skin using electron beams.
- UK-based research: Teams in Oxford and Manchester are working on the biology and technology of FLASH, preparing for clinical trials in the UK.
Companies are also developing new machines that can deliver FLASH treatment safely and accurately.
What Could the Future Look Like?
If all goes well, FLASH radiotherapy could change how we treat cancer in several ways:
- Fewer side effects: Patients might experience less fatigue, skin damage, and organ injury.
- Shorter appointments: Whole treatments could be done in a single flash, which would be especially helpful for elderly or frail patients.
- Better quality of life: Reducing harm to healthy tissue could make recovery faster and more comfortable.
- New combinations: FLASH might be used in conjunction with chemotherapy or immunotherapy to enhance the effectiveness of treatments.
In time, FLASH could become a standard part of cancer care, especially for cancers where side effects from radiotherapy are a big problem.
Final Thoughts
FLASH radiotherapy is one of the most exciting developments in cancer treatment in decades. Its ability to spare healthy tissue while still fighting tumours could be a game-changer. Although there are hurdles to overcome, the early results are encouraging, and the research is progressing rapidly.
For patients, FLASH could mean more effective treatments with fewer lasting effects. For healthcare systems, it could provide faster and more efficient care. And for researchers, it opens up a whole new field of questions—and possibilities.
Disclaimer
The information provided in this article is for general informational purposes only and is not intended as medical advice, diagnosis, or treatment. FLASH radiotherapy remains an experimental technique and is not yet widely available or approved for routine clinical use. While early research is promising, further studies are required to determine its safety, effectiveness, and suitability for different types of cancer.
Readers should not rely solely on the content of this blog for decisions regarding their health. Always consult a qualified healthcare professional for advice on any medical condition or treatment option. Open Medscience does not endorse any specific treatment or therapy and accepts no liability for any loss or damage arising from the use of the information contained in this publication.
You are here: home » diagnostic medical imaging blog »