Summary: Medical imaging is a cornerstone of modern healthcare, allowing clinicians to diagnose, monitor, and treat a wide range of conditions with greater accuracy and efficiency. From X-rays and ultrasounds to CT scans and MRI, these technologies have revolutionised diagnostic medicine. This article looks at the fundamentals of medical imaging, its major modalities, the importance of safety protocols, recent advancements, and its role in shaping the future of patient care.
Keywords: Medical imaging, radiology, diagnostic tools, MRI, CT scan, healthcare technology
Understanding Medical Imaging
Medical imaging refers to the techniques and processes used to create visual representations of the interior of a body for clinical analysis and medical intervention. It is essential in diagnosing a wide range of medical conditions, guiding treatment decisions, and monitoring therapeutic outcomes. This non-invasive approach helps clinicians obtain critical anatomical and functional information without the need for surgical exploration.
The history of medical imaging began with the discovery of X-rays by Wilhelm Conrad Roentgen in 1895, a breakthrough that led to the rapid development of radiological medicine. Today, the field has expanded to encompass a range of imaging techniques, each with its own strengths and limitations.
The Main Modalities in Medical Imaging
There are several primary modalities used in medical imaging, each serving specific diagnostic needs depending on the clinical question.
X-ray Imaging
X-ray is the oldest and most commonly used form of medical imaging. It works by passing ionising radiation through the body to capture images of dense tissues such as bones. While it provides limited soft tissue detail, it remains indispensable for detecting fractures, infections, and abnormalities in the chest, such as pneumonia or lung cancer.
Computed Tomography (CT)
CT scanning builds on the principles of X-ray imaging, taking multiple cross-sectional images to construct a three-dimensional representation of the body. It provides more detail than standard X-rays and is particularly useful in evaluating trauma, detecting tumours, and guiding complex surgical procedures. CT is a rapid and widely available tool, though it does involve a higher dose of radiation.
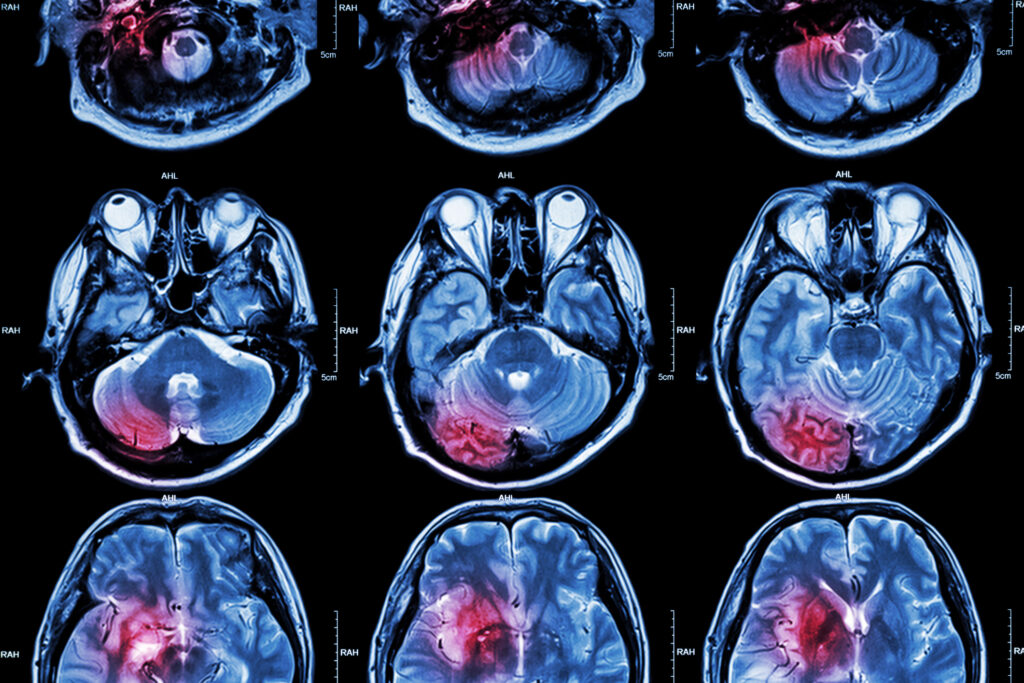
Magnetic Resonance Imaging (MRI)
MRI uses strong magnetic fields and radio waves to produce detailed images of organs and tissues. It is especially useful in neurology, orthopaedics, and cardiovascular medicine. Unlike CT, MRI does not use ionising radiation, making it safer for repeated use. However, it is more expensive, slower, and contraindicated in patients with certain implants or metal fragments.
Ultrasound
Ultrasound employs high-frequency sound waves to produce real-time images. It is commonly used in obstetrics to monitor foetal development, as well as in cardiology, emergency medicine, and guided procedures. It is safe, portable, and cost-effective, although image quality can be highly dependent on the operator.
Nuclear Medicine and PET Scans
Nuclear imaging involves administering small amounts of radioactive substances to assess organ function and detect diseases such as cancer, thyroid disorders, and cardiac conditions. Positron Emission Tomography (PET) is a type of nuclear imaging that shows how tissues and organs are functioning, often combined with CT for anatomical localisation.
Image-Guided Interventions
Beyond diagnostics, medical imaging also plays a key role in guiding minimally invasive procedures. Interventional radiology enables clinicians to perform biopsies, drain fluids, place stents, and treat vascular diseases with precision, guided by imaging to direct instruments. These procedures reduce the need for open surgery, lower risk, and offer quicker recovery times.
Ultrasound, CT, and fluoroscopy are frequently used to assist in these interventions, which are increasingly becoming standard practice in hospitals worldwide. As technology continues to evolve, the accuracy and applications of image-guided interventions are set to expand further.
Safety and Radiation Considerations
While medical imaging provides substantial clinical benefits, it is not without risks, particularly those involving ionising radiation. Excessive exposure can increase the risk of cancer, which is why imaging must always be justified and optimised.
The principle of ALARA – “As Low As Reasonably Achievable” – is central to radiological safety, aiming to minimise patient dose while maintaining diagnostic image quality. Shielding, appropriate technique selection, and modern equipment design all contribute to safer imaging practices.
MRI, which does not use ionising radiation, poses different safety challenges, such as the risks posed by strong magnetic fields to metal implants or devices. Comprehensive safety screening and staff training are, therefore, critical components of MRI practice.
The Role of the Radiologist
Medical images require expert interpretation, and this is where the radiologist comes in. Radiologists are medical doctors trained to analyse imaging studies and provide reports that aid in diagnosis and treatment planning. Their expertise is crucial in distinguishing normal anatomy from pathology and advising referring clinicians on the best imaging strategy.
Radiologists often subspecialise in areas such as musculoskeletal, neurological, or abdominal imaging, contributing to multidisciplinary teams in hospital settings. In recent years, their role has expanded to include active participation in patient care, particularly in interventional procedures and multidisciplinary diagnostic discussions.
Technological Innovations and AI in Imaging
The field of medical imaging is experiencing rapid technological growth, with innovations enhancing image quality, diagnostic accuracy, and workflow efficiency. High-resolution imaging, 3D reconstruction, and functional imaging are becoming standard in many departments. Hybrid machines, such as PET-CT and PET-MRI, combine structural and functional data, offering comprehensive assessments in oncology and neurology.
Artificial Intelligence (AI) is also making a substantial impact. AI algorithms are being developed to assist in image interpretation, detect abnormalities, and even predict disease progression. While these tools are not intended to replace radiologists, they offer support in reducing reporting times and increasing consistency.
Automated image segmentation, anomaly detection, and workflow optimisation are just a few examples of how AI is reshaping imaging services. However, concerns about data privacy, diagnostic accountability, and algorithmic bias remain and must be addressed as these technologies become more embedded in clinical practice.
Education and Training
Medical imaging professionals include radiologists, radiographers, and sonographers, each with specific training and responsibilities. Radiographers operate imaging equipment and ensure patient safety, while sonographers specialise in performing ultrasound examinations. All imaging professionals require extensive education, technical skill, and ongoing training to keep pace with technological advances and regulatory standards.
In the UK, the Health and Care Professions Council (HCPC) regulates radiographers, ensuring their competence and adherence to ethical practice. Continuing Professional Development (CPD) is mandatory, reflecting the dynamic nature of medical imaging and the continual release of new techniques and protocols.
Challenges and Ethical Considerations
The growth of medical imaging brings several challenges, including rising demand, workforce shortages, and escalating healthcare costs. As imaging becomes more integral to clinical pathways, departments must manage increased workloads while maintaining quality and timely reporting.
There are also ethical concerns. Over-reliance on imaging may lead to unnecessary tests or incidental findings, sometimes causing patient anxiety and prompting further unneeded investigations. Informed consent, appropriate referral practices, and clear communication are essential to ensure imaging is used judiciously and effectively.
Patient confidentiality and data protection are also critical, particularly with the increasing digitisation and sharing of imaging records. Systems must be robust enough to protect sensitive medical information while enabling efficient clinical access.
The Future of Medical Imaging
Medical imaging is expected to become even more personalised, predictive, and precise. Advances in molecular imaging, radiomics (the extraction of large amounts of data from medical images), and AI-guided diagnostics promise to transform patient care.
Teleradiology – the remote reporting of images – is also likely to expand, improving access to specialist expertise, particularly in rural or under-resourced regions. Cloud-based storage, mobile imaging units, and portable devices are further widening the reach of diagnostic services.
Moreover, with growing emphasis on value-based healthcare, imaging must demonstrate not just diagnostic accuracy but also its impact on patient outcomes, quality of life, and cost-effectiveness.
Conclusion
Medical imaging stands as one of the most transformative developments in healthcare, enabling earlier diagnosis, more accurate monitoring, and less invasive treatment. As technology continues to evolve, imaging professionals must adapt and innovate to meet the challenges of modern medicine.
Understanding how imaging works, when it is appropriate, and what it can offer is essential not just for clinicians but also for patients. With the right balance of innovation, safety, and clinical judgement, medical imaging will remain at the heart of effective healthcare delivery well into the future.
Disclaimer
This article is intended for general informational purposes only and does not constitute medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy of the information presented, Open Medscience makes no guarantees regarding its completeness or applicability to individual circumstances. Medical imaging procedures should always be discussed with a qualified healthcare professional who can provide personalised advice based on your medical history and clinical needs. The technologies and practices mentioned may vary by location, institution, or over time. Readers should not delay seeking medical advice or disregard professional guidance based on the content of this article.