Summary: Modern medicine relies heavily on advanced imaging technologies to diagnose, monitor, and treat a vast range of health conditions. Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET) are three major types of scanners that have revolutionised healthcare. Although these tools often appear similar to patients, each operates on a distinct principle, offers unique clinical advantages, and is suited to specific diagnostic scenarios. This article explores the core differences between CT, MRI, and PET scanners, examining their mechanisms, clinical uses, strengths, limitations, and how they contribute collectively to patient care.
Keywords: Medical Imaging, CT Scanner, MRI Scanner, PET Scanner, Diagnosis, Radiology
Introduction: The Role of Medical Imaging in Modern Healthcare
Medical imaging has transformed the way doctors understand and manage disease. Instead of relying solely on external examination or exploratory surgery, clinicians can now look inside the body with remarkable clarity and detail. Among the many imaging modalities, CT, MRI, and PET stand out for their versatility and diagnostic power. Each technology has evolved from decades of scientific innovation, and together, they underpin much of twenty-first-century diagnostic medicine.
Understanding the differences between these scanners is vital, not only for healthcare professionals but also for patients who may undergo these scans. This knowledge empowers individuals to make informed decisions about their health and demystifies what can often seem like a bewildering array of tests.
The CT Scanner: Fast and Detailed Imaging with X-Rays
Computed Tomography, or CT, was first introduced in the early 1970s and remains a cornerstone of radiological practice. The CT scanner uses X-rays, the same form of electromagnetic radiation as standard radiographs, but arranges them in a sophisticated way. The patient lies on a motorised table that moves through a doughnut-shaped ring, where an X-ray tube rotates around the body. Detectors capture the attenuated X-rays after they pass through tissues, and powerful computers reconstruct these data into detailed cross-sectional images.
One of the key features of CT is its speed. A scan of the entire body can be completed in a matter of minutes, which is particularly valuable in emergency situations, such as trauma or stroke. CT excels at visualising bone, soft tissues, and blood vessels with high spatial resolution. For example, it can detect fractures, haemorrhages, tumours, and infections with remarkable accuracy.
However, because CT relies on X-rays, there is exposure to ionising radiation, which carries a small but measurable risk, especially if repeated scans are needed. As a result, CT is generally used when the clinical benefit outweighs this risk, and alternative imaging is considered for younger patients or situations where radiation sensitivity is a concern.
Advancements such as multislice CT and dual-energy CT have further expanded its capabilities. Today, CT angiography can non-invasively assess blood vessels, and perfusion CT can evaluate blood flow to the brain or heart. The technique remains indispensable in cancer staging, preoperative planning, and acute care.
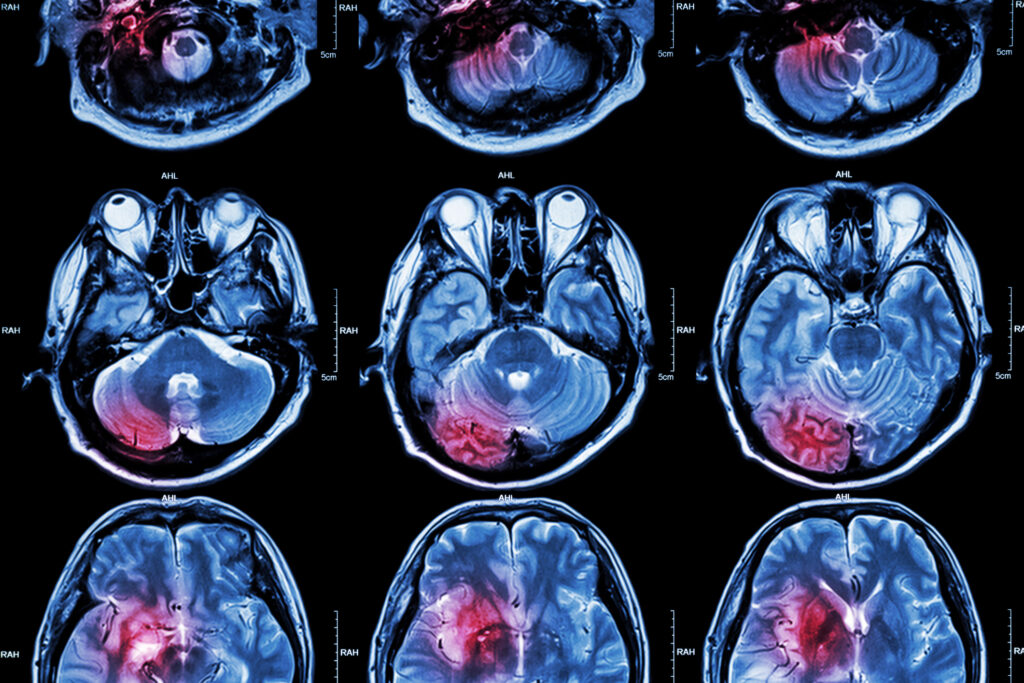
MRI: Harnessing Magnetism for Unparalleled Soft Tissue Contrast
Magnetic Resonance Imaging, or MRI, represents an entirely different approach to visualising the body. Instead of radiation, MRI uses powerful magnets, radiofrequency pulses, and sophisticated computing to create images. When a patient enters the scanner, the strong magnetic field causes hydrogen nuclei (mainly from water and fat) in the body to align. Brief radiofrequency pulses tip these nuclei out of alignment, and as they relax back, they emit signals detected by the scanner. By manipulating these signals with gradients and sequences, the MRI can produce highly detailed images of soft tissues.
The major strength of MRI lies in its ability to differentiate between various types of soft tissue. It is the imaging method of choice for the brain, spinal cord, joints, and soft tissue structures such as muscles and ligaments. MRI is invaluable in diagnosing neurological diseases like multiple sclerosis, identifying ligament tears, or characterising tumours.
Unlike CT, MRI does not use ionising radiation, making it preferable for children, pregnant women (in certain circumstances), and for follow-up imaging where repeated scans are necessary. Nevertheless, the strong magnetic field means that patients with certain implants (such as pacemakers or cochlear implants) may be unable to undergo an MRI. The process also tends to be longer than CT, sometimes requiring up to an hour, and can be noisy and uncomfortable for those with claustrophobia.
Recent developments include functional MRI (fMRI), which measures changes in blood flow to map brain activity, and diffusion tensor imaging (DTI), which traces nerve fibre pathways. These advances are not only invaluable for research but are also transforming the clinical management of neurological diseases.
PET Scanning: Imaging Cellular Activity and Metabolism
Positron Emission Tomography, or PET, offers a unique window into the body’s metabolic and biochemical activity. Rather than simply depicting anatomy, PET visualises physiological processes, such as glucose metabolism or receptor binding, at the molecular level.
A PET scan begins with the administration of a radiotracer, most commonly a form of glucose labelled with a short-lived radioactive isotope (such as fluorine-18). As cells in the body take up the tracer, positrons are emitted, which interact with electrons and produce gamma rays. These gamma rays are detected by the scanner and used to construct images that map the concentration and distribution of the tracer.
PET is best known for its use in oncology. Because many cancers consume glucose at a higher rate than normal tissues, PET can detect tumours, assess their spread, and monitor response to therapy. PET also plays an essential role in neurology (for example, in evaluating epilepsy or dementia) and cardiology (to assess viable heart muscle after a heart attack).
However, PET images are often less detailed in terms of structure compared to CT or MRI. For this reason, most modern PET scanners are combined with CT (PET/CT) or MRI (PET/MRI) in a single machine, allowing simultaneous acquisition of metabolic and anatomical information. This fusion of techniques enhances diagnostic accuracy and provides a more complete picture of disease.
The use of radioactive tracers does mean that there is exposure to radiation, although the doses are typically low and the tracers decay quickly. The preparation for a PET scan is also more involved, requiring careful timing and sometimes dietary restrictions to optimise the results.
Choosing the Right Scanner: Clinical Applications and Decision-Making
The clinical question, patient characteristics, and availability of equipment guide the decision to use CT, MRI, or PET. In trauma or acute settings, CT is often favoured because of its speed and its ability to detect life-threatening injuries rapidly. When soft tissue detail is crucial—such as for neurological, musculoskeletal, or pelvic imaging—MRI is often preferred.
PET, on the other hand, is primarily used for functional imaging, especially in cancer diagnosis, staging, and treatment monitoring. It is also valuable in selected cases of cardiac or neurological disease where information about tissue metabolism or receptor status can change management.
There are also situations where combining two or more modalities is essential. For instance, a patient with suspected cancer might undergo a CT scan to identify the location of a mass, followed by a PET to determine its metabolic activity, and then an MRI to map its relationship to critical soft tissues. The fusion of PET with CT or MRI is especially powerful, offering a blend of anatomical precision and metabolic insight that neither method alone could achieve.
It is worth noting that the choice of scanner is not always clear-cut, and the availability of expertise, scanner type, and even patient preference can influence the decision. Collaboration between radiologists, nuclear medicine physicians, and clinicians ensures that the right test is performed for the right patient at the right time.
Safety Considerations and Patient Experience
Each imaging modality has its own safety considerations. CT and PET both expose patients to ionising radiation, although modern scanners are designed to minimise doses while maintaining image quality. For most adults, the risk from a single scan is very low, but cumulative exposure over time should be kept as low as reasonably achievable.
MRI does not use radiation, but the powerful magnets require stringent safety protocols. Implants and metallic fragments can pose a hazard, and thorough screening is essential before entering the scanner. Additionally, the confined space and loud noise can be distressing for some patients, and sedation or open MRI scanners may be needed in selected cases.
Preparing for each scan varies. CT often requires minimal preparation, although contrast agents may be used to enhance certain structures. MRI may require fasting and the removal of all metal objects. PET involves dietary preparation and a waiting period after the injection of the tracer to allow it to accumulate in the target tissues.
Patient comfort and communication are vital. Radiographers and nuclear medicine technologists play a key role in explaining procedures, addressing concerns, and ensuring safety throughout the process. The experience of undergoing these scans is usually brief and painless, although it can cause anxiety, particularly in those unaccustomed to medical procedures.
The Future of Medical Imaging: Integration and Innovation
The fields of CT, MRI, and PET scanning are in constant evolution. Advances in artificial intelligence and machine learning are beginning to aid image interpretation, streamline workflow, and even predict disease progression. Hybrid scanners that combine multiple imaging modalities are becoming more common, providing comprehensive answers to complex clinical questions in a single session.
Personalised medicine is also influencing imaging. PET tracers can now be tailored to individual tumour types, revealing specific mutations or treatment targets. MRI techniques are being refined to offer quantitative data about tissue health, such as mapping the stiffness of organs or measuring blood flow without the need for contrast agents.
Portable and point-of-care imaging devices are on the horizon, bringing high-quality diagnostics to previously inaccessible settings. Research into reducing scan times, minimising side effects, and improving patient comfort continues to drive innovation.
Medical imaging remains a partnership between technology, clinical expertise, and patient-centred care. By understanding the unique strengths of CT, MRI, and PET, both doctors and patients can navigate the increasingly sophisticated world of diagnostics with confidence.
Harnessing the Power of Imaging for Better Health
CT, MRI, and PET scanners each offer distinct insights into the human body, drawing on the principles of physics, chemistry, and biology. Their differences lie not only in the technology used but also in the types of information they reveal and the clinical scenarios they address best.
CT is rapid and precise for structural imaging, especially in emergencies and for visualising bones and blood vessels. MRI excels in soft tissue contrast and is indispensable for neurological and musculoskeletal imaging without radiation exposure. PET opens a window onto cellular activity and metabolism, making it a vital tool in oncology and beyond.
Understanding these differences helps ensure that each patient receives the most appropriate, accurate, and safe diagnostic test. As technology advances, the boundary between these modalities continues to blur, promising ever more detailed and meaningful insights into health and disease. The future of medical imaging is bright, driven by ongoing innovation and a commitment to improving patient care.
Disclaimer
This article, “CT, MRI, and PET Scanners: Unravelling the Differences in Modern Medical Imaging”, is intended for general informational purposes only. It does not constitute medical advice, diagnosis, or recommendation for any specific procedure. The technologies and clinical practices discussed reflect current knowledge as of August 2025, but advancements and changes may occur over time. Patients should consult a qualified healthcare professional for personalised advice and to discuss the most appropriate imaging method for their individual circumstances. Open Medscience and the authors disclaim responsibility for any actions taken based on the information provided herein.
You are here: home » diagnostic medical imaging blog »