Summary: An innovative artificial intelligence (AI) model has demonstrated strong potential in accurately diagnosing prostate cancer, one of the most common cancers in men worldwide. Recent studies and clinical trials have shown that AI tools can assist radiologists and pathologists in detecting tumours earlier and more reliably, reducing human error and variability in diagnosis. By integrating machine learning with advanced imaging technologies, these systems can offer a faster and more consistent approach to diagnosing the disease, especially in ambiguous or early-stage cases. This article examines how AI is transforming prostate cancer diagnostics, the scientific basis of the model, its potential benefits, the remaining challenges, and what this advancement could mean for the future of men’s health.
Keywords: prostate cancer, artificial intelligence, diagnosis, machine learning, medical imaging, clinical trials
The Global Burden of Prostate Cancer
Prostate cancer is the second most frequently diagnosed cancer in men, with over 1.4 million new cases worldwide each year. The disease primarily affects older men, with risk increasing significantly after the age of 50. Early detection remains key to successful treatment, yet prostate cancer often develops silently in its early stages. Traditional methods of diagnosis, such as digital rectal examinations (DRE), prostate-specific antigen (PSA) blood tests, biopsies, and multiparametric MRI (mpMRI), are not always definitive. These tools rely heavily on human interpretation and clinical judgement, which can lead to underdiagnosis, overdiagnosis, or misdiagnosis.
Given these limitations, there has been growing interest in integrating artificial intelligence to aid diagnostic accuracy. AI algorithms, particularly those based on deep learning, can process vast datasets far faster than any clinician, identifying patterns and subtleties in imaging that the human eye might overlook.
The Role of AI in Medical Imaging
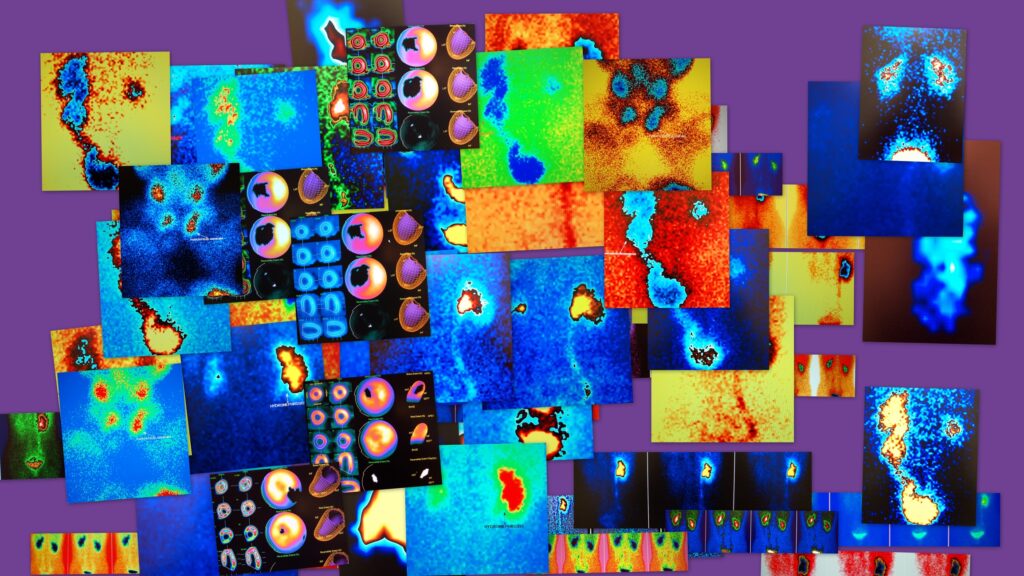
AI has been increasingly applied across various medical imaging domains, from detecting lung nodules in CT scans to identifying diabetic retinopathy in retinal images. In prostate cancer, AI is being trained to analyse mpMRI scans and digital histopathology slides. These models are fed thousands of annotated images, allowing them to learn the characteristics of malignant tissue.
Once trained, an AI system can rapidly evaluate a new image and provide a diagnosis with a high degree of confidence. Some models have demonstrated diagnostic accuracy on par with experienced radiologists and uropathologists. This has the potential to reduce diagnostic delays, support overworked clinical staff, and standardise assessments across institutions with differing levels of expertise.
In particular, a recent study led by researchers at a leading academic medical centre demonstrated that their AI model could accurately identify clinically significant prostate cancer in mpMRI scans. The tool not only flagged suspicious areas but also provided a malignancy score to help guide further investigation or biopsy.
Improved Accuracy and Reduced Variability
One of the most significant challenges in prostate cancer diagnosis is variability. Human interpretation of mpMRI is highly subjective, and inter-reader variability between radiologists is well-documented. Factors such as fatigue, experience, and institutional protocols can all affect outcomes. Even histopathological evaluation, considered the gold standard, can show significant variation between pathologists.
AI models are not subject to the same inconsistencies. Once validated and deployed, an AI tool performs the same task identically each time, making results more consistent and potentially more reproducible across healthcare systems. This does not mean AI should replace clinicians, but rather that it can serve as a second reader, alerting clinicians to findings they may have missed or helping to prioritise urgent cases.
There is also growing evidence that AI can detect subtle features invisible to the human eye, such as textural patterns in tissue density or early markers of tumour aggressiveness. These findings could refine diagnostic thresholds and help differentiate between aggressive cancers that require immediate treatment and indolent cases that may benefit from active surveillance.
Clinical Integration and Real-World Trials
For any AI tool to be implemented in clinical practice, it must undergo rigorous validation. This includes prospective trials that compare AI-supported diagnosis with standard practice. Several such trials are underway or have recently concluded, providing a growing body of evidence in support of these technologies.
One such study involved over 1,000 men undergoing prostate MRI scans at multiple institutions. The AI model was able to match or outperform radiologists in detecting clinically significant cancers while reducing false positives. Another trial focused on pathology slide analysis, with an AI system accurately grading tumours according to Gleason score, helping inform treatment decisions.
Integration into the clinical workflow is also crucial. The most successful models operate seamlessly within existing systems, such as PACS (Picture Archiving and Communication Systems) or electronic health records, providing real-time decision support without causing disruption. Training and education are also crucial, as clinicians need to understand how AI works, its limitations, and how to interpret its outputs in context.
Ethical, Legal and Practical Considerations
Although the benefits of AI in prostate cancer diagnosis are clear, several concerns remain. One is the risk of bias in training data. If an AI model is trained primarily on data from a specific population, it may perform poorly when applied to other populations. This raises concerns about health equity and access, particularly among underrepresented groups.
There are also legal questions about liability. If an AI system makes an error that leads to harm, who is responsible — the developer, the clinician, or the institution? These questions remain largely unresolved, and regulatory bodies are still determining how best to oversee the deployment of such systems in clinical care.
Data privacy is another concern. Training an AI model requires large volumes of patient data, which must be handled in accordance with strict data protection laws. Anonymisation, encryption, and clear consent procedures are vital in maintaining public trust.
Finally, clinicians must retain ultimate control. AI should support human decision-making, not replace it. A well-designed system will present its findings in an interpretable way, with confidence scores and visual outputs that allow clinicians to make informed decisions. The goal is to enhance, not supplant, medical expertise.
The Future of AI-Driven Prostate Cancer Diagnosis
The development of AI in prostate cancer diagnosis is progressing rapidly, with significant implications. As models improve and become more widely adopted, we may see earlier diagnoses, more accurate grading, and better targeting of biopsies and treatments. This could lead to improved survival rates, reduced overtreatment, and a better quality of life for patients.
In the future, AI might also be used to predict disease progression, assess treatment response, and personalise care. By integrating imaging data with genomic and clinical information, more comprehensive predictive models could be built, offering truly individualised medicine.
Moreover, AI could play a vital role in regions with limited access to specialist care. In settings where radiologists and pathologists are in short supply, AI tools could support local healthcare workers in providing high-quality diagnostics, helping close gaps in healthcare delivery.
Nonetheless, widespread adoption will depend on regulatory approval, clinician acceptance, and robust real-world validation. Collaboration between AI developers, healthcare professionals, and regulators will be essential in ensuring these tools are safe, effective, and equitable.
Conclusion
The use of artificial intelligence in prostate cancer diagnosis represents a promising development in the field of men’s health. By enhancing the accuracy, speed, and consistency of diagnostic assessments, AI has the potential to transform how prostate cancer is detected and managed. Although challenges remain — including regulatory, ethical, and technical hurdles — the early evidence is encouraging. Through continued research, validation, and thoughtful integration into clinical practice, AI has the potential to become a powerful tool in the fight against prostate cancer.
Disclaimer
The information provided in this article is for general informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment, and should not be relied upon as a substitute for professional medical guidance. Readers should consult a qualified healthcare professional regarding any medical condition or concerns, including the prevention, diagnosis, or treatment of prostate cancer. While every effort has been made to ensure the accuracy of the information at the time of publication, Open MedScience does not accept responsibility for any errors, omissions, or outcomes resulting from the use of this content. Any mention of specific technologies, products, studies, or organisations does not imply endorsement.