Proton therapy is a significant advancement in the field of oncology, offering a more targeted approach to radiation therapy. Unlike traditional radiation therapy, which uses X-rays, proton therapy uses protons to precisely target tumours, minimising damage to surrounding healthy tissues. This article explores the fundamentals of proton therapy, its benefits, the treatment process, its application across various cancer types, advancements in the technology, and comparisons with other treatments.
Introduction to Proton Therapy
Cancer treatment has undergone transformative changes over the decades, evolving from the broad application of surgery, chemotherapy, and traditional radiation therapy to more refined and targeted approaches. Among these advances, proton therapy stands out as a cutting-edge treatment, heralded for its precision and promise in reducing the unwanted side effects often associated with cancer care. This sophisticated form of radiation therapy uses protons—a type of charged particle—instead of the X-rays used in conventional radiation therapy to destroy cancer cells. Its emergence as a beacon of hope for many patients lies in its innovative approach and its significant benefits in terms of accuracy, efficacy, and quality of life for patients during and after treatment.
The advantage of proton therapy comes from the fundamental properties of protons themselves. Unlike X-rays, which release energy along their entire path through the body, protons deposit most of their energy directly at the tumour site before coming to a stop. This precise targeting is made possible by controlling the energy of the protons, allowing them to reach a specific depth in the tissues. This characteristic minimises the dose delivered to the surrounding healthy tissues and vital organs, a concept known as the Bragg peak. The ability to concentrate high doses of radiation directly on the tumour while sparing the surrounding healthy tissue is a paradigm shift in radiation therapy, offering hope for improved outcomes and fewer side effects.
The significance of proton therapy extends beyond its technical capabilities. It represents a more personalised approach to cancer treatment, where therapies are tailored to the unique characteristics of the patient’s tumour and anatomical structure. This is particularly crucial for cancers located in or near critical structures, where traditional radiation therapy’s lack of precision could lead to damaging side effects. The precision of proton therapy is especially beneficial for paediatric patients, whose developing bodies are more susceptible to the harmful effects of radiation. By reducing exposure to radiation, proton therapy minimises the risk of growth and developmental problems, secondary cancers, and other long-term health issues.
Moreover, the evolution of this therapy technology underscores the rapid pace of innovation in cancer treatment. Advances in treatment planning systems, imaging technologies, and proton beam delivery methods, such as pencil beam scanning, have enhanced the precision and efficiency of proton therapy even further. These technological advancements have expanded the range of cancers that can be treated with proton therapy, including but not limited to brain cancers, spinal tumours, head and neck cancers, lung cancers, prostate cancers, and certain paediatric cancers.
However, the journey of proton therapy from a novel idea to a mainstream treatment option has not been without challenges. Issues such as the high cost of building and operating proton therapy centres and the need for more extensive clinical trials to compare its effectiveness against traditional therapies have been points of debate within the medical community. Despite these challenges, the growing body of evidence supporting its benefits, coupled with advancements in technology that reduce costs and increase accessibility, is making proton therapy an increasingly viable option for a broader range of patients.
Proton therapy embodies the future of cancer treatment. In the future, therapies will be effective and designed with the utmost consideration for the patient’s overall well-being and quality of life. As we probe deeper into the nuances of proton therapy, it becomes clear why it is regarded as a game-changer in the area of cancer care. Its development and refinement over the years symbolise the relentless pursuit of better, more humane ways to battle cancer, offering hope and a new lease on life to many who face this daunting diagnosis.
Understanding Proton Therapy Towards Treatment Planning
Proton therapy is a significant advancement in the field of radiation oncology, offering a highly targeted approach to the treatment of various cancers. Unlike conventional radiation therapy that uses X-rays, proton therapy employs protons—positively charged particles—to deliver radiation directly to the tumour. This method harnesses the unique physical properties of protons, allowing for unparalleled precision in cancer treatment. This precision significantly reduces the exposure of healthy tissues to radiation, potentially resulting in fewer side effects and enhancing patients’ quality of life during and after treatment.
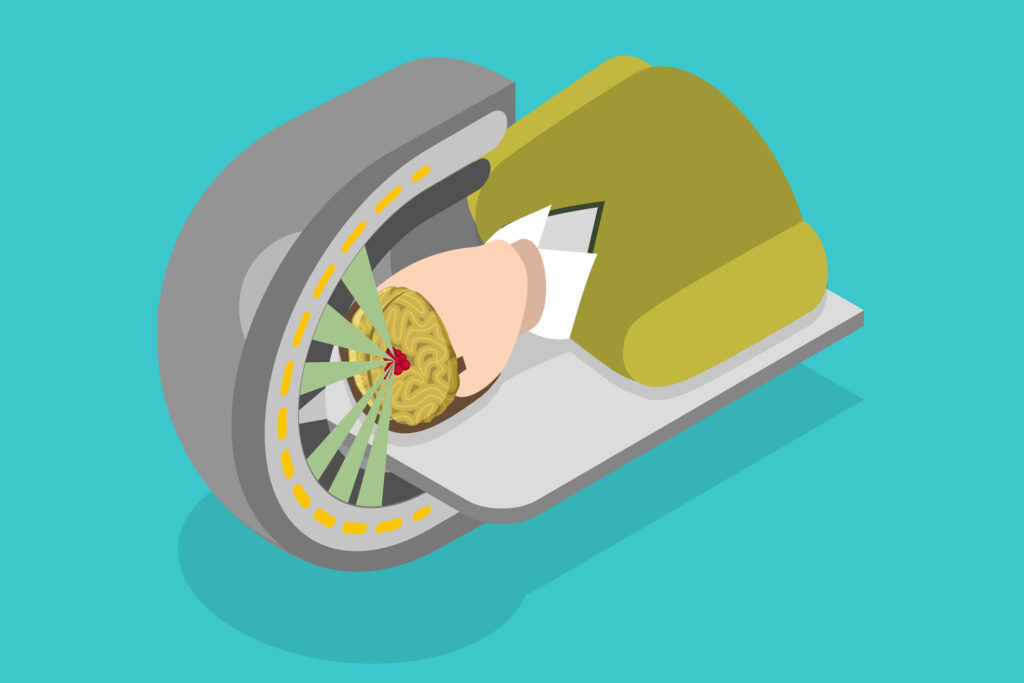
The core principle of proton therapy lies in the distinctive way protons release energy. As protons travel through the body, they deposit a low dose of radiation along their path until they reach a specific, pre-determined depth—the location of the tumour. At this point, they release the bulk of their energy in a sharp burst, known as the Bragg peak. The ability to manipulate the energy of protons so that the Bragg peak corresponds precisely to the tumour site is what sets proton therapy apart. This precise control means that the tumour can receive the high doses of radiation needed to destroy cancer cells while sparing the surrounding healthy tissues and organs. This level of precision is particularly advantageous for treating tumours located in or near vital organs and for pediatric patients, whose developing bodies are more susceptible to the adverse effects of radiation.
The delivery of proton therapy involves sophisticated technology and careful planning. Before treatment begins, a multidisciplinary team, including radiation oncologists, medical physicists, and dosimetrists, collaborate to create a highly individualised treatment plan. This process involves detailed imaging studies, such as MRI and CT scans, to determine the tumour’s exact size, shape, and location. Advanced computer software then calculates the optimal dose distribution and the precise angles for the proton beams. This precise preparation ensures that the treatment is tailored to the specific characteristics of each patient’s cancer.
Proton therapy sessions typically take place on an outpatient basis, with each session lasting only a few minutes. However, the total number of sessions can vary depending on the type and stage of cancer being treated. Regardless of the brevity of each session, the treatment process usually spans several weeks to ensure the delivery of the full therapeutic dose of radiation to the tumour.
One of the key advantages of proton therapy is its reduced incidence of side effects compared to traditional radiation therapy. By reducing damage to healthy tissues, patients undergoing proton therapy are less likely to experience the unwanted side effects associated with radiation, such as fatigue, skin irritation, and damage to surrounding organs. This can be particularly important for cancers in sensitive areas, where traditional radiation therapy might risk causing significant harm, such as in brain, spinal, head and neck, lung, and paediatric cancers.
Proton therapy is a cutting-edge cancer treatment modality that offers targeted, precise radiation delivery with the potential for fewer side effects. Its ability to spare healthy tissues while effectively treating tumours makes it a valuable option for many cancer patients, particularly those with complex or sensitive tumour locations. As research continues and technology advances, the availability and applications of proton therapy are expected to expand, further solidifying its role in modern oncology.
The Benefits of Proton Therapy
Proton therapy, a state-of-the-art form of cancer treatment, has been increasingly recognised for its potential to reduce the side effects typically associated with traditional radiation therapy. This innovative approach leverages the unique properties of protons—positively charged particles—to target cancer cells with remarkable precision, thereby minimising the radiation dose that surrounding healthy tissues receive. The significance of this targeted approach cannot be overstated, particularly when it comes to improving patients’ quality of life during and after treatment.
Traditional radiation therapy, which uses X-rays, cannot discriminate as effectively between cancerous and healthy tissues. X-rays continue to deposit energy beyond the tumour, affecting healthy tissues and organs in their path. This can lead to a range of side effects, from fatigue and skin irritation to more severe, long-term complications such as organ damage or secondary cancers. In contrast, proton therapy’s ability to precisely target tumours reduces the risk of these side effects. The protons deliver their maximum energy directly to the tumour site through a phenomenon known as the Bragg peak, beyond which no further radiation is emitted. This precision significantly spares the surrounding healthy tissues, leading to fewer immediate and long-term side effects.
The reduced side effects of proton therapy are particularly beneficial for patients undergoing treatment for tumours in sensitive or hard-to-reach areas. Cancers of the brain, spine, and those located near vital organs are notoriously difficult to treat with traditional radiation therapy without causing significant collateral damage. Proton therapy’s targeted approach allows for high doses of radiation to be safely delivered to such tumours, maximising the chance of successful treatment while preserving the function and integrity of the surrounding healthy tissues and organs.
For example, proton therapy offers a critical advantage in treating pediatric cancers, where the potential for long-term side effects is a significant concern due to the sensitivity of developing tissues and organs. Reduced radiation exposure lowers the risk of growth abnormalities, hormonal deficiencies, and the development of secondary cancers, issues that are particularly pertinent in the treatment of young patients.
Moreover, the effectiveness of proton therapy in treating complex tumours translates into a reduction in side effects and potentially improved survival rates and quality of life. Patients treated with proton therapy often report a quicker recovery time and a faster return to their daily activities, underscoring the treatment’s impact on preserving quality of life.
Despite its advantages, it’s important to note that proton therapy is not without its challenges, including accessibility and cost. However, as the technology becomes more widespread and insurance coverage for the treatment expands, it’s expected that more patients will be able to benefit from this advanced treatment option.
The reduced side effects of proton therapy represent a significant advancement in cancer treatment. By minimising the impact on healthy tissues, proton therapy offers a more patient-friendly approach to radiation therapy, particularly for those with tumours in sensitive areas or for whom preserving the quality of life is a paramount concern. As research continues and technology evolves, the role of proton therapy in reducing treatment-related side effects and improving patient outcomes is likely to grow, marking a new era in the fight against cancer.
Proton Therapy Treatment Planning Process
The pathway to proton therapy, a revolutionary cancer treatment, commences with an initial consultation—a critical first step in determining the appropriateness of this advanced technique for each individual patient. This consultation is more than just a preliminary meeting; it represents a comprehensive evaluation wherein a multidisciplinary team of specialists, including oncologists, radiologists, and physicists, collaboratively assess the patient’s medical condition, tumour characteristics, and overall suitability for proton therapy. This careful deliberation ensures that proton therapy, with its unique benefits and considerations, is tailored to those who stand to gain the most from its precision and reduced side effect profile.
The patient’s medical history, previous treatments, and current health status are thoroughly reviewed during the initial consultation. Advanced diagnostic tests, such as MRI and CT scans, may be utilised to provide a detailed understanding of the tumour’s size, shape, and location. This holistic approach not only aids in determining the feasibility of proton therapy but also fosters an open dialogue between the patient and the medical team, providing a platform for addressing concerns, discussing potential benefits and limitations, and setting realistic expectations for the treatment outcome.
Following the decision to proceed with proton therapy, the next crucial phase is treatment planning. This stage involves sophisticated imaging techniques that map out the exact contours of the tumour with remarkable accuracy. The goal is to create a highly customised treatment plan that maximises the effectiveness of the proton beam, directing it precisely to the tumour while sparing the surrounding healthy tissues as much as possible. Software algorithms calculate the optimal dose distribution, taking into account the tumour’s three-dimensional shape and the specific characteristics of proton beam physics. This meticulous planning process, which may take several days to weeks, is vital for achieving the precision that sets proton therapy apart from conventional radiation treatments.
With the treatment plan in place, the patient embarks on the series of treatment sessions that form the core of their proton therapy experience. Typically, these sessions occur five days a week over several weeks, depending on the specific cancer type, its stage, and the goals of treatment. Each session is relatively quick and painless, lasting about 30 minutes, with the actual time spent delivering the proton beams amounting to only a few minutes. Patients are positioned with the aid of custom-made devices designed to ensure they remain still and in the correct posture throughout the treatment. The non-invasiveness and precision of proton therapy mean that patients can usually resume their normal activities immediately after each session, with minimal disruption to their daily lives.
This structured approach—from the initial consultation through treatment planning to the completion of the treatment sessions—embodies the patient-centred ethos of proton therapy. It highlights the technical sophistication of the treatment and the commitment to providing personalised care that addresses each patient’s specific needs and concerns. As proton therapy continues to evolve and become more accessible, its integration into comprehensive cancer care underscores the ongoing advancements in the quest to treat cancer more effectively and enhance the quality of life for patients during and after treatment.
Applications of Proton Therapy
Proton therapy has been a significant breakthrough in the treatment of a wide range of cancers, offering new hope to patients across various demographics. Its success spans several types of cancer, including prostate, breast, lung, and, notably, paediatric cancers, where its precision and reduced collateral damage are of paramount importance. The unique advantage of proton therapy lies in its ability to deliver targeted radiation to the tumour with minimal exposure to the surrounding healthy tissues. This characteristic is particularly crucial when treating children whose bodies are still growing and are more susceptible to the harmful effects of radiation.
The ability of proton therapy to minimise damage to growing tissues reduces the risk of developmental issues and secondary cancers later in life, a common concern with traditional radiation therapy. For paediatric patients, this means a better chance at a cure and a significantly improved quality of life post-treatment. The tailored approach of proton therapy, focusing radiation precisely where it’s needed, ensures that children can continue to grow and develop with fewer long-term health complications. As such, proton therapy represents a significant advancement in oncological care, offering a safer, more effective treatment option for cancer patients, especially the youngest among them.
Advancements in Proton Therapy Technology
Recent technological advancements in the sphere of proton therapy have significantly enhanced its accessibility and efficiency, marking a new era in the treatment of cancer. Among these innovations, pencil beam scanning stands out for its remarkable precision in targeting tumours. This advanced technique allows for the modulation of the proton beam’s intensity and direction, enabling it to conform more closely to the complex shapes of tumours. The result is an even greater sparing of healthy tissues surrounding the tumour, thereby reducing the potential for side effects and improving patient outcomes.
Further, imaging and computer technology developments have revolutionised treatment planning and delivery in proton therapy. The use of cutting-edge imaging techniques, such as Positron Emission Tomography (PET) and Magnetic Resonance Imaging (MRI), provide detailed and accurate visualisations of tumours, facilitating more precise treatment planning. Additionally, sophisticated computer algorithms now enable the customisation of proton therapy for each patient, optimising the dose distribution based on the tumour’s and surrounding tissues’ unique characteristics. These technological advancements improve the precision and effectiveness of proton therapy and streamline the treatment process, making proton therapy a more accessible option for a broader range of patients.
Comparing Proton Therapy to Other Treatments
Proton therapy, despite its remarkable benefits, is not a one-size-fits-all solution for every cancer diagnosis. Its application and effectiveness are contingent upon specific factors, including the type, location, and stage of cancer. However, for certain cancers, the advantages of proton therapy over traditional radiation therapy and surgery are significant, underscoring the need for a personalised approach to cancer treatment. Conventional radiation therapy, though effective, often involves a compromise between destroying cancer cells and preserving healthy tissues. With its precision, Proton therapy minimises this compromise, offering a targeted treatment that reduces damage to surrounding healthy tissues and lowers the risk of side effects.
Similarly, surgery, while curative for many cancers, carries risks associated with anaesthesia, infection, and long recovery times. For tumours located near critical structures or in parts of the body where surgery poses high risks, proton therapy provides a non-invasive alternative that can achieve comparable outcomes without the physical trauma of surgery. These distinctions highlight the importance of evaluating each cancer case individually, allowing for a treatment modality that is best suited to the patient’s specific condition and needs, thereby optimising the effectiveness of treatment while aiming to preserve the quality of life.
The Future of Proton Therapy
The landscape of proton therapy is undergoing a significant transformation, driven by relentless research and technological innovation. This cutting-edge form of cancer treatment is on a trajectory of rapid evolution, with scientists and medical professionals working tirelessly to broaden its applicability and enhance patient outcomes. As the technology underpinning proton therapy becomes more sophisticated and accessible, the potential for its integration into standard cancer care protocols grows, promising to redefine the paradigms of oncological treatment.
Current research endeavours are focused on refining the precision and efficiency of proton therapy and exploring its potential benefits across a broader spectrum of cancers. Studies are underway to understand the biological effects of proton therapy at a cellular level, aiming to uncover the mechanisms that might make certain cancers more responsive to proton beams. This research is critical in identifying new cancer types that could benefit from proton therapy, potentially extending its use beyond the current indications.
Moreover, technological advancements, such as the development of more compact and cost-effective proton therapy systems, are addressing one of the primary barriers to its widespread adoption—cost and accessibility. These innovations will make proton therapy a more feasible option for many healthcare facilities, thereby increasing the number of patients who can access this treatment.
The integration of artificial intelligence and machine learning into treatment planning is another frontier being explored, with the potential to significantly improve the precision of proton therapy and personalise treatment plans to an unprecedented degree. This could lead to more effective treatments with even fewer side effects, further improving patient outcomes.
As proton therapy continues to evolve, its role in cancer treatment is set to become more prominent. With ongoing research and technological advancements, the future of proton therapy is bright, offering hope for more effective, targeted, and patient-friendly cancer treatments. This progress underscores the dynamic nature of the oncology field, where innovation continually drives the improvement of patient care and outcomes.
Conclusion
Proton therapy marks a transformative advancement in the field of cancer treatment, setting a new benchmark in precision, efficacy, and patient well-being. Unlike traditional therapies, which often struggle to balance the effective eradication of cancer cells with the preservation of healthy tissue, proton therapy achieves this equilibrium with unparalleled accuracy. Its ability to deliver high doses of radiation directly to the tumour while sparing surrounding healthy tissues minimises the side effects commonly associated with cancer treatment, thereby enhancing the quality of life for patients both during and after treatment.
As ongoing research sheds more light on the mechanisms and potential of proton therapy and technological innovations, make it more accessible, its significance within oncology is poised for exponential growth. This progress opens new avenues for treating various types of cancer and reinforces the shift towards more personalised and patient-centred care models. Proton therapy, with its emphasis on minimising harm, while maximising treatment effectiveness, is at the forefront of this shift, offering a glimpse into a future where cancer treatment is not only about survival but also about preserving the quality of life. For patients grappling with the daunting realities of cancer, proton therapy represents a beacon of hope, embodying the next frontier in customised, compassionate cancer care in treatment planning.
Disclaimer
The information presented in this article is intended for general educational and informational purposes only and should not be construed as medical advice or a substitute for professional healthcare guidance. While every effort has been made to ensure the accuracy and reliability of the content, Open Medscience makes no representations or warranties of any kind, express or implied, about the completeness, accuracy, or suitability of the information contained herein.
Proton therapy, like all cancer treatments, involves complex decision-making tailored to the individual patient’s diagnosis, medical history, and overall health. The benefits and risks of such treatments must be carefully considered in consultation with qualified healthcare professionals. This article does not replace or constitute a medical consultation, diagnosis, or treatment recommendation.
Any reliance you place on the information provided in this article is strictly at your own risk. Open Medscience, its authors, and affiliates are not liable for any direct or indirect damages or consequences arising from the use or interpretation of this information.
Readers are strongly advised to consult with their oncologist, radiologist, or other appropriately licensed medical professionals for personalised advice and before making any decisions related to cancer treatment.
You are here: home » diagnostic medical imaging blog »