Summary: Simulation and imaging technologies have significantly advanced radiation therapy planning, enhancing the accuracy and efficacy of cancer treatment. Modern techniques such as computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), and advanced computational simulations have improved tumour delineation, patient positioning, and dose optimisation. This article examines the methods, challenges, and future prospects of imaging and simulation in radiation therapy planning, highlighting how technological advancements are enhancing clinical outcomes.
Keywords: Radiation Therapy; Imaging Techniques; Simulation; Treatment Planning; Computed Tomography; Dose Optimisation.
The Role of Simulation in Radiation Therapy Planning
Radiation therapy remains a cornerstone of cancer treatment, aiming to eradicate malignant cells while preserving healthy tissue. Critical to the success of radiation therapy is precise treatment planning, which involves careful patient simulation and sophisticated imaging modalities. Historically, treatment planning was limited by basic imaging techniques and manual calculations. Modern developments have greatly improved precision and effectiveness through enhanced visualisation, detailed anatomical information, and precise dose delivery.
Historical Context and Advances
Historically, radiation therapy simulation was primarily accomplished using fluoroscopic imaging, with manual adjustments made by clinicians. These simulations lacked precision, potentially leading to inaccurate radiation delivery and increased risk to healthy tissues. Modern simulation techniques integrate digital imaging and advanced computing technologies, facilitating accurate patient positioning, precise targeting, and improved outcomes.
Virtual Simulation and Patient Positioning
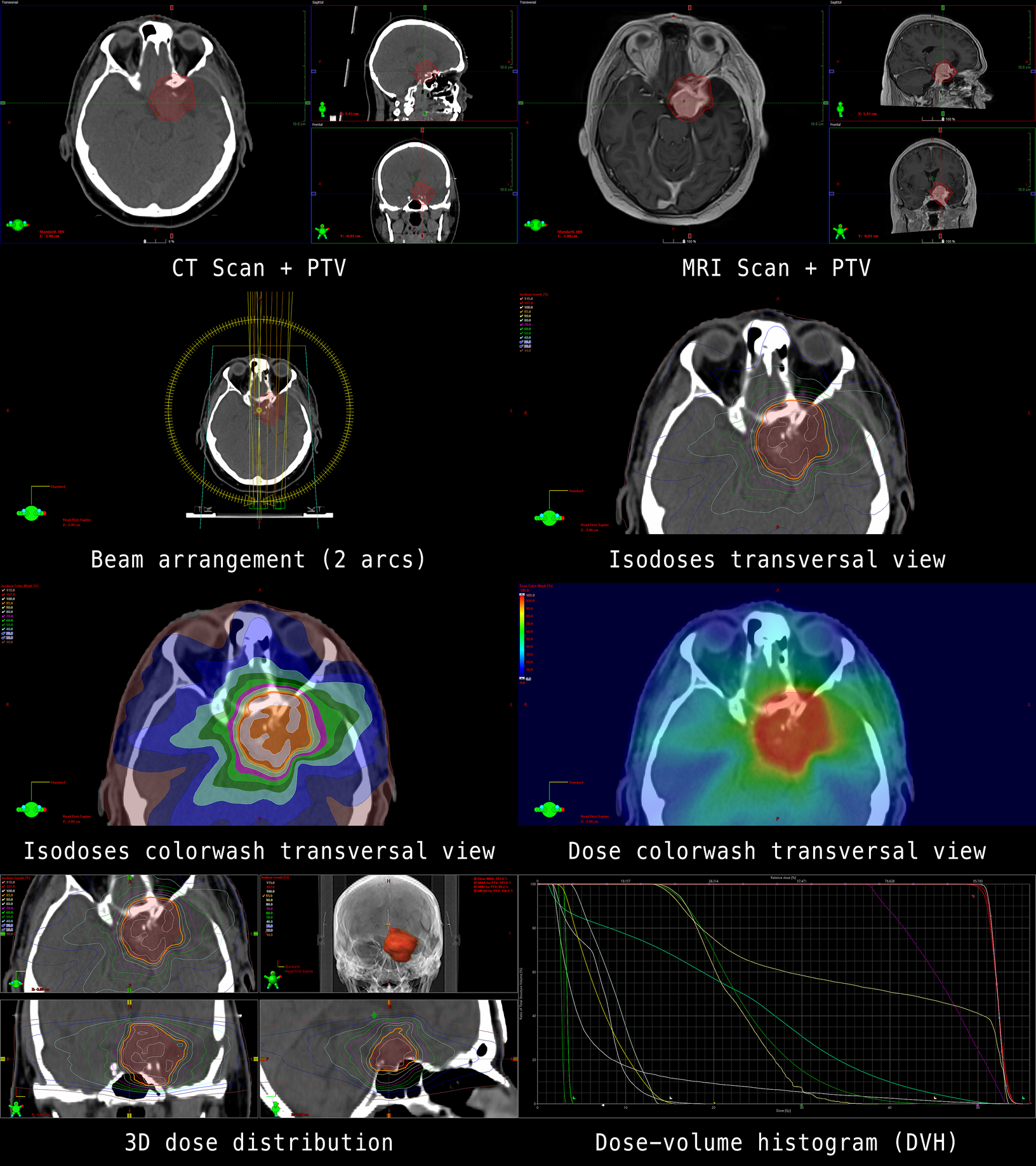
Virtual simulation combines CT imaging with advanced software, enabling clinicians to visualise and manipulate patient anatomy digitally. This virtual environment enables precise planning of radiation fields without requiring repeated physical patient repositioning. Ensuring accurate patient positioning minimises the potential for misalignment during treatment, reducing side effects and improving therapeutic efficacy.
Imaging Techniques in Radiation Therapy Planning
Computed tomography is currently the most extensively used imaging modality in radiation therapy planning. It provides detailed anatomical information, facilitating precise localisation and delineation of tumours and surrounding structures. CT images provide high-resolution, three-dimensional data that enable clinicians to accurately calculate radiation dose distributions, thereby optimising patient safety and treatment effectiveness.
However, CT has limitations, including poor soft-tissue contrast compared to other modalities such as MRI. As a result, integration with complementary imaging techniques has become standard practice.
Magnetic Resonance Imaging (MRI)
MRI offers superior soft-tissue contrast, particularly beneficial in delineating tumours within soft tissues, such as the brain, spinal cord, and pelvis. MRI’s ability to distinguish between healthy and diseased tissues enables better targeting of radiation doses, improving therapeutic precision and reducing collateral damage.
Increasingly, MRI is being integrated directly into radiation therapy planning processes, including MRI-guided radiation therapy systems. These technologies allow for real-time imaging during treatment delivery, ensuring precise alignment throughout the therapy course.
Positron Emission Tomography (PET)
PET imaging enhances radiation therapy planning through metabolic and functional information about tumours. By detecting radiotracer uptake, PET helps clinicians differentiate active tumour cells from non-viable tissue or necrosis. PET-CT fusion imaging has become particularly significant, as it combines anatomical and functional data to deliver targeted therapy with precision.
PET imaging has notably improved the planning of radiation therapy for cancers such as lymphoma, lung cancer, and head and neck cancers, where precise targeting significantly impacts outcomes.
Computational Simulations and Dose Optimisation
The fundamental goal of radiation therapy is maximising tumour eradication while minimising damage to healthy tissues. Dose optimisation involves complex computational algorithms that calculate precise radiation distribution, ensuring optimal therapeutic efficacy.
Monte Carlo Simulations
Monte Carlo simulations provide advanced computational methods for radiation dose calculations, significantly enhancing accuracy compared to conventional methods. By simulating millions of radiation interactions within patient-specific anatomy, Monte Carlo methods precisely predict dose distribution, enabling meticulous planning tailored to individual patients.
Although computationally demanding, advancements in processing power and algorithm efficiency have made Monte Carlo simulations increasingly feasible in clinical practice.
Intensity-Modulated Radiation Therapy (IMRT)
IMRT uses advanced computational simulations to optimise radiation dose distribution precisely. IMRT enables clinicians to modulate radiation intensity across multiple beams, ensuring maximum dose delivery to tumour sites while sparing adjacent healthy tissue. This method significantly improves treatment outcomes and reduces the risk of radiation-induced side effects.
Challenges in Simulation and Imaging for Radiation Therapy Planning
One major challenge in radiation therapy planning is integrating data from multiple imaging modalities, such as CT, MRI, and PET. Accurate image registration is crucial for aligning images from different modalities, thereby providing comprehensive anatomical and functional views. Errors in registration can lead to inaccuracies in tumour delineation and dose calculation, undermining treatment effectiveness.
Patient Movement and Organ Motion
Managing patient movement and internal organ motion during simulation and treatment presents a continuous challenge. Respiratory and digestive movements can significantly affect radiation targeting accuracy. Techniques such as respiratory gating and motion-tracking technologies have been developed to counteract these effects, though challenges persist, particularly with tumours in the thorax and abdomen.
Future Directions and Innovations
Adaptive radiation therapy represents an evolving approach that involves continually adapting treatment based on changes in patient anatomy and tumour dynamics. By frequently updating simulation and imaging during therapy, ART enables ongoing refinement of dose delivery, enhancing efficacy and safety.
Artificial Intelligence (AI) and Machine Learning
Artificial intelligence and machine learning are increasingly contributing to radiation therapy planning. AI-based systems can automate and optimise image segmentation, dose calculations, and treatment adjustments, significantly enhancing precision and efficiency. Additionally, AI-driven predictive models can anticipate tumour response, allowing clinicians to proactively adjust therapeutic approaches.
Proton Therapy and Advanced Particle Therapy
Advances in proton and particle therapy offer considerable promise for precise radiation therapy delivery. Proton beams have a distinct physical characteristic called the Bragg peak, which deposits maximum energy at the tumour site while sparing surrounding tissues. Enhanced simulation and imaging techniques are essential to fully exploit the benefits of proton therapy, further pushing the boundaries of therapeutic precision.
Conclusion
Simulation and imaging techniques have revolutionised radiation therapy planning, driving unprecedented precision and efficacy. Computed tomography, magnetic resonance imaging, and positron emission tomography provide essential anatomical and functional data, while computational simulations such as Monte Carlo methods optimise dose calculations. Despite challenges related to integration and motion management, innovations in adaptive therapy, artificial intelligence, and proton therapy continue to propel the field forward. As these advancements become widely implemented, they promise enhanced outcomes, improved patient safety, and greater therapeutic success.
In the future, continued investment and research in simulation and imaging technologies will be instrumental in transforming radiation therapy into an even more precise, personalised, and effective treatment modality.
Disclaimer
The information presented in “Advancements in Simulation and Imaging for Precision Radiation Therapy Planning” by Open Medscience is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Healthcare professionals should be consulted for personal medical concerns or treatment decisions. While every effort has been made to ensure the accuracy and currency of the information provided, Open Medscience makes no representations or warranties regarding its completeness, reliability, or applicability in clinical settings. The views expressed in this article are those of the authors and do not necessarily reflect those of any affiliated institutions or organisations.