Medical imaging technology has revolutionised the way healthcare professionals understand, diagnose, and treat a wide array of conditions within the human body. From the early days of X-rays to cutting-edge technologies such as functional MRI (fMRI) and 3D ultrasounds, medical imaging has become an indispensable tool in modern medicine. This article looks into the history, various modalities, and the future of medical imaging, illustrating how these technologies continue to shape our understanding of human health.
The Evolution of Medical Imaging Technology
The history of medical imaging is a tale of remarkable innovation and relentless curiosity. Before the advent of imaging technologies, medical professionals relied solely on physical examinations and exploratory surgery to diagnose internal ailments. The turning point came in 1895 when Wilhelm Conrad Röntgen discovered X-rays, forever altering the trajectory of medicine.
X-ray: The First Glimpse Inside the Body
Röntgen’s accidental discovery of X-rays opened the door to non-invasive internal imaging. X-ray imaging is based on the principle of differential absorption, where dense materials such as bones absorb more radiation than soft tissues, producing distinct images. The ability to visualise bones and detect fractures without surgery was revolutionary and laid the foundation for the development of other imaging technologies.
The Rise of Computed Tomography (CT)
By the 1970s, Computed Tomography (CT) emerged, offering far more detailed images than traditional X-rays. CT scans take multiple X-ray images from different angles and use computer processing to create cross-sectional images, or “slices,” of bones, blood vessels, and soft tissues. This ability to produce 3D images has made CT scans invaluable in diagnosing cancers, heart diseases, and internal injuries.
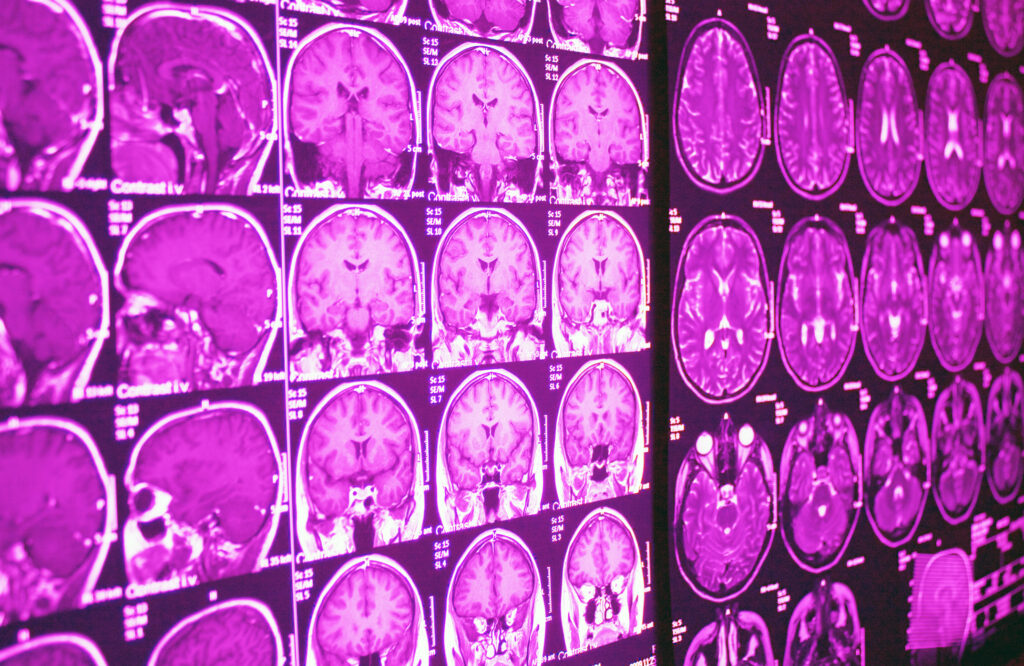
Magnetic Resonance Imaging (MRI): A Game-Changer in Soft Tissue Imaging
While X-rays and CT scans are excellent at imaging bones and certain dense tissues, they fall short when it comes to visualising soft tissues such as the brain, muscles, and organs. This gap was filled by Magnetic Resonance Imaging (MRI), which uses strong magnetic fields and radio waves to create detailed images of soft tissues.
How MRI Works
Unlike X-rays, MRI does not use ionising radiation. Instead, it relies on the interaction between magnetic fields and hydrogen atoms in the body. When exposed to a magnetic field, hydrogen atoms in the body align in a certain direction. Radiofrequency pulses are then applied, causing these atoms to spin out of alignment. As they return to their original position, they emit signals that are detected and converted into images by a computer.
Applications of MRI
MRI has become the gold standard for imaging soft tissues, especially the brain and spinal cord. It is widely used to diagnose neurological conditions such as multiple sclerosis, brain tumours, and stroke. MRI is also highly effective in assessing joint disorders, muscle injuries, and detecting tumours in organs like the liver and kidneys.
Functional MRI (fMRI)
One of the most fascinating advancements in MRI technology is functional MRI (fMRI), which measures brain activity by detecting changes in blood flow. As neurons in the brain become active, they require more oxygen, leading to increased blood flow in those areas. fMRI detects these changes and creates maps of brain activity, allowing researchers and clinicians to study brain functions related to movement, perception, and cognitive processes.
Ultrasound: Safe and Real-Time Imaging
Ultrasound imaging, also known as sonography, has a unique place in medical imaging as it does not rely on ionising radiation. Instead, it uses high-frequency sound waves to create images of structures within the body. Ultrasound is particularly known for its use in obstetrics to monitor foetal development, but its applications extend far beyond that.
How Ultrasound Works
An ultrasound probe emits sound waves, which travel through the body and bounce back when they encounter different tissues. These returning echoes are captured by the probe and used to create an image. The ability to produce real-time images makes ultrasound an invaluable tool for guiding certain procedures, such as needle biopsies or catheter placements.
Applications of Ultrasound
Aside from its well-known use in pregnancy, ultrasound is widely used to examine the heart, blood vessels, and abdominal organs. Doppler ultrasound, a specialised form of the technology, is used to assess blood flow and detect blockages in arteries or veins, making it essential in diagnosing cardiovascular diseases.
3D and 4D Ultrasound
Recent advancements in ultrasound technology have led to the development of 3D and 4D ultrasounds, providing more detailed and dynamic images. While 2D ultrasound images are essentially flat, 3D ultrasounds create a three-dimensional image, offering a clearer picture of structures. 4D ultrasound takes it a step further by adding the element of time, creating live, moving images that can be particularly helpful in monitoring the development of a foetus or assessing the motion of organs.
Positron Emission Tomography (PET): Imaging Metabolic Activity
While most imaging techniques focus on visualising anatomical structures, Positron Emission Tomography (PET) provides insights into the metabolic activity of tissues. PET is a type of nuclear medicine imaging that uses small amounts of radioactive materials, known as tracers, to detect abnormal metabolic processes.
How PET Works
In a PET scan, a patient is injected with a radioactive tracer, typically a form of glucose. Because cancer cells and other abnormal tissues tend to have higher metabolic rates than normal cells, they absorb more of the tracer. As the tracer decays, it emits positrons, which collide with electrons and produce gamma rays. These gamma rays are detected by a scanner and used to create images that highlight areas of abnormal metabolic activity.
Applications of PET
PET scans are widely used in oncology to detect and monitor the spread of cancer. They are also valuable in cardiology for assessing heart function and identifying areas of reduced blood flow. In neurology, PET scans help diagnose conditions like Alzheimer’s disease by revealing areas of the brain with abnormal metabolic activity.
Advances in Medical Imaging Technologies
While the core imaging modalities like X-ray, CT, MRI, and ultrasound remain essential, the field of medical imaging is continually evolving. Advances in imaging techniques, artificial intelligence, and hybrid imaging systems are pushing the boundaries of what is possible.
Artificial Intelligence and Machine Learning in Medical Imaging
Artificial intelligence (AI) and machine learning are transforming medical imaging by improving the speed and accuracy of image analysis. AI algorithms can be trained to detect patterns in imaging data that may not be visible to the human eye. These algorithms can assist radiologists in diagnosing conditions, prioritising urgent cases, and reducing the rate of false positives and negatives.
Hybrid Imaging: PET-CT and PET-MRI
Hybrid imaging systems, such as PET-CT and PET-MRI, combine the strengths of different imaging modalities to provide more comprehensive diagnostic information. PET-CT combines the metabolic insights of PET with the anatomical detail of CT, while PET-MRI offers high-resolution images of soft tissues alongside metabolic data. These systems are particularly valuable in cancer diagnosis and treatment planning.
Optical Imaging and Fluorescence-Guided Surgery
Another exciting area of development is optical imaging, which uses light to visualise tissues and cells. Optical imaging is especially promising in the field of fluorescence-guided surgery, where fluorescent dyes are used to highlight tumours, making it easier for surgeons to remove cancerous tissues while sparing healthy ones.
The Future of Medical Imaging
The future of medical imaging promises even greater precision, speed, and accessibility. Emerging technologies like quantum imaging, hyperpolarised MRI, and portable ultrasound devices are on the horizon, offering the potential for real-time, point-of-care diagnostics.
Quantum Imaging
Quantum imaging is an emerging field that uses quantum properties of light to create images with unprecedented detail. By exploiting the phenomenon of quantum entanglement, researchers are developing imaging systems that could surpass the resolution limits of current technologies. This could lead to earlier and more accurate diagnoses, especially in detecting microscopic changes in tissues.
Hyperpolarised MRI
Traditional MRI relies on the natural alignment of hydrogen atoms in a magnetic field, but this alignment is relatively weak, limiting the sensitivity of the images. Hyperpolarised MRI enhances this alignment by artificially boosting the signal from certain molecules, such as carbon-13. This technique could revolutionise the imaging of metabolic processes and provide more detailed information about diseases like cancer and heart conditions.
Portable and Wearable Imaging Devices
Advances in miniaturisation and wireless technology are paving the way for portable and wearable medical imaging devices. Portable ultrasound machines are already making their way into emergency rooms and rural clinics, providing immediate diagnostic capabilities in settings where traditional imaging is unavailable. Wearable imaging devices, such as MRI helmets, could allow for continuous monitoring of brain activity in patients with neurological conditions.
3D Printing and Medical Imaging
Another exciting frontier is the integration of medical imaging with 3D printing. By using imaging data to create precise 3D models of organs, bones, and tissues, healthcare professionals can plan surgeries with greater accuracy, create customised implants, and even print organs for transplantation research. This synergy between medical imaging and 3D printing holds enormous potential for improving patient outcomes and advancing personalised medicine.
Ethical and Societal Considerations in Medical Imaging
As medical imaging technologies advance, they raise important ethical and societal questions. The increasing use of AI in image analysis, for example, brings concerns about data privacy, algorithmic bias, and the role of human oversight. Additionally, the widespread use of imaging in preventive medicine, such as screening for cancers and heart disease, has led to debates about the potential harms of overdiagnosis and unnecessary interventions.
Radiation Exposure and Patient Safety
While many imaging modalities, such as MRI and ultrasound, do not involve ionising radiation, others, like X-rays and CT scans, do. Repeated exposure to ionising radiation carries a risk of radiation-induced cancer, especially in children and young adults. As imaging technology evolves, efforts are being made to reduce radiation exposure through techniques such as dose optimisation and alternative imaging methods.
For instance, advancements in low-dose CT technology allow for high-quality images while minimising the radiation dose to patients. Similarly, some conditions that traditionally required CT scans can now be effectively diagnosed using MRI, which poses no radiation risk. Continued efforts to balance diagnostic benefits with patient safety will be essential as imaging technologies become more widespread.
Overuse of Medical Imaging
The growing availability of advanced medical imaging has raised concerns about its potential overuse, leading to unnecessary procedures and interventions. For example, whole-body scans are sometimes marketed to healthy individuals as a preventive measure, but such screenings can result in false positives, leading to anxiety, unnecessary biopsies, and treatments that may not have been needed.
Additionally, the use of imaging in conditions where it may not significantly change the course of treatment—such as mild back pain—has been a topic of debate. The challenge lies in finding the right balance between leveraging the power of medical imaging for early detection and avoiding overdiagnosis and overtreatment.
Cost and Accessibility
While medical imaging has transformed healthcare, it is not without its challenges in terms of cost and accessibility. Advanced imaging techniques like MRI and PET scans are expensive and often require specialised equipment and personnel, making them less accessible in low-resource settings. This disparity in access can exacerbate health inequalities, as patients in under-served regions may not have the same opportunities for early diagnosis and treatment as those in more affluent areas.
Efforts to make imaging technologies more affordable and portable could help address these disparities. Portable ultrasound devices and other point-of-care imaging technologies have already shown promise in expanding access to diagnostic tools in remote and resource-limited areas. As technology advances, there is hope that medical imaging will become more accessible to patients around the world.
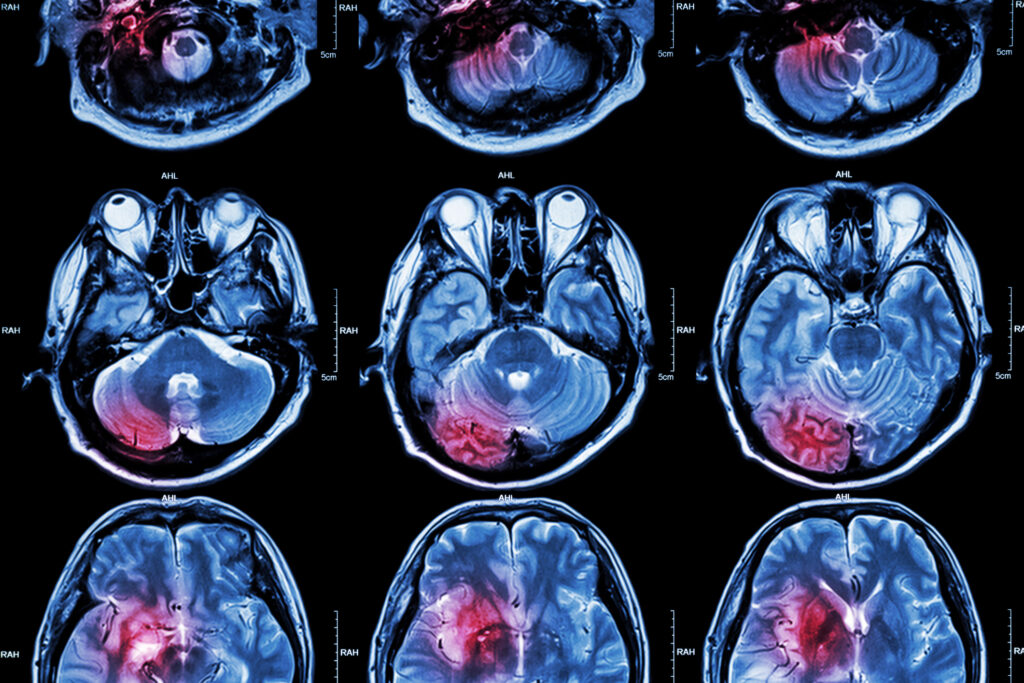
Imaging the Human Brain: Insights into Neurological Disorders
The human brain remains one of the most complex and least understood organs in the body. Imaging techniques such as MRI, fMRI, and PET have provided unprecedented insights into the brain’s structure and function, transforming the diagnosis and treatment of neurological and psychiatric disorders.
MRI in Neurological Diagnosis
MRI has become the go-to imaging technique for diagnosing a wide range of neurological disorders, including multiple sclerosis (MS), Alzheimer’s disease, and Parkinson’s disease. In MS, for example, MRI is used to detect lesions in the brain and spinal cord that indicate areas of demyelination, a hallmark of the disease. This allows for earlier diagnosis and more targeted treatment, potentially slowing disease progression.
In Alzheimer’s disease, MRI can detect structural changes in the brain, such as the shrinking of the hippocampus, long before symptoms like memory loss become apparent. Early detection of these changes is crucial for managing the disease and exploring potential therapeutic interventions.
Functional MRI and Brain Mapping
Functional MRI (fMRI) has revolutionised our understanding of how the brain works in real time. By measuring changes in blood flow, fMRI can identify which areas of the brain are active during specific tasks, such as speaking, moving, or solving problems. This ability to map brain activity has led to breakthroughs in understanding cognitive processes, as well as disorders like schizophrenia and autism.
One of the most exciting applications of fMRI is in pre-surgical planning for patients with brain tumours or epilepsy. Surgeons can use fMRI to map out critical areas of the brain responsible for language, motor function, and other essential processes, allowing them to avoid these areas during surgery. This reduces the risk of post-surgical complications and improves patient outcomes.
PET Scans and Neurological Disorders
Positron Emission Tomography (PET) has become an invaluable tool for studying the metabolic processes of the brain. In patients with Alzheimer’s disease, for instance, PET scans using specialised tracers can detect the build-up of amyloid plaques, a key feature of the disease. These scans are often used in conjunction with other imaging techniques to confirm a diagnosis and monitor disease progression.
PET is also used in the diagnosis of epilepsy, where it can identify areas of the brain with abnormal metabolic activity that may be triggering seizures. In patients with movement disorders like Parkinson’s disease, PET scans can detect abnormalities in the dopamine-producing neurons that are affected by the disease.
Imaging the Cardiovascular System
Cardiovascular disease remains one of the leading causes of death worldwide, and medical imaging plays a crucial role in diagnosing and managing heart and vascular conditions. From echocardiography to cardiac MRI, imaging technologies provide detailed insights into the structure and function of the heart and blood vessels.
Echocardiography: Imaging the Heart in Motion
Echocardiography, or ultrasound of the heart, is a widely used imaging technique that provides real-time images of the heart’s chambers, valves, and blood flow. It is commonly used to diagnose conditions such as heart valve disease, heart failure, and congenital heart defects. Doppler echocardiography, which measures the speed and direction of blood flow, is particularly useful in assessing conditions like heart murmurs and detecting blockages in blood vessels.
The non-invasive nature of echocardiography, combined with its ability to provide real-time, dynamic images, makes it an essential tool in cardiology. It is often used during stress tests to evaluate how the heart functions under physical exertion, helping clinicians assess the risk of heart attacks and other cardiovascular events.
Cardiac MRI: Detailed Imaging of the Heart’s Structure
Cardiac MRI offers a more detailed view of the heart’s anatomy than echocardiography. It provides high-resolution images of the heart’s muscle, valves, and blood vessels, making it particularly useful in diagnosing conditions such as myocarditis, cardiomyopathy, and heart tumours.
One of the key advantages of cardiac MRI is its ability to assess the viability of heart muscle after a heart attack. By using contrast agents, cardiac MRI can distinguish between damaged and healthy tissue, providing valuable information for treatment planning, such as determining whether a patient would benefit from revascularisation procedures like coronary artery bypass surgery.
Coronary CT Angiography: Visualising Blood Vessels
Coronary CT angiography is a specialised type of CT scan that provides detailed images of the coronary arteries, which supply blood to the heart. This non-invasive procedure has become a key tool in diagnosing coronary artery disease, as it allows clinicians to detect blockages or narrowing in the arteries that could lead to heart attacks.
By using contrast dye, coronary CT angiography provides a clear view of the blood vessels and helps assess the severity of blockages. It is particularly useful for patients with chest pain or those at high risk of cardiovascular disease. In some cases, it can even be used to guide treatment decisions, such as determining whether a patient needs a stent or other intervention.
Imaging in Oncology: Revolutionising Cancer Diagnosis and Treatment
Medical imaging has played a transformative role in the field of oncology, enabling earlier detection of cancers, precise tumour staging, and personalised treatment planning. From mammography to PET-CT, imaging technologies are critical in the fight against cancer.
Mammography: The Gold Standard for Breast Cancer Screening
Mammography remains the most effective imaging technique for the early detection of breast cancer. By using low-dose X-rays, mammography can identify tumours that are too small to be felt during a physical examination. Early detection through regular mammograms has been shown to significantly reduce breast cancer mortality by allowing for earlier treatment.
In recent years, digital mammography has improved the clarity and detail of images, making it easier to detect abnormalities in dense breast tissue. Tomosynthesis, or 3D mammography, has also emerged as a promising advancement, providing more accurate images and reducing the need for follow-up biopsies.
PET-CT in Cancer Diagnosis and Staging
PET-CT combines the metabolic imaging capabilities of PET with the anatomical detail of CT, making it a powerful tool in cancer diagnosis and staging. PET-CT scans are used to detect cancers, assess the extent of disease, and monitor treatment response. The ability to visualise both the tumour and its metabolic activity provides clinicians with valuable information for treatment planning.
For example, PET-CT is widely used in the management of lymphoma, where it can detect the presence of cancerous lymph nodes and guide decisions about chemotherapy or radiation therapy. In lung cancer, PET-CT can help determine whether the cancer has spread to other parts of the body, influencing decisions about surgery or systemic therapy.
MRI in Cancer Imaging
MRI is particularly useful for imaging soft tissue cancers, such as brain tumours, liver cancer, and prostate cancer. Its ability to provide high-resolution images without ionising radiation makes it an ideal choice for repeated imaging, especially in younger patients or those who require long-term monitoring.
In prostate cancer, for example, MRI can detect tumours at an early stage and provide detailed information about the tumour’s size and location, helping guide decisions about surgery or radiation therapy. MRI is also used to monitor response to treatment and detect any recurrence of cancer.
The Role of Medical Imaging in Personalised Medicine
Personalised medicine, also known as precision medicine, tailors medical treatments to individual patients based on their genetic, environmental, and lifestyle factors. Medical imaging is a key enabler of this approach, providing detailed information about a patient’s specific condition that can guide more targeted therapies.
Imaging Biomarkers and Precision Therapy
Medical imaging has the potential to identify imaging biomarkers—specific characteristics in scans that can indicate the presence or severity of a disease. These biomarkers are crucial in personalised medicine, as they help clinicians tailor treatments to the unique biological profile of a patient.
For instance, in oncology, imaging biomarkers can be used to assess how a tumour is likely to respond to certain treatments. This allows oncologists to select therapies that are more likely to be effective for a particular patient’s cancer, while avoiding treatments that may be ineffective or cause unnecessary side effects. This approach, known as theranostics, combines diagnosis and therapy in a single, integrated framework.
In cardiovascular medicine, imaging biomarkers can be used to assess a patient’s risk of heart disease by detecting early signs of plaque build-up in arteries or abnormal heart function. This enables clinicians to prescribe personalised preventive measures, such as lifestyle changes or medications, to reduce the patient’s risk of heart attacks or strokes.
Imaging-Guided Interventions
Medical imaging also plays a critical role in guiding minimally invasive procedures, allowing for more precise and targeted interventions. These imaging-guided procedures have revolutionised many areas of medicine, from oncology and cardiology to orthopaedics and neurosurgery.
In cancer treatment, for example, imaging techniques such as CT and ultrasound are used to guide needle biopsies, ensuring that the sample is taken from the precise location of the tumour. This reduces the need for open surgery and provides more accurate diagnostic information. Similarly, in interventional radiology, imaging is used to guide procedures such as the placement of stents, the ablation of tumours, and the repair of blood vessels.
The use of imaging-guided interventions has significantly improved patient outcomes by reducing the invasiveness of procedures, shortening recovery times, and lowering the risk of complications. As these techniques continue to advance, they will further enhance the precision and effectiveness of treatments, contributing to the broader goals of personalised medicine.
The Impact of Artificial Intelligence in Medical Imaging
The integration of artificial intelligence (AI) into medical imaging is rapidly transforming the field, offering new opportunities for more efficient and accurate diagnostics. AI has the potential to analyse complex imaging data faster and more accurately than human radiologists, providing valuable insights that can improve patient care.
AI-Driven Image Analysis
AI algorithms, particularly those based on machine learning and deep learning, can be trained to recognise patterns in medical images, such as the presence of tumours, fractures, or lesions. These algorithms have the ability to process vast amounts of imaging data in a fraction of the time it would take a human radiologist, helping to streamline the diagnostic process.
One of the key advantages of AI is its ability to detect subtle changes in imaging data that may be missed by the human eye. For instance, AI can identify early-stage cancers, such as small lung nodules or tiny breast tumours, with a high degree of accuracy. This early detection is critical for improving patient outcomes, as it allows for treatment to begin at a stage when the disease is more manageable.
AI-driven image analysis is also being used to assess disease progression and predict patient outcomes. In patients with chronic conditions such as multiple sclerosis or cardiovascular disease, AI can analyse imaging data to track changes over time and predict how the disease is likely to progress. This information can help clinicians make more informed decisions about treatment and care.
Workflow Efficiency and Reducing Diagnostic Errors
AI is also being used to improve workflow efficiency in radiology departments by automating routine tasks and prioritising urgent cases. For example, AI algorithms can automatically flag abnormal scans for immediate review, ensuring that patients with serious conditions receive timely care. This not only improves patient outcomes but also reduces the workload for radiologists, allowing them to focus on more complex cases.
In addition to enhancing efficiency, AI has the potential to reduce diagnostic errors, which are a significant concern in medical imaging. Misinterpretation of imaging data can lead to incorrect diagnoses and delayed treatments. AI algorithms, when used as a second reader alongside human radiologists, can provide an additional layer of verification, reducing the risk of errors and improving diagnostic accuracy.
Ethical Considerations and Challenges of AI in Medical Imaging
While the use of AI in medical imaging offers numerous benefits, it also raises important ethical and practical challenges. One of the primary concerns is the issue of data privacy, as AI relies on access to large datasets of medical images to train its algorithms. Ensuring that patient data is anonymised and protected is essential to maintaining trust in AI technologies.
Another challenge is the potential for algorithmic bias. AI systems are only as good as the data they are trained on, and if the training data is not representative of diverse populations, the algorithms may produce biased results. This could lead to disparities in diagnostic accuracy for certain patient groups, potentially exacerbating existing health inequalities.
Furthermore, the role of AI in medical decision-making raises questions about accountability. While AI can assist radiologists in making diagnoses, the final responsibility for clinical decisions still rests with human healthcare providers. Striking the right balance between leveraging the strengths of AI and maintaining human oversight will be critical as these technologies become more integrated into clinical practice.
Conclusion: The Expanding Horizons of Medical Imaging Technology
Medical imaging technology has revolutionised our ability to see inside the human body, providing detailed insights into anatomy, physiology, and disease processes. From the discovery of X-rays over a century ago to the development of sophisticated imaging techniques like MRI, PET, and ultrasound, medical imaging has become a cornerstone of modern healthcare.
As we look to the future, advances in imaging technologies, such as AI, quantum imaging, and hyperpolarised MRI, promise to push the boundaries of what is possible. These innovations will not only improve our ability to diagnose and treat diseases but also bring us closer to the goal of personalised medicine, where treatments are tailored to the unique needs of each patient.
At the same time, the widespread use of medical imaging raises important ethical and societal considerations, including the potential for overuse, disparities in access, and concerns about data privacy. Addressing these challenges will be essential to ensuring that the benefits of medical imaging are realised for all patients, regardless of where they live or their socio-economic status.
In conclusion, medical imaging technology has already transformed the landscape of healthcare, and its future potential is vast. As technology continues to evolve, medical imaging will remain a vital tool in diagnosing and treating disease, improving patient outcomes, and enhancing our understanding of the human body. The continued advancement of imaging technologies will undoubtedly play a pivotal role in shaping the future of medicine, helping clinicians provide more precise, effective, and personalised care for patients around the world.
Disclaimer
The content provided in this article, “Advances in Medical Imaging Technology: Unlocking the Mysteries of the Human Body”, is intended for informational and educational purposes only. It does not constitute professional medical advice, diagnosis, or treatment. While every effort has been made to ensure the accuracy of the information presented, Open Medscience does not guarantee the completeness or timeliness of the content. Medical imaging technologies and their applications may evolve, and practices may vary by region or clinical setting.
Readers should consult qualified healthcare professionals for advice on any specific medical condition or imaging procedure. Open Medscience and the article’s authors disclaim any liability for decisions made or actions taken based on the information contained herein.
home » blog » medical imaging modalities »