Medical imaging plays a crucial role in detecting and preventing heart disease. It allows doctors to visualise the heart’s structure, function, and blood flow, which helps them identify abnormalities and make accurate diagnoses.
The Role of Medical Imaging in Early Detection and Prevention of Heart Disease
Medical imaging of the heart is used to diagnose and prevent heart disease, a leading cause of death worldwide. In addition, imaging can help improve patient outcomes and quality of life by providing detailed and accurate information about the heart.
For example, heart imaging can investigate the following:
- Heart imaging can help diagnose various heart conditions, such as coronary artery disease, congenital heart defects, heart valve disease, and heart failure.
- Monitor heart disease progression and assess treatments’ effectiveness.
- Healthcare providers can determine the best course of treatment for heart conditions, such as medication, surgery, or lifestyle changes.
- Identify risk factors for heart disease, such as plaque build-up in the arteries or heart enlargement, allowing for early intervention and prevention of heart disease.
Advances in Medical Imaging of the Heart: Applications in Diagnosis, Treatment, and Prevention of Heart Disease
Medical imaging of the heart can be performed using several different modalities, including:
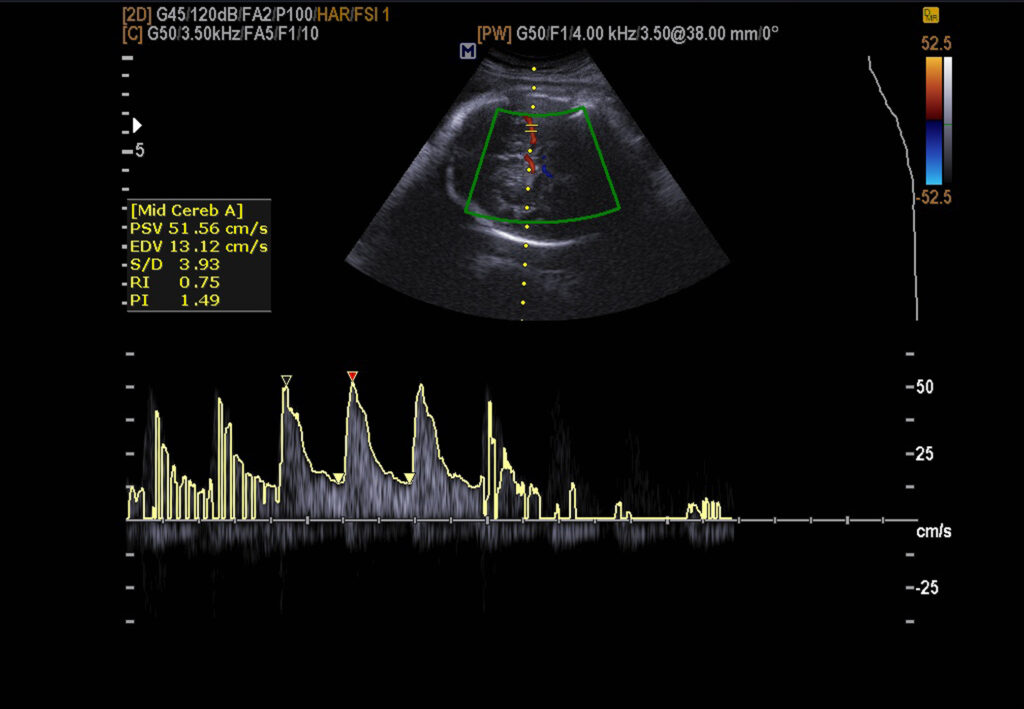
Echocardiography is a non-invasive imaging modality that uses ultrasound waves to generate images of the heart. It is a commonly used diagnostic tool for assessing the structure and function of the heart and diagnosing various heart conditions.
During an echocardiogram, a trained technician or physician places a small, hand-held device called a transducer on the chest, which emits high-frequency sound waves. These sound waves bounce off the heart’s structures and create images displayed on a monitor.
There are several types of echocardiograms, including:
- The transducer is placed on the chest in a transthoracic echocardiogram (TTE) to create heart images.
- Transesophageal echocardiogram (TEE) uses a small probe with a transducer passed down the throat and into the oesophagus to create more detailed images of the heart.
- Stress echocardiogram involves performing an echocardiogram before and after exercise to assess the heart’s function during physical activity.
Cardiac CT Imaging: Diagnosis of Cardiovascular Disease
During a cardiac CT scan, the patient lies on a table that travels through a large, doughnut-shaped machine called a CT scanner. The scanner emits X-rays detected by a series of detectors, which create detailed images of the heart and surrounding blood vessels.
There are different types of cardiac CT scans, including:
- Calcium scoring involves a non-contrast CT scan that detects the presence of calcium in the coronary arteries, which is an indication of coronary artery disease.
- Coronary CT angiography (CTA) involves a contrast-enhanced CT scan that provides detailed images of the coronary arteries to detect blockages or narrowing.
- Cardiac CT for pulmonary embolism involves a contrast-enhanced CT scan that detects the presence of blood clots in the pulmonary arteries.
Cardiac CT scanning is safe but exposes the patient to a small amount of radiation. In addition, patients with kidney disease or allergies to contrast dye may not be candidates for cardiac CT.
Cardiac Magnetic Resonance Imaging: Diagnosis of Cardiovascular Disease
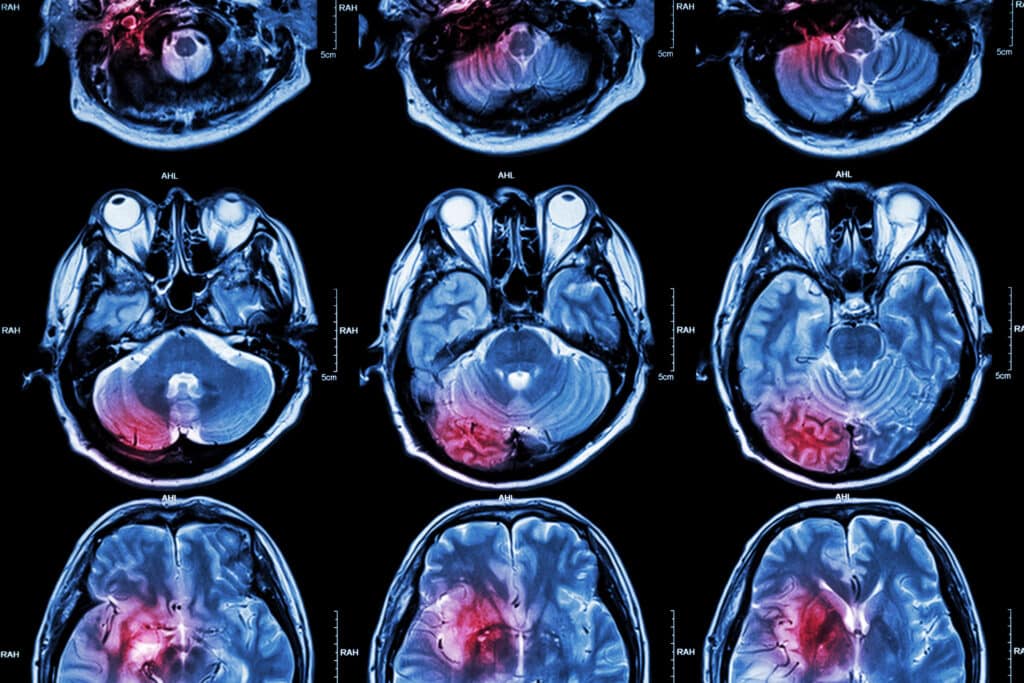
Magnetic resonance imaging (MRI) is valuable for diagnosing various heart conditions, including heart valve disease, heart failure, and congenital heart defects.
During a cardiac MRI, the patient lies on a table that travels through a large, doughnut-shaped machine. The patient is subjected to a strong magnetic field and radio waves to create images of the heart and surrounding blood vessels.
There are different types of cardiac MRI scans, including:
- Cine MRI involves creating a series of images that show the heart’s movement over time. It can provide information about the heart’s size, shape, and function.
- Cardiac MRI with contrast involves the injection of a contrast dye into the bloodstream, which enhances the images of the heart and blood vessels.
- Magnetic resonance angiography (MRA) involves the creation of detailed images of the blood vessels in and around the heart.
Cardiac MRI is generally safe, but it is not recommended for patients with certain types of metallic implants or devices, such as pacemakers or defibrillators. In addition, patients with kidney disease may also not be candidates for cardiac MRI with contrast. Therefore, discussing any concerns with a healthcare provider before undergoing a cardiac MRI is essential.
Myocardial Perfusion Imaging in the Evaluation of Coronary Artery Disease
Myocardial perfusion imaging is a non-invasive diagnostic imaging technique that uses a small amount of radioactive material to create images of blood flow to the heart muscle. It is also known as nuclear stress testing or radionuclide myocardial perfusion imaging (MPI).
During a myocardial perfusion imaging test, a small amount of radioactive tracer material is injected into the patient’s bloodstream, which is then taken up by the heart muscle. The patient then undergoes a series of images through SPECT (single-photon emission computed tomography) or PET (positron emission tomography) imaging to visualise the blood flow to the heart muscle.
The test is typically performed while the patient rests and again while exercising or under stress. By comparing the images obtained at rest with those obtained under stress, doctors can identify areas of reduced blood flow to the heart, which may indicate a heart condition such as coronary artery disease.
Myocardial perfusion imaging is generally considered a safe procedure with few risks or side effects. However, it may not be suitable for patients with certain medical conditions, such as pregnancy or kidney disease. Therefore, discussing any concerns with a healthcare provider before undergoing a myocardial perfusion imaging test is imperative.
Myoview is a brand name for a radioactive tracer material used in myocardial perfusion imaging (MPI). The tracer material is a small amount of technetium-99m, which is injected into the patient’s bloodstream during the imaging procedure.
Once injected, the Myoview tracer is taken up by the heart muscle, allowing doctors to visualise blood flow to the heart and detect any areas of reduced blood flow or blockages in the coronary arteries.
Myoview is commonly used with either SPECT (single-photon emission computed tomography) or PET (positron emission tomography) imaging to produce detailed images of the heart muscle and surrounding blood vessels.
As with any imaging procedure involving radioactive material, there is a small risk of radiation exposure associated with Myoview imaging. However, the dose of radiation used in MPI is generally considered safe, and the benefits of the test in diagnosing and treating heart disease typically outweigh the risks.
Coronary Angiography: Imaging in Cardiovascular Disease
Angiography of the heart, also known as coronary angiography, is an imaging test that uses X-ray technology and a contrast dye to visualise the heart’s blood vessels, including the coronary arteries. It is used to diagnose and evaluate heart conditions such as heart valve disease, coronary artery disease and congenital heart defects.
During coronary angiography, a catheter is inserted into an artery, usually in the groin or wrist, and threaded up to the heart. Then, a contrast dye is injected through the catheter and into the coronary arteries. X-ray images are taken as the dye flows through the arteries, allowing doctors to visualise any blockages or narrowing in the arteries.
Coronary angiography is generally a safe procedure, but it does carry some risks, including infection, bleeding and damage to the artery or surrounding tissue. There is also a possible risk of an allergic reaction from the contrast dye during the procedure.
Depending on the angiography results, further treatment may be necessary, such as angioplasty to open blocked arteries or surgery to repair or replace a heart valve.
During a CT angiography, the patient lies on a table that moves through a CT scanner. The scanner uses X-rays to create detailed images of the heart and surrounding blood vessels. Then, a contrast dye is injected into the patient’s bloodstream to enhance the images of the blood vessels.
CT angiography is generally considered safe, but it does carry some risks, including allergic reactions to the contrast dye, radiation exposure, and kidney damage in patients with pre-existing kidney problems.
CT angiography may not be suitable for patients with certain medical conditions, such as pregnancy or kidney disease, or for those who cannot lie still for an extended period.
The choice of imaging modality will depend on the specific clinical situation and the information required by the healthcare provider.
Emerging Technologies in Cardiac Imaging: The Next Frontier in Cardiovascular Diagnosis and Treatment
The future of heart imaging will likely involve continued advancements in technology and techniques that provide more detailed and accurate information about the structure and function of the heart. Some possible future developments include:
- Artificial intelligence and machine learning: Both of these technologies can be used to analyse vast amounts of imaging data and provide insights into heart function and disease.
- Advanced imaging techniques that allow for detailed 3D and even 4D (3D plus time) heart images can provide better visualisation and understanding of heart function and abnormalities.
- Techniques that allow for the visualisation of specific molecules in the heart, such as proteins or enzymes, can provide information about disease processes at a cellular level.
- Miniature sensors that can be worn or implanted in the body can continuously monitor heart function, potentially allowing for earlier detection of heart disease and personalised treatment.
- Advancements in noninvasive imaging techniques, such as MRI and CT, may allow for more accurate and detailed heart imaging without requiring invasive procedures.
The future of heart imaging is likely to focus on more personalised and precise diagnosis and treatment of heart disease, leading to improved patient outcomes and quality of life.
Disclaimer
The content presented in this article is intended for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider with any questions you may have regarding a medical condition or before undertaking any diagnostic imaging procedure.
Open Medscience does not endorse or recommend any specific tests, treatments, procedures, or opinions mentioned in this article. The information provided is accurate to the best of our knowledge at the time of publication (18 March 2023) but may not reflect the most current developments in cardiac imaging or related medical practices.
Readers are advised not to rely solely on the information contained herein and should consult a medical professional or specialist before making any decisions related to their health or treatment options. Open Medscience shall not be liable for any loss, injury, or damage resulting from the use or misuse of the information contained in this publication.
You are here: home » diagnostic medical imaging blog »