Cancer remains one of the most formidable challenges in modern medicine. Its complexity, ability to metastasize, and resistance to traditional therapies make it a difficult disease to treat and manage. However, one of the most promising advancements in oncology in recent years has been the development and use of cancer markers. These biomarkers are transforming how healthcare professionals monitor cancer treatment, offering more personalized, accurate, and efficient ways to track a patient’s response to therapy.
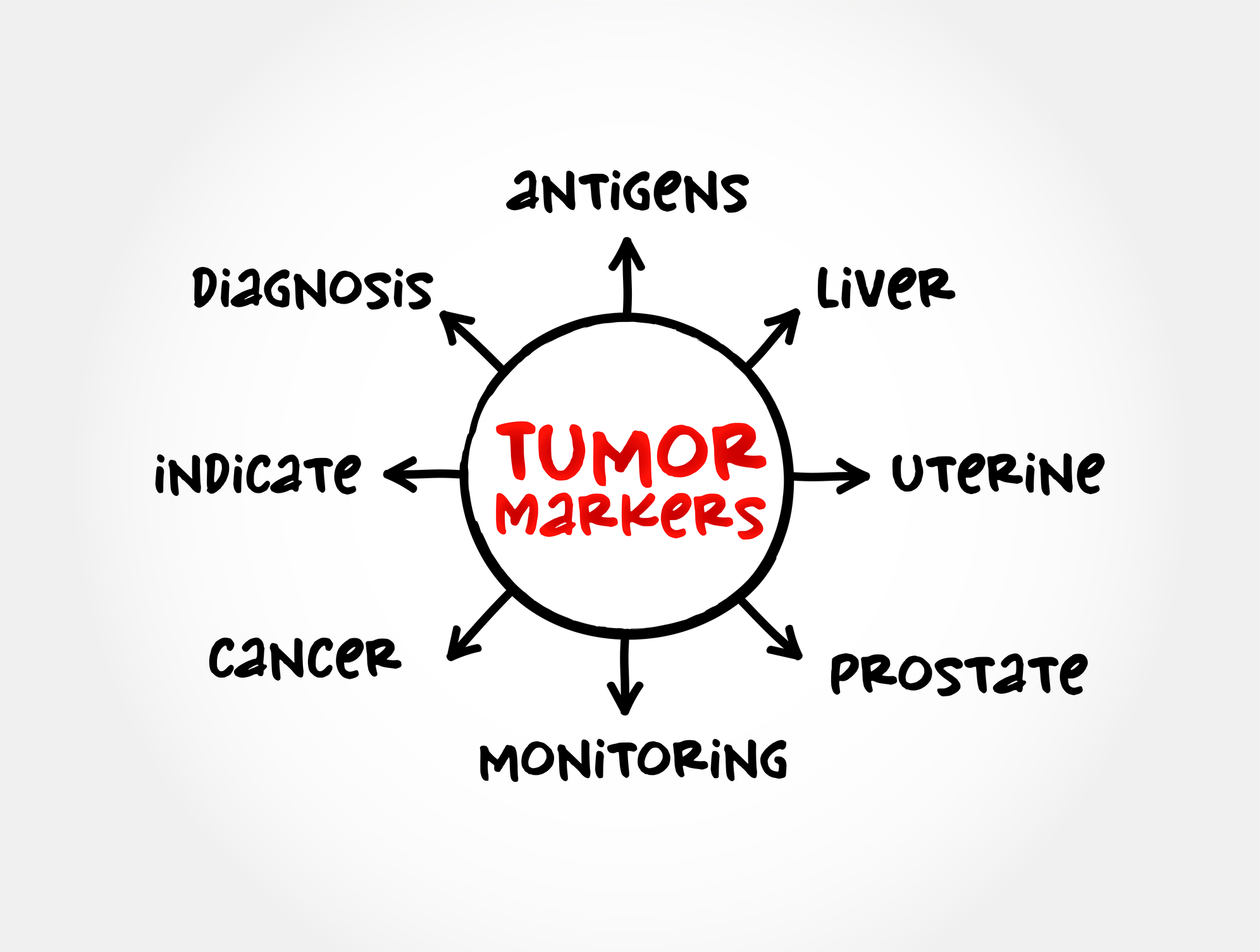
What Are Cancer Markers?
Cancer markers, also known as tumor markers or cancer biomarkers, are substances found in the blood, urine, tissues, or other bodily fluids that are produced by the body in response to cancer or by the cancer cells themselves. These markers can offer valuable insights into the presence, progression, and response to treatment of various cancers.
There are many types of cancer markers, including proteins, DNA, RNA, and other molecular markers. Common cancer markers include:
- PSA (Prostate-Specific Antigen): A protein often elevated in prostate cancer.
- CA-125: A protein found in higher levels of ovarian cancer.
- HER2 (Human Epidermal Growth Factor Receptor 2): A protein overexpressed in certain types of breast cancer.
- EGFR (Epidermal Growth Factor Receptor): A gene mutation linked to lung cancer.
These markers are not only crucial for diagnosing cancer but are also central to monitoring how well treatments are working.
How Cancer Markers Are Used in Treatment Monitoring
Cancer markers have become indispensable in the monitoring of treatment progress. Traditionally, monitoring cancer treatment involved imaging tests, biopsies, and other invasive procedures, but with the advent of cancer biomarkers, doctors can now track the effectiveness of treatment in real-time through non-invasive tests. Here’s how cancer markers are used in treatment monitoring:
Detection and Early Diagnosis
Cancer biomarkers are instrumental in detecting cancer early. For example, elevated levels of PSA in the blood can indicate prostate cancer before physical symptoms develop. Similarly, markers like CA-125 in ovarian cancer can help in identifying the disease at earlier stages, potentially leading to quicker interventions and better outcomes.
Treatment Response Assessment
One of the primary uses of cancer biomarkers is assessing how well a treatment is working. By measuring specific tumor markers over time, doctors can gauge the effectiveness of chemotherapy, immunotherapy, or targeted therapy. For example, if levels of the HER2 marker decrease in response to breast cancer treatment, it suggests the treatment is effectively targeting and reducing the tumor cells that express HER2.
Personalized Treatment Adjustments
Because cancer treatment is not one-size-fits-all, cancer markers allow for a more personalized approach. Through the use of biomarkers, doctors can determine which therapies are most likely to work for a particular patient based on the tumor’s unique molecular profile. This approach maximizes the chances of successful treatment while minimizing unnecessary side effects from ineffective therapies.
The Advantages of Using Cancer Markers
The use of cancer markers in monitoring treatment has numerous advantages. These benefits extend beyond simply detecting cancer; they are revolutionizing how healthcare providers tailor and manage cancer care.
Early Detection and Diagnosis
One of the greatest advantages of cancer biomarkers is their ability to detect cancer at very early stages. By identifying cancer before physical symptoms appear, biomarkers enable earlier intervention, which is critical in improving long-term survival rates. For instance, detecting colorectal cancer with biomarkers like CEA (Carcinoembryonic Antigen) allows for earlier treatment, leading to a higher likelihood of successful outcomes.
Personalized Treatment
Cancer is not a single disease but a collection of disorders that vary greatly between individuals. Biomarkers help doctors tailor treatment plans based on each patient’s specific cancer type, genetic makeup, and molecular profile. This personalized approach, also known as precision medicine, ensures that the most effective therapies are chosen for each individual, reducing the trial-and-error approach and improving treatment outcomes.
Minimizing Invasive Procedures
Monitoring cancer through traditional means often requires invasive procedures such as biopsies or imaging scans, which can be costly and uncomfortable. With the presence of cancer biomarkers in blood, doctors can monitor a patient’s condition through simple blood tests that measure the activity levels of some of these markers. This non-invasive method can potentially reduce the need for frequent hospital visits, lowers healthcare costs, and provide patients with a more comfortable experience throughout their treatment.
Challenges in Cancer Marker Use
Despite the many advantages, the use of cancer markers is not without challenges. The following are some of the limitations and hurdles still faced by the medical community:
Variability in Marker Levels
Cancer marker levels can fluctuate due to various factors such as a patient’s age, comorbid conditions, or the type of cancer being treated. This variability can make it difficult to establish universal thresholds for what constitutes a “normal” or “abnormal” level of a marker, leading to potential misinterpretation of results.
Lack of Standardization
Although many cancer biomarkers are well-established, the methods used to detect and quantify them can vary between laboratories and institutions. This lack of standardization means that results might not always be consistent, making it harder to rely on biomarkers for accurate decision-making.
Interpretation of Results
The interpretation of cancer marker data is complex. While elevated levels of certain markers may indicate cancer progression, they can also be caused by other conditions, leading to false positives. Similarly, low marker levels may not always correlate with tumor regression, leading to false negatives. This makes it crucial for healthcare providers to consider multiple factors, including patient history and imaging results when interpreting biomarker data.
Conclusion
Cancer biomarkers are changing the landscape of cancer treatment monitoring, offering more personalized, accurate, and less invasive methods to track disease progression and response to therapy. As technology advances and new markers are discovered, these tools will continue to enhance the precision and effectiveness of cancer care, improving outcomes and quality of life for patients around the world.
Disclaimer
The content of this article is intended for informational purposes only and does not constitute medical advice, diagnosis, or treatment. While efforts have been made to ensure accuracy, Open Medscience makes no guarantees about the completeness or reliability of the information provided. Readers should consult qualified healthcare professionals regarding any medical concerns or before making decisions related to cancer diagnosis or treatment. The views expressed are those of the author and do not necessarily reflect the official policy or position of any medical or governmental organisation.