- Introduction to Radiopharmaceuticals
- Importance of Lutetium in Radiopharmaceuticals
- Methods of Production for Lutetium Isotopes in Radiopharmaceuticals
- Quality Control and Standardisation in the Production of Lutetium Radiopharmaceuticals
- How Lutetium Radiopharmaceuticals Work at a Cellular Level
- Targeting Specific Cancers or Conditions with Lutetium Radiopharmaceuticals
- Overview of Diseases and Conditions Treated with Lutetium Radiopharmaceuticals
- Case Studies and Clinical Trial Results for Lutetium Radiopharmaceuticals
- Detailed Discussion on Lutetium-Based Drugs: A Focus on Lutathera
- Administration Procedures and Dosing for Lutetium Radiopharmaceuticals
- Potential Side Effects and Risks Associated with Lutetium Radiopharmaceuticals
- Patient Monitoring and Safety Protocols for Lutetium Radiopharmaceuticals
- Overview of the Regulatory Landscape for Lutetium Radiopharmaceuticals
- Research Advancements in Lutetium Radiopharmaceuticals
- Future Potential and Emerging Trends
- Summary of the Impact of Lutetium Radiopharmaceuticals in Medicine
- Future Outlook
- Conclusion
Lutetium radiopharmaceuticals, notably 177Lu, are transforming cancer treatment through targeted therapy and diagnostic advancements, promising a personalised medicine future.
Introduction to Radiopharmaceuticals
Radiopharmaceuticals represent a unique and increasingly important area in the field of medical diagnostics and therapeutics. These specialised drugs are designed to interact with specific physiological processes within the body, often for the purposes of imaging or treatment, particularly in the field of nuclear medicine.
At the heart of radiopharmaceuticals is the combination of a radioactive compound and a pharmaceutical component. The radioactive part, often a radioisotope, is what makes these drugs distinctive. It emits radiation that can be detected by medical imaging equipment, allowing for highly detailed visualisation of internal bodily structures and processes. This feature is crucial in diagnostic procedures, particularly in identifying, staging, and monitoring various diseases.
Radiopharmaceuticals are used primarily in Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) scans in diagnostic applications. These scans provide vital information about the functioning of different organs and tissues, offering insights into conditions like cancer, heart disease, neurological disorders, and more.
Therapeutically, radiopharmaceuticals are used in the treatment of certain types of cancers and other diseases. Here, the radioactive component serves a different purpose: it delivers targeted radiation to diseased cells, helping to destroy or diminish them while minimising damage to surrounding healthy tissue. This approach is particularly valuable in treating specific cancers, such as thyroid cancer, where targeted radiation can be more effective and less invasive than traditional treatments.
The choice of radioisotope is critical and varies depending on the intended use. Isotopes like technetium-99m are widely used in diagnostic imaging due to their ideal physical properties and short half-life, minimising radiation exposure. For therapeutic purposes, isotopes like iodine-131 or lutetium-177 are chosen for their ability to deliver therapeutic radiation doses to specific tissues.
The development and use of radiopharmaceuticals are subject to stringent regulatory controls due to their radioactive nature. Ensuring the safety and efficacy of these drugs for patients is paramount. This involves rigorous testing, quality control, and adherence to safety guidelines in their handling, storage, and administration.
Importance of Lutetium in Radiopharmaceuticals
Lutetium, particularly its isotope lutetium-177 (177Lu), has emerged as a significant player in the field of radiopharmaceuticals. Its unique properties and applications have made it a valuable tool in diagnostic imaging and targeted radiotherapy, especially in treating various cancers.
Unique Characteristics
- Ideal Half-Life: 177Lu has a half-life of about 6.65 days, which is long enough to allow for the production, preparation, and application of the radiopharmaceutical but short enough to minimise prolonged radiation exposure to the patient.
- Emission Profile: It emits both beta particles and gamma radiation. The beta radiation is therapeutic and effective in destroying cancer cells, while the gamma emission allows for imaging and tracking the distribution of the radiopharmaceutical within the body.
- Low Energy Beta Emission: The relatively low energy of its beta emissions (maximum energy of 0.497 MeV) results in a short tissue penetration range (maximum 2 mm). This characteristic is beneficial in minimising damage to surrounding healthy tissues while effectively targeting tumour cells.
Therapeutic Applications
- Cancer Treatment: 177Lu-based radiopharmaceuticals, such as lutetium-177 dotatate (Lutathera), are primarily used in treating neuroendocrine tumours (NETs). This type of cancer originates from cells of the neuroendocrine system and is often found in the gastrointestinal tract and pancreas.
- Prostate Cancer: Recent advancements have also seen the application of 177Lu in treating metastatic castration-resistant prostate cancer, offering a new therapeutic avenue for patients with limited treatment options.
- Personalised Treatment: The ability to target specific cancer cells while sparing healthy tissue makes 177Lu radiopharmaceuticals a form of personalised medicine. They can be tailored to the patient’s specific type of cancer, improving treatment efficacy and reducing side effects.
Diagnostic Capabilities
- Imaging: The gamma radiation emission of 177Lu enables single-photon emission computed tomography (SPECT) imaging. This aids in diagnosing, staging, and monitoring the response of cancers to treatment, providing valuable information for personalised treatment planning.
Research and Development
- Innovative Treatments: Ongoing research is exploring new ligands and targeting molecules to be labelled with 177Lu, expanding the potential to treat various types of cancers.
- Clinical Trials: Numerous clinical trials are underway to evaluate the efficacy and safety of 177Lu-based therapies in different oncological indications, signifying its growing importance in the field.
The significance of lutetium, especially 177Lu, in radiopharmaceuticals cannot be overstated. Its combination of therapeutic and diagnostic capabilities – often referred to as “theranostics” – represents a major advancement in personalised medicine, particularly in oncology. As research progresses, lutetium-based therapies are expected to play an increasingly vital role in the management of cancer and potentially other diseases, marking a new era in targeted and effective treatment strategies.
Methods of Production for Lutetium Isotopes in Radiopharmaceuticals
Lutetium-177 is the most widely used isotope of lutetium in radiopharmaceuticals. Its production methods are crucial for ensuring its availability, purity, and suitability for medical applications. Two main methods for producing 177Lu are neutron activation and direct production.
Neutron Activation
- Process Overview: This method involves irradiating a stable lutetium target, usually lutetium-176 (176Lu), with neutrons. The neutron capture process converts 176Lu into 177Lu.
- Reactors Used: The irradiation typically occurs in nuclear reactors, which provide a high flux of neutrons necessary for the process.
- Advantages: This method is widely used due to its relatively straightforward process and the ability to produce high-purity 177Lu, as the only contaminant is generally lutetium-177m (a metastable isomer), which decays to 177Lu.
- Challenges: The major challenge is the availability and access to nuclear reactors capable of providing the necessary neutron flux. Additionally, the presence of long-lived radioactive isotopes in the irradiated target requires careful handling and waste management.
Direct Production
- Process Overview: Direct production involves using particle accelerators like cyclotrons to irradiate targets like ytterbium-176 (176Yb) with protons or deuterons. The interaction leads to a nuclear reaction that directly produces 177Lu.
- Specific Reactions: Common reactions include 176Yb(d,n)177Lu and 176Yb(p,n)177Lu, where d and p represent a deuteron and proton, respectively.
- Advantages: This method allows for the production of 177Lu without the need for a nuclear reactor. It can also result in a product with lower levels of long-lived radioactive contaminants compared to the neutron activation method.
- Challenges: The direct production method may yield 177Lu with a lower specific activity, which might not be suitable for certain radiopharmaceutical applications. Also, the availability and cost of the target material (176Yb) and the need for specialised facilities like cyclotrons can be limiting factors.
Quality Control and Standardisation
- Purity Requirements: The produced 177Lu must meet stringent purity criteria, including specific activity, radionuclidic purity, and chemical purity.
- Regulatory Compliance: Producers must adhere to regulatory standards for the production of medical-grade isotopes, ensuring that the final product is safe and effective for clinical use.
- Transport and Handling: Given the radioactive nature of 177Lu, its transport and handling require specialised protocols to ensure safety and maintain its integrity.
The production of lutetium-177 for radiopharmaceutical applications is a complex process that demands technical expertise and adherence to safety and quality standards. Both neutron activation and direct production methods have their advantages and challenges, and the choice between them often depends on the availability of facilities, desired purity, and specific activity required for medical applications. As the demand for 177Lu in medical treatments increases, advancements in production methods are expected to enhance its availability and efficacy in clinical settings.
Quality Control and Standardisation in the Production of Lutetium Radiopharmaceuticals
Quality control and standardisation are critical components in the production of lutetium-based radiopharmaceuticals, particularly 177Lu. Ensuring these radiopharmaceuticals’ safety, efficacy, and consistency requires rigorous processes and adherence to established standards.
Radionuclidic Purity
- Definition: Radionuclidic purity refers to the proportion of the desired radionuclide (177Lu) in the total radioactive content.
- Importance: High radionuclidic purity is essential to minimise patient exposure to unnecessary radiation and ensure the radiopharmaceutical’s effectiveness.
- Testing: It involves measuring the presence of other radionuclides, which could be a result of the production process. Gamma spectroscopy is commonly used for this assessment.
Radiochemical Purity
- Definition: Radiochemical purity is the proportion of the radionuclide in the desired chemical form.
- Importance: Ensuring that 177Lu is in the correct chemical form (e.g., bound to the right ligand or molecule for targeting cancer cells) is crucial for its effectiveness and safety.
- Testing: Techniques like high-performance liquid chromatography (HPLC) are employed to determine radiochemical purity.
Specific Activity
- Definition: Specific activity refers to the radioactivity per unit mass of the radiopharmaceutical.
- Importance: It determines the therapeutic effectiveness of the radiopharmaceutical, especially for targeting specific types of cancer cells.
- Standardisation: The specific activity should meet the requirements for the intended clinical application.
Chemical Purity
- Definition: This refers to the absence of non-radioactive impurities in the radiopharmaceutical.
- Importance: Impurities can affect the safety and efficacy of the treatment. They might also cause adverse reactions in patients.
- Testing: Methods like mass spectrometry and atomic absorption spectroscopy are used to assess chemical purity.
Sterility and Endotoxin Testing
- Sterility: Radiopharmaceuticals must be sterile to prevent infections.
- Endotoxins: Low levels of endotoxins are crucial to prevent harmful immune reactions. Tests are conducted to ensure endotoxin levels are within safe limits.
Pharmacopeia Standards
- Regulatory Compliance: Producers must adhere to standards set by pharmacopoeias (e.g., USP, EP), which provide guidelines on the production, testing, and quality requirements for pharmaceuticals.
- Documentation: Complete and accurate documentation of production, quality control tests, and outcomes is mandatory for regulatory compliance and traceability.
Shelf Life and Stability
- Testing: Stability studies are conducted to determine the shelf life of the radiopharmaceutical, ensuring it remains effective and safe for use during its intended shelf life.
- Storage Conditions: Standardised storage conditions are established to maintain the stability of the radiopharmaceutical.
Packaging and Labelling
- Safe Packaging: Radiopharmaceuticals require specialised packaging to protect handlers and transporters from radiation exposure.
- Labelling: Labels must provide essential information, including radionuclide content, activity, expiration date, and safety warnings.
Quality control and standardisation in the production of lutetium-based radiopharmaceuticals are paramount for patient safety and treatment efficacy. The adherence to strict regulatory guidelines and quality standards ensures that these sophisticated medical products are safe, effective, and reliable for clinical use. As the field of nuclear medicine evolves, these standards are continually updated to reflect new research findings and technological advancements.
How Lutetium Radiopharmaceuticals Work at a Cellular Level
Lutetium radiopharmaceuticals operate on the principle of targeted radiation therapy, particularly those involving 177Lu. At the cellular level, their mechanism of action involves several key steps that allow them to selectively target and destroy cancer cells while minimising harm to normal tissues. This section delves into these processes.
Targeting Specific Cells
- Ligand Binding: 177Lu is attached to a molecule (ligand) that specifically targets cancer cells. For example, 177Lu is often bound to a somatostatin analogue in neuroendocrine tumours. These analogues mimic somatostatin, a hormone for which neuroendocrine tumours often have receptors.
- Receptor Binding: The ligand-radioisotope complex binds to specific receptors expressed on the surface of the cancer cells. This highly selective process ensures that the radiopharmaceutical accumulates primarily in the cancer cells, sparing most of the normal cells.
Internalisation and Localisation
- Cellular Uptake: The complex is often internalised into the cell once bound to the cancer cell receptors. This internalisation is crucial for the therapeutic radioisotopes to be in close proximity to critical cellular components.
- Targeting the Nucleus: After internalisation, the 177Lu radiopharmaceutical tends to localise near the cell’s nucleus, which houses the DNA.
Radiation Emission
- Beta Radiation: 177Lu emits beta particles (electrons) as a form of radiation therapy. These particles have a relatively short path length, typically only travelling a short distance within tissues (up to a few millimetres).
- DNA Damage: The emitted beta particles cause ionisation and create free radicals when they collide with atoms and molecules within the cells. These free radicals can directly or indirectly damage the DNA of the cancer cells.
Cellular Damage and Apoptosis
- DNA Damage Mechanism: The primary mechanism of cell killing is through the induction of irreparable DNA damage. The double-strand breaks in DNA caused by the radiation are particularly lethal to cells.
- Inducing Apoptosis: If the DNA damage is severe and irreparable, it triggers the process of apoptosis, or programmed cell death, in cancer cells.
- Limited Damage to Surrounding Tissue: Due to the short path length of the beta particles, the damage to surrounding healthy tissue is limited, making this a targeted therapeutic approach.
Gamma Radiation for Imaging
- Diagnostic Capability: Besides therapeutic beta particles, 177Lu also emits gamma rays. These gamma rays can be detected using imaging techniques like Single Photon Emission Computed Tomography (SPECT), enabling doctors to visualise the distribution of the radiopharmaceutical within the body.
Lutetium radiopharmaceuticals represent a sophisticated and highly targeted approach to cancer treatment. By combining the specificity of molecular targeting with the potent cell-killing ability of beta radiation, these drugs offer a powerful tool in the fight against cancer. This mechanism of action at the cellular level underscores the potential of radiopharmaceuticals as a personalised treatment modality in oncology, particularly for cancers that are difficult to treat with conventional therapies.
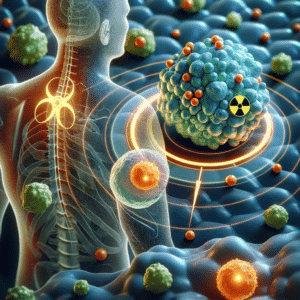
Targeting Specific Cancers or Conditions with Lutetium Radiopharmaceuticals
Lutetium radiopharmaceuticals, notably those containing lutetium-177, have shown significant promise in targeting specific types of cancers and medical conditions. Their ability to deliver targeted radiation therapy makes them particularly effective in treating certain malignancies where traditional therapies may be less effective or have significant side effects.
Neuroendocrine Tumours (NETs)
- Targeting Mechanism: Many neuroendocrine tumours overexpress somatostatin receptors. Radiopharmaceuticals like lutetium-177 dotatate (Lutathera) are designed to target these receptors.
- Efficacy: Treatment with lutetium-177 dotatate has been shown to be effective in controlling tumour growth, reducing symptoms, and improving survival rates in patients with advanced, metastatic NETs, particularly those originating in the gastrointestinal tract and pancreas.
Prostate Cancer
- PSMA Targeting: Prostate-Specific Membrane Antigen (PSMA) is frequently overexpressed in prostate cancer cells. 177Lu-labelled PSMA inhibitors can specifically target these cells.
- Treatment for Advanced Cases: This approach is particularly valuable for metastatic castration-resistant prostate cancer (mCRPC), offering a new treatment avenue for patients who have limited response to conventional therapies.
Bone Metastases
- Pain Palliation: 177Lu-labelled radiopharmaceuticals are also explored for the palliation of pain in bone metastases. They target bone lesions, providing relief from pain caused by the spread of cancer, especially in cases of prostate and breast cancer.
Other Potential Applications
- Research and Trials: Ongoing research and clinical trials are investigating the use of 177Lu in other types of cancers. These include lymphomas, leukaemia, and certain types of brain tumours.
- Radiosynovectomy: There is also interest in using 177Lu for radiosynovectomy – a treatment for inflammatory joint conditions like rheumatoid arthritis, where it could help reduce inflammation and pain.
Personalised Treatment
- Theranostics Concept: Lutetium radiopharmaceuticals embody the concept of “theranostics” – a combination of therapy and diagnostics. This approach allows for personalised treatment, where the therapeutic agent is also used for diagnostic imaging to monitor treatment response and adjust therapy accordingly.
- Tailored Therapy: By assessing the expression of specific markers (like somatostatin receptors or PSMA), treatments can be tailored to the individual patient’s tumour characteristics, enhancing efficacy and reducing unnecessary exposure to non-effective treatments.
Lutetium radiopharmaceuticals represent a significant advancement in the targeted treatment of certain cancers and medical conditions. By specifically targeting cancer cells or pain-causing lesions while sparing healthy tissues, these treatments offer new hope for patients with challenging conditions, particularly those with advanced, metastatic, or treatment-resistant cancers. As research continues, the potential applications of lutetium in the field of radiopharmaceuticals are likely to expand, further enhancing the role of personalised medicine in cancer treatment.
Overview of Diseases and Conditions Treated with Lutetium Radiopharmaceuticals
Lutetium radiopharmaceuticals, particularly those based on lutetium-177, have been increasingly utilised in the treatment of various diseases and conditions, primarily in the field of oncology. These targeted therapies offer a novel approach for conditions where conventional treatments may be less effective or pose significant side effects. Here’s an overview of some key diseases and conditions where Lutetium radiopharmaceuticals are making an impact:
Neuroendocrine Tumors (NETs)
- Common Target: NETs often express somatostatin receptors, making them suitable targets for 177Lu-based therapies, such as lutetium-177 dotatate (Lutathera).
- Effectiveness: This therapy has shown significant results in reducing tumour size, slowing disease progression, and improving survival rates, especially in advanced cases of gastrointestinal and pancreatic NETs.
Prostate Cancer
- Targeting PSMA: Prostate-Specific Membrane Antigen (PSMA) is a protein overexpressed in most prostate cancer cells. 177Lu-PSMA therapy targets these cells for the treatment of metastatic castration-resistant prostate cancer (mCRPC).
- Clinical Results: This approach has demonstrated promising outcomes in reducing tumour burden and PSA levels, especially in patients who have exhausted other treatment options.
Bone Metastases
- Pain Management: 177Lu radiopharmaceuticals are used for palliative treatment of bone pain due to metastases, common in cancers like breast and prostate cancer.
- Mechanism: The therapy targets bone lesions, providing pain relief and potentially slowing the progression of bone metastases.
Lymphoma
- Potential Application: Research is ongoing to explore the use of 177Lu in treating certain types of lymphoma, where it could offer a targeted approach to destroy lymphoma cells while sparing healthy tissue.
Leukaemia
- Experimental Use: There is investigative work on the use of 177Lu for certain types of leukaemia. The approach would involve targeting leukaemia cells with a 177Lu-labelled compound.
Radiosynovectomy
- Application in Rheumatology: 177Lu is being explored for use in radiosynovectomy, a treatment for inflammatory joint conditions like rheumatoid arthritis, aiming to reduce inflammation and joint pain.
Other Emerging Applications
- Ongoing Research: The versatility of 177Lu allows for ongoing research into its application in other types of cancers and potentially non-oncological conditions.
- Customised Therapeutics: Future developments may lead to customised therapeutic regimens based on the specific characteristics of a patient’s disease, enhancing the effectiveness of treatment.
The use of lutetium radiopharmaceuticals, especially 177Lu, represents a significant advancement in the treatment of a range of diseases, particularly challenging cancers. These therapies provide a valuable option for patients with advanced or treatment-resistant forms of cancer, offering a targeted approach that can improve quality of life and survival rates. As research progresses, the scope of diseases treatable by lutetium radiopharmaceuticals is expected to widen, further cementing their role in modern therapeutic strategies.
Case Studies and Clinical Trial Results for Lutetium Radiopharmaceuticals
Lutetium-177 radiopharmaceuticals have been the focus of several clinical trials and case studies, particularly in the treatment of neuroendocrine tumours (NETs) and prostate cancer. These studies provide valuable insights into the efficacy, safety, and potential of 177Lu in targeted cancer therapy. Below are summaries of key clinical trials and case studies:
Neuroendocrine Tumours (NETs)
- NETTER-1 Trial: A pivotal phase III clinical trial for 177Lu-DOTATATE (Lutathera) in the treatment of advanced midgut NETs.
- Results: The trial significantly improved progression-free survival compared to high-dose octreotide LAR, a standard treatment for NETs. There was also a promising trend towards improved overall survival.
- Impact: Based on this trial, 177Lu-DOTATATE was approved by regulatory agencies like the FDA and EMA for the treatment of somatostatin receptor-positive NETs.
Prostate Cancer
- PSMA-617 Trials: Several trials are exploring the efficacy of 177Lu-PSMA-617 in metastatic castration-resistant prostate cancer (mCRPC).
- Preliminary Results: Early results have shown a significant reduction in PSA levels and a positive impact on overall survival and quality of life.
- Ongoing Studies: These trials are crucial in determining the optimal dosing, safety profile, and long-term benefits of 177Lu-PSMA-617 in prostate cancer.
Individual Case Studies
- Case Reports: Multiple case reports have documented the success of 177Lu radiopharmaceuticals in individual patients.
- Examples: Cases where patients with advanced NETs or mCRPC showed remarkable responses, significantly reducing tumour size and improving symptoms.
- Insights: These reports provide real-world evidence of the potential benefits and challenges of using 177Lu-based therapies.
Bone Metastases
- Pain Palliation Studies: Clinical studies have evaluated the effectiveness of 177Lu radiopharmaceuticals in palliating pain due to bone metastases.
- Findings: Results indicate significant pain relief in a substantial proportion of patients with a favourable safety profile.
Other Emerging Applications
- Early Phase Trials: Research is also being conducted on the use of 177Lu in other cancers, such as lymphomas and ovarian cancer, with some early phase trials showing encouraging results.
Long-Term Efficacy and Safety
- Follow-Up Studies: Long-term follow-up studies are essential to assess the prolonged efficacy, potential late side effects, and overall survival benefits of 177Lu therapies.
The clinical trials and case studies for Lutetium radiopharmaceuticals have been instrumental in establishing their role in cancer treatment. Particularly for NETs and prostate cancer, these studies have provided compelling evidence of the benefits of 177Lu-based therapies. As more data emerge from ongoing trials and real-world use, the scope of Lutetium radiopharmaceuticals in oncology is likely to expand, potentially offering new hope to patients with difficult-to-treat cancers.
Detailed Discussion on Lutetium-Based Drugs: A Focus on Lutathera
Lutathera, a prominent example of a lutetium-177 based drug, has garnered significant attention in the field of nuclear medicine for its efficacy in treating certain types of neuroendocrine tumours (NETs). Below is a detailed discussion of Lutathera, including its mechanism of action, usage, and clinical significance.
Overview of Lutathera
- Generic Name: Lutetium Lu-177 dotatate
- Brand Name: Lutathera
- Approval: It was approved by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for clinical use.
- Indication: Lutathera is indicated for the treatment of somatostatin receptor-positive gastroenteropancreatic neuroendocrine tumours (GEP-NETs), including those in the pancreas and gastrointestinal tract.
Mechanism of Action
- Targeting Strategy: Lutathera consists of a radionuclide (177Lu) attached to dotatate, a somatostatin analogue. Somatostatin receptors are commonly overexpressed in NETs.
- Radiation Delivery: Once administered, Lutathera binds to these receptors, and the 177Lu component delivers targeted beta radiation directly to the tumour cells, causing cellular damage and death.
Administration and Dosage
- Method of Administration: Lutathera is administered intravenously.
- Dosage Regimen: The typical treatment involves four doses, each administered approximately eight weeks apart. However, the regimen can be adjusted based on patient response and tolerance.
Efficacy and Clinical Trials
- NETTER-1 Trial: A pivotal phase III clinical trial demonstrated that Lutathera significantly improved progression-free survival compared to high-dose octreotide LAR in patients with advanced midgut NETs.
- Overall Survival Benefit: While initial data showed a strong trend towards improved overall survival, long-term follow-up studies are ongoing to establish definitive survival benefits.
Side Effects and Safety Profile
- Common Side Effects: These include nausea, vomiting, fatigue, and a temporary decrease in blood cell counts.
- Serious Concerns: Kidney toxicity and bone marrow suppression are serious potential side effects. Pre- and post-therapy measures, including renal protection protocols, are essential to mitigate these risks.
Patient Selection and Monitoring
- Eligibility Criteria: Patients with somatostatin receptor-positive NETs are considered eligible for Lutathera therapy. Imaging studies, like a gallium-68 dotatate PET/CT scan, are used to confirm receptor positivity.
- Monitoring: Regular monitoring is necessary to assess therapy response and detect any adverse effects. This includes blood tests, renal function tests, and imaging studies.
Future Directions and Research
- Expanding Indications: Ongoing trials are exploring the use of Lutathera in other types of NETs and in combination with other therapies.
- Research in Dosimetry: Studies are also focused on personalised dosimetry to optimise the radiation dose delivered to the tumours while minimising exposure to healthy tissues.
Lutathera represents a significant advancement in the treatment of neuroendocrine tumours, offering a new line of therapy for patients with advanced disease. Its approval and success underscore the potential of targeted radiopharmaceuticals in oncology. The ongoing research and development in this field are expected to further enhance the efficacy and safety profile of Lutathera and expand its applications in cancer treatment.
Administration Procedures and Dosing for Lutetium Radiopharmaceuticals
The administration of lutetium radiopharmaceuticals, especially lutetium-177 based therapies like Lutathera, involves specific procedures and dosing protocols to ensure both efficacy and safety. Here’s an overview of the typical administration and dosing procedures for these treatments:
Pre-Administration Assessment
- Patient Eligibility: Ensure patients meet the criteria for treatment, such as confirming the presence of somatostatin receptor-positive tumours for Lutathera.
- Baseline Assessments: Conduct baseline evaluations, including renal function tests, haematological assessments, and imaging studies.
Preparation for Administration
- Radiopharmaceutical Handling: Due to the radioactive nature of 177Lu, the preparation and handling of the drug must be performed by trained personnel in designated radiopharmacy facilities.
- Radiation Safety: Adherence to radiation safety guidelines is essential to protect healthcare personnel and patients from unnecessary radiation exposure.
Premedication
- Renal Protection: For drugs like Lutathera, amino acid solutions are administered intravenously before and after the radiopharmaceutical to protect the kidneys from radiation.
- Anti-emetics: Administer anti-emetic medication to prevent or reduce nausea and vomiting.
Radiopharmaceutical Administration
- Intravenous Infusion: Lutetium radiopharmaceuticals are typically administered via intravenous infusion.
- Monitoring: Continuous monitoring of the patient is required during the infusion for any adverse reactions
Dosing
- Standard Dosing for Lutathera: The typical dosing regimen for Lutathera involves 4 administrations, each providing 7.4 GBq (200 mCi) of 177Lu, administered every 8 weeks.
- Individual Adjustments: Dosing may be adjusted based on the patient’s response and tolerance to the treatment.
Post-Administration Care
- Hydration: Encourage patients to stay well-hydrated post-infusion to aid in the elimination of the radiopharmaceutical.
- Radiation Precautions: Patients may need to follow specific radiation safety precautions post-treatment to minimise radiation exposure to family members and the public.
Follow-Up and Monitoring
- Routine Assessments: Regular follow-up is required to monitor the effectiveness of the treatment and to check for any delayed adverse effects.
- Renal and Hematological Monitoring: Particular attention should be paid to renal function and blood counts during follow-up visits.
Documentation and Compliance
- Treatment Record: Maintain detailed records of each treatment, including dosing, administration details, and patient responses.
- Regulatory Compliance: Ensure compliance with all regulatory requirements related to the handling, administration, and disposal of radioactive materials
The administration of lutetium radiopharmaceuticals is a complex process that requires careful planning, specialised handling, and strict adherence to safety protocols. The standardisation of dosing and administration procedures, along with diligent patient monitoring, is crucial to maximising the therapeutic benefits of these treatments while minimising potential risks and side effects. As experience with these therapies grows, refinements in administration and dosing protocols continue to evolve, enhancing patient care and treatment outcomes.
Potential Side Effects and Risks Associated with Lutetium Radiopharmaceuticals
Lutetium radiopharmaceuticals, particularly those containing lutetium-177, have been a significant advancement in treating specific cancers. However, like all medical treatments, they come with potential side effects and risks. Understanding these is crucial for patient management and informed consent.
Haematological Toxicity
- Bone Marrow Suppression: 177Lu therapies can cause a reduction in blood cell counts, including white blood cells, red blood cells, and platelets, leading to an increased risk of infections, anaemia, and bleeding.
- Monitoring: Regular blood tests are required to monitor blood counts, and management may include supportive care like growth factor administration or blood transfusions.
Renal Toxicity
- Kidney Damage: The kidneys can be affected because they are involved in the excretion of the radiopharmaceutical. This can lead to a decrease in kidney function over time.
- Preventive Measures: Hydration and co-infusion with amino acids are standard practices to reduce renal uptake and mitigate the risk of renal toxicity.
Gastrointestinal Effects
- Nausea and Vomiting: These are common side effects, often manageable with anti-emetic medications.
- Other GI Issues: Diarrhea, abdominal pain, and constipation may also occur.
Xerostomia (Dry Mouth)
- 177Lu therapies, especially those targeting somatostatin receptors, can affect the salivary glands, leading to reduced saliva production and dry mouth.
Radiation Exposure Risks
- External Exposure: There is a risk of radiation exposure to family members and healthcare providers, although this is usually low and manageable with appropriate safety measures.
- Radiation Safety Guidelines: Patients are usually advised to follow specific guidelines to minimise radiation exposure to others, especially after treatment.
Secondary Malignancies
- While rare, exposure to radiation from radiopharmaceuticals carries a long-term risk of inducing secondary cancers.
Allergic Reactions
- As with any drug, there is a potential for allergic reactions to the components of the radiopharmaceutical, though this is relatively uncommon.
Reproductive Health
- Fertility: There may be an impact on fertility, and patients of reproductive age should discuss fertility preservation options.
- Pregnancy: Radiopharmaceuticals are contraindicated during pregnancy due to the risk of radiation to the fetus.
The side effects and risks associated with Lutetium radiopharmaceuticals require careful consideration and management. Regular monitoring and supportive care are essential components of the treatment process. Despite these risks, for many patients, the benefits of 177Lu therapy, particularly in terms of improved quality of life and survival in difficult-to-treat cancers, can outweigh the potential side effects. As with any cancer therapy, patient education and informed decision-making are key to ensuring the best possible outcomes.
Patient Monitoring and Safety Protocols for Lutetium Radiopharmaceuticals
When administering Lutetium radiopharmaceuticals, especially lutetium-177 based therapies like Lutathera, it’s crucial to implement rigorous patient monitoring and safety protocols. These measures are designed to maximise treatment efficacy, minimise side effects, and ensure the safety of both patients and healthcare providers.
Pre-Treatment Evaluation
- Assessment of Eligibility: Confirm the patient’s suitability for 177Lu therapy, including verifying the presence of somatostatin receptor-positive tumours if using Lutathera.
- Baseline Health Check: Evaluate renal function, blood counts, and liver function. Perform cardiac assessment if necessary.
During treatment
- Continuous Monitoring: Monitor vital signs (blood pressure, heart rate, oxygen saturation) during the infusion to detect any immediate adverse reactions.
- Hydration: Ensure adequate hydration before, during, and after the administration to facilitate radiopharmaceutical excretion and protect the kidneys.
- Radiation Safety: Follow strict radiation safety protocols to minimise exposure to medical staff and others.
Post-Treatment Monitoring
- Short-term Follow-up: Monitor for acute side effects like nausea, vomiting, and allergic reactions immediately after administration.
- Long-term Monitoring: Regular follow-up appointments to monitor for delayed effects like renal dysfunction or bone marrow suppression. This includes periodic blood tests, renal function tests, and imaging studies.
Haematological Monitoring
- Blood Counts: Regular blood tests to monitor for bone marrow suppression, a common side effect of radiopharmaceutical therapy.
- Management of Anemia or Neutropenia: If necessary, implement supportive care, including growth factors or blood transfusions.
Renal Function Monitoring
- Regular Assessment: Periodic assessment of renal function since 177Lu therapies can potentially impair kidney function over time.
- Renal Protective Measures: Continuing hydration and amino acid infusion protocols post-treatment as needed.
Radiation Safety for Patients and Families
- Post-therapy Precautions: Educate patients about radiation safety measures post-treatment, such as using separate bathrooms, avoiding close contact with others, and specific guidelines for pregnant women or those with young children.
- Waste Management: Instruct patients on the safe disposal of bodily fluids and materials that may be contaminated with radioactivity for a certain period post-treatment.
Managing Long-term Side Effects
- Regular Check-ups: Long-term follow-up to monitor for any signs of secondary cancers or other delayed side effects.
- Supportive Care: Addressing issues like xerostomia (dry mouth) and fatigue with appropriate interventions.
Psychological Support
- Emotional and Psychological Care: Providing psychological support to help patients cope with the stress and anxiety that can accompany cancer treatment
Patient monitoring and safety protocols are integral to the successful use of Lutetium radiopharmaceuticals. These protocols ensure not only the effective and safe administration of the therapy but also address the patient’s holistic needs, encompassing both physical and psychological aspects. Regular monitoring, adherence to safety guidelines, and prompt management of side effects are key components in optimising patient outcomes and ensuring the highest standards of care in nuclear medicine treatments.
Overview of the Regulatory Landscape for Lutetium Radiopharmaceuticals
The regulatory landscape for lutetium radiopharmaceuticals, particularly those involving lutetium-177, is a critical aspect that governs their development, approval, and clinical use. Stringent regulations and guidelines shape this landscape to ensure these advanced therapies’ safety, efficacy, and quality.
Regulatory Agencies
- U.S. Food and Drug Administration (FDA): In the United States, the FDA oversees the approval and regulation of radiopharmaceuticals, including those based on 177Lu.
- European Medicines Agency (EMA): In the European Union, the EMA is responsible for evaluating and supervising medicinal products.
- Other National and Regional Authorities: Each country or region has a regulatory body governing the approval and use of radiopharmaceuticals.
Regulatory Approval Process
- Clinical Trials: Radiopharmaceuticals must undergo rigorous clinical trials to demonstrate their safety and efficacy. These trials are typically conducted in multiple phases, including assessments of dosage, safety, efficacy, and comparison with standard treatments.
- Application for Approval: Following successful clinical trials, a manufacturer submits an application for regulatory approval, providing detailed data on clinical trials, manufacturing processes, quality controls, and proposed labelling.
- Review and Approval: Regulatory agencies thoroughly review the submission to ensure the product meets the required standards for safety and effectiveness.
Quality and Manufacturing Standards
- Good Manufacturing Practice (GMP): Radiopharmaceuticals must be manufactured in accordance with GMP standards to ensure their quality and safety.
- Radiation Safety: Additional regulations govern the handling, storage, and disposal of radioactive materials to protect healthcare workers, patients, and the environment.
Recent Approvals and Ongoing Clinical Trials
- Lutathera Approval: One of the most significant recent approvals is lutetium-177 dotatate (Lutathera), approved by the FDA and EMA for the treatment of somatostatin receptor-positive gastroenteropancreatic neuroendocrine tumours (GEP-NETs).
- Expanding Indications: Ongoing trials are exploring the use of Lutathera and other 177Lu-based drugs in different types of cancers and in combination with other treatments.
- New Developments: Research and trials are also focused on developing new 177Lu-labelled compounds for various oncological and non-oncological indications.
Future Directions
- Personalised Medicine: There is a growing emphasis on personalised medicine approaches, where radiopharmaceuticals are tailored to individual patient profiles for maximum efficacy.
- International Collaboration: Harmonisation of regulatory standards across different countries can facilitate the global development and accessibility of these treatments.
The regulatory landscape for lutetium radiopharmaceuticals is complex and evolving, with stringent requirements ensuring the safety and efficacy of these advanced therapies. As the field grows, with new products and indications emerging, regulatory frameworks will continue to adapt, balancing the need for rigorous oversight with the potential of these innovative treatments to significantly impact patient care. The progress in clinical trials and recent approvals mark an exciting era in developing and applying Lutetium-based therapies in medicine.
Research Advancements in Lutetium Radiopharmaceuticals
The field of lutetium radiopharmaceuticals, particularly those based on lutetium-177, has seen significant research advancements in recent years. These developments are improving current therapeutic options and paving the way for new applications.
Enhanced Targeting Mechanisms
- Improved Ligands: Research is focused on developing new ligands that can more effectively target specific types of cancer cells, increasing the efficacy of 177Lu therapies.
- Dual-Targeting Systems: There’s growing interest in creating dual-targeting systems that can simultaneously target different receptors on cancer cells, potentially increasing treatment effectiveness.
Combination Therapies
- Synergistic Approaches: Studies are exploring the use of 177Lu radiopharmaceuticals in combination with other treatments, such as chemotherapy, immunotherapy, or targeted therapy, to enhance overall treatment efficacy.
- Radiosensitisers: Incorporating radiosensitisers, which make cancer cells more sensitive to radiation, is another area of exploration.
Personalised Treatment Protocols
- Individualised Dosimetry: Efforts are underway to develop personalised dosimetry protocols, where the dose of radiopharmaceutical is tailored to the individual patient’s metabolism and tumour characteristics.
- Theranostics: This approach combines therapeutic and diagnostic capabilities in a single agent, allowing for personalised treatment monitoring and adjustments.
Expanding Indications
- Beyond NETs and Prostate Cancer: Research is expanding into using 177Lu for other types of cancers, including breast, ovarian, and certain types of brain tumours.
- Non-Oncological Uses: There’s also interest in exploring the potential of 177Lu in treating non-oncological conditions, such as certain types of chronic inflammatory diseases.
Future Potential and Emerging Trends
New Radiopharmaceuticals
- Innovative Compounds: Ongoing research is likely to yield new 177Lu-labelled compounds with improved targeting, reduced side effects, and enhanced efficacy.
- Radiopharmaceuticals for Rare Cancers: There’s potential for developing treatments for rare or hard-to-treat cancers, offering new hope to patients with limited options.
Advances in Imaging and Diagnosis
- Improved Imaging Techniques: Advancements in imaging technologies, such as PET/CT, can enhance the diagnostic accuracy of 177Lu therapies, leading to better treatment planning and monitoring.
- Molecular Imaging: The development of novel imaging agents that can precisely visualise disease processes at the molecular level will further refine the use of 177Lu therapies.
Global Accessibility
- Production and Distribution: Efforts are being made to improve the production and distribution of 177Lu, making these therapies more accessible worldwide.
- Regulatory Harmonisation: Harmonising regulatory requirements across different regions could facilitate the global development and approval of new treatments.
Multidisciplinary Collaboration
- Integrated Approaches: Collaboration between nuclear medicine, oncology, radiology, and other disciplines is crucial for the advancement of 177Lu radiopharmaceuticals.
- Patient-Centric Care: A focus on patient-centred approaches in research and clinical application will drive advancements that directly address patient needs and outcomes.
The field of Lutetium radiopharmaceuticals is at an exciting juncture, with research advancements opening new avenues in cancer treatment and beyond. The combination of innovative targeting mechanisms, personalised treatment protocols, and multidisciplinary collaboration holds significant promise for the future, potentially revolutionising the way certain diseases are treated. As the research progresses, these emerging trends are expected to significantly impact patient care, offering more effective and tailored treatment options.
Summary of the Impact of Lutetium Radiopharmaceuticals in Medicine
The introduction and development of Lutetium radiopharmaceuticals, particularly those based on lutetium-177, have marked a significant milestone in the field of nuclear medicine and oncology. Their impact is multifaceted, addressing both diagnostic and therapeutic needs.
Therapeutic Advancements
- Targeted Cancer Therapy: 177Lu-based drugs like Lutathera have revolutionised the treatment of certain neuroendocrine tumours (NETs) and prostate cancer, providing effective options where traditional therapies have limited success.
- Reduced Side Effects: By targeting specific cancer cells, these treatments minimise damage to healthy tissues, reducing side effects compared to conventional radiotherapy or chemotherapy.
Diagnostic Contributions
- Improved Imaging: The use of 177Lu in diagnostic imaging has enhanced the ability to accurately diagnose, stage, and monitor the progression of certain cancers.
- Theranostics: The dual role of 177Lu in both therapy and diagnostics (theranostics) allows for more personalised and effective treatment plans.
Quality of Life
- Symptom Management: These treatments have been instrumental in improving symptoms and quality of life for patients with advanced cancers, particularly those suffering from pain due to metastases.
Future Outlook
Expansion of Indications
- Broader Cancer Types: Ongoing research is likely to extend the use of 177Lu radiopharmaceuticals to a wider range of cancers, including breast, ovarian, and certain types of brain tumours.
Technological and Research Advancements
- Innovative Compounds: The development of new 177Lu-labelled compounds is expected to improve targeting efficiency and reduce side effects.
- Advanced Imaging Techniques: Improvements in imaging technologies will enhance the diagnostic precision of 177Lu therapies, leading to better patient outcomes.
Personalised Medicine
- Customised Treatment Protocols: The move towards personalised medicine, including individualised dosing and treatment regimens based on patient-specific factors, is anticipated to increase the efficacy of 177Lu therapies.
- Integrated Patient Care: Enhanced collaboration between different medical specialties will foster a more holistic approach to patient care.
Global Accessibility
- Increased Production and Distribution: Efforts to streamline the production and distribution of 177Lu will make these therapies more accessible globally.
- Regulatory Harmonisation: Efforts to standardise regulatory processes internationally could expedite the approval and availability of new treatments.
Conclusion
Lutetium radiopharmaceuticals have significantly impacted the landscape of medical treatment, particularly in the realm of cancer therapy. Their future in medicine looks promising, with ongoing advancements poised to broaden their applications, improve patient outcomes, and integrate them more seamlessly into personalised treatment protocols. As research and technology continue to advance, the full potential of lutetium radiopharmaceuticals in improving patient care and treatment options will likely be realised.
You are here: home » medical imaging blog »