Lead radiopharmaceuticals are transforming oncology by offering precise, potent cancer therapies with reduced adverse effects.
Targeted Cancer Therapy
Radiopharmaceuticals have seen remarkable progress in recent years, with advances in nuclear medicine facilitating improved diagnosis and more effective therapies. New radiopharmaceuticals are being developed alongside efficient production methods for relevant radioisotopes. High-energy and high-current accelerators are now available for radioisotope production, broadening access to several promising radionuclides, including Lead-212 (212Pb).
The table below summarises the key properties of Lead-212:
| Property | Description |
| Atomic Number | 82 |
| Mass Number | 212 |
| Half-Life | 10.64 hours |
| Decay Mode | Beta decay to Bismuth-212 (212Bi) |
| Atomic Mass | 211.9912857 u |
| Neutrons | 130 |
| Protons | 82 |
| Specific Activity | High due to its short half-life |
| Radiation Type | Emits beta particles and gamma radiation |
| Daughter Products | Bismuth-212 (212Bi), Polonium-212 (212Po) through the decay chain |
| Occurrence | Rare, usually produced in laboratories or as part of the Thorium decay series |
The radiopharmaceutical market, which was valued at around $4.8 billion in 2017, is expected to experience significant growth, reaching nearly $12 billion by 2030. This growth is driven by factors such as an ageing population, the increasing prevalence of chronic diseases, and technological advancements in imaging technologies.
This sector, which began with a single therapy (iodine-131) in the 1950s, marked a significant advancement in the field of nuclear medicine and the treatment of certain medical conditions, particularly thyroid disorders.
Today, various drugs have been designed to deliver tumour-killing radioactive payloads while sparing healthy cells. The integration of radiology and chemotherapy in radiopharma allows for greater specificity and more biomarker-driven management of patients.
One of the most promising areas in radiopharmaceutical development involves attaching radioligands to different modalities, like chimeric antigen receptor (CAR) T-cell therapy. This approach could offer new strategies to tackle some of oncology’s most significant challenges, including cancer resistance and metastases. The radiopharmaceutical pipeline is rapidly expanding, with a diverse array of therapeutic options being clinically tested and categorised by isotope.
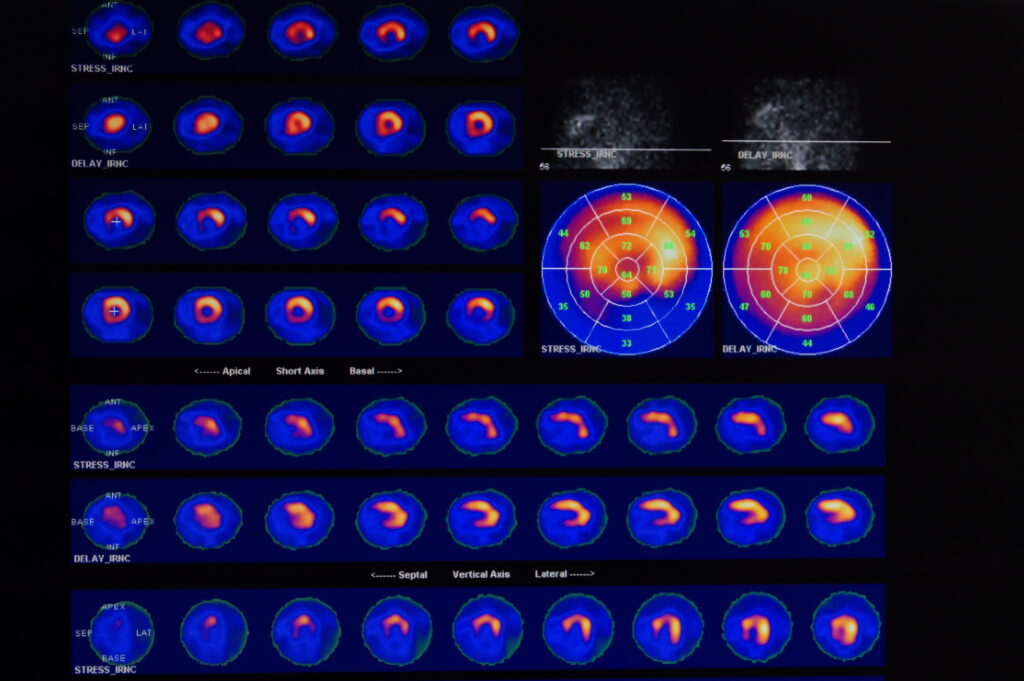
These developments demonstrate the evolving nature of radiopharmaceuticals, from simple radioiodine to complex coordination complexes of technetium-99m radiopharmaceuticals. The field now encompasses a variety of PET radioligands and therapeutic agents evaluated for potential clinical applications. This evolution includes novel radiochemistry methods for radiolabelling a variety of ligands with different radionuclides, automated process developments, and the availability of nonclinical evaluation techniques. The concept of theranostic radioisotopes, combining diagnostic and therapeutic properties, is a particularly exciting development for future medical applications of radionuclides.
In the corporate sphere, major pharmaceutical companies are actively investing in radiopharmaceuticals, recognising their potential to revolutionise the treatment of hard-to-treat cancers. Eli Lilly’s acquisition of POINT Biopharma, for instance, brought promising radioligand therapies targeting metastatic castration-resistant prostate cancer and gastroenteropancreatic neuroendocrine tumours under its umbrella. Similarly, Novartis AG’s contemplation to sell part of Advance Accelerator Applications, a radiopharmaceutical company, aligns with its strategy to focus on high-risk, high-reward business units.
Recent clinical trials using lead radiopharmaceuticals
Several clinical trials involving Lead-212 are currently underway or planned, focusing on its potential for treating various types of cancer through targeted alpha therapy (TAT):
- Phase 1 Trial of 212Pb-Pentixather Radioligand Therapy: This trial, scheduled to start in July 2024, focuses on patients with atypical lung carcinoids and neuroendocrine carcinomas. It aims to evaluate the safety of an alpha-radiation treatment using Lead-212 labelled Pentixather. The treatment involves two cycles of intravenous infusion of Pentixather radiolabelled with Lead-212, spaced six weeks apart. This study will determine the recommended phase 2 dose based on observed dose-limiting toxicities.
- Perspective Therapeutics Phase 1/2a Trials: Perspective Therapeutics has initiated two different trials. The first is a Phase 1/2a Dose Escalation of [212Pb]VMT-α-NET Targeted Alpha-Particle Therapy for Advanced SSTR2 Positive Neuroendocrine Tumors. The second trial is a Phase 1/2a Dose Escalation trial of [212Pb]VMT01 Targeted Alpha-Particle Therapy for patients with MC1R Positive unresectable and metastatic melanoma. Both trials explore the efficacy and safety of Lead-212-based therapies in targeting specific receptors on cancer cells.
- Orano Med’s Phase I Trial with 212Pb-GRPR: This is an ongoing trial evaluating the alpha radioligand therapy with Lead-212, [212Pb]Pb-GRPR, in patients with advanced solid tumours expressing gastrin-releasing peptide receptor (GRPR). This study focuses on prostate, lung, and breast cancers, which highly express GRPR. The trial includes a dose escalation phase and aims to evaluate the treatment’s safety, tolerability, and efficacy.
- 212Pb-DOTAMTATE for Metastatic Neuroendocrine Tumours: Another recent study at the University of Kentucky Markey Cancer Center highlights the potential of a new radiopharmaceutical compound, 212Pb-DOTAM-GRPR1, for treating advanced cervical cancer. This study suggests that the drug, which targets the gastrin-releasing peptide receptor (GRPR) expressed by cancer cells, may be useful in the treatment of persistent, recurrent, or metastatic cervical cancer. The evaluation of tissue from 33 tumours from women with metastatic cervical cancer showed that most of the tissue overexpressed GRPR, suggesting that 212Pb-DOTAM-GRPR1 is a promising therapy for this disease. This study validates a phase 1 clinical trial of 212Pb-DOTAM-GRPR1, marking a significant step forward in developing targeted cervical cancer treatments.
These trials represent a broader trend in the use of radiopharmaceuticals for targeted cancer therapy. Radiopharmaceuticals, which deliver radiation therapy directly to cancer cells, are increasingly seen as an important part of future cancer treatments. They offer the potential for more effective treatment outcomes with reduced side effects compared to traditional radiation therapy. The development and clinical validation of these new agents are crucial steps in bringing advanced therapies to the oncology market and offer hope for improved treatment options for patients with hard-to-treat cancers.
A brief history of lead radiopharmaceuticals
The history of lead radiopharmaceuticals used in theranostics – a field combining therapy and diagnostics – is a fascinating journey of scientific advancement and clinical innovation. It intertwines the development of nuclear medicine, radiopharmaceutical technology, and the evolving understanding of cancer biology.
Early Foundations
- 1950s-1960s: The roots of theranostics can be traced back to the mid-20th century with the advent of nuclear medicine. The initial focus was on diagnostics, primarily using iodine isotopes for thyroid imaging and therapy.
- 1970s-1980s: The concept of using radiolabelled antibodies for cancer detection emerged, laying the groundwork for targeted therapy. These decades saw significant advances in radiochemistry and imaging technologies, leading to the first generation of radiolabelled agents.
The Emergence of Lead Radiopharmaceuticals
- Late 1980s-1990s: Scientists began exploring various radionuclides for therapeutic purposes. Lead isotopes, particularly lead-212 (Pb-212), gained attention due to their favourable properties, such as appropriate half-life and decay characteristics for targeting tumours.
- 2000s: The first experimental therapies using lead radiopharmaceuticals were initiated. Researchers focused on Pb-212 because of its emission of short-range, high-energy alpha particles, making it ideal for killing cancer cells while minimising damage to surrounding healthy tissues.
Conclusion
Lead radiopharmaceuticals represent a significant breakthrough in the field of nuclear medicine and theranostics, offering a novel and promising approach to cancer treatment. The unique properties of lead isotopes, particularly their ability to emit high-energy alpha particles, make them highly effective in targeting and destroying cancer cells while minimising damage to surrounding healthy tissues.
The development of lead radiopharmaceuticals has been marked by a series of clinical trials and research efforts, demonstrating their potential in treating various types of cancers, including prostate and cervical cancers. These trials have shown the efficacy of these treatments in reducing tumour size and growth and their tolerability, with fewer side effects compared to traditional radiation therapies.
Moreover, the integration of lead radiopharmaceuticals into theranostic strategies has opened new horizons in personalised medicine. Combining diagnostic and therapeutic capabilities allows for more precise targeting of cancer cells, leading to more effective and customised treatment regimens.
The ongoing research and development in this field are likely to yield further improvements in drug delivery systems, targeting mechanisms, and safety profiles. Regulatory advancements are also supporting the expedited evaluation and approval of these innovative treatments.
Lead radiopharmaceuticals stand at the forefront of a new era in cancer therapy, offering hope for more effective, targeted, and patient-friendly treatment options. Their continued development and refinement are essential in the fight against cancer, potentially transforming the landscape of oncological care.
Disclaimer
The content presented in this article is for informational and educational purposes only and does not constitute medical advice, diagnosis, or treatment recommendations. Open Medscience does not endorse or promote any specific treatment, pharmaceutical product, or clinical trial mentioned herein. All information provided, including references to clinical studies and medical technologies, is based on publicly available sources as of the publication date and may not reflect the most current research or regulatory status.
Readers are advised to consult qualified healthcare professionals for medical advice tailored to their individual circumstances. Any mention of ongoing clinical trials, investigational therapies, or company activities should not be interpreted as a guarantee of efficacy, safety, or future approval by regulatory bodies.
Open Medscience shall not be held responsible for any action taken or not taken based on the content of this publication. Reliance on any information provided in this article is solely at the reader’s own risk.
You are here: home » diagnostic medical imaging blog »