Magnetic Resonance Angiography (MRA) has emerged as a powerful, non-invasive imaging modality in the assessment of vascular diseases, particularly those involving the aorta and its major branches. As cardiovascular diseases continue to represent a significant burden worldwide, accurate and detailed imaging plays an essential role in diagnosis, treatment planning, and follow-up. MRA offers high-resolution vascular imaging without the need for ionising radiation, making it an increasingly preferred choice in clinical practice. This blog article explores the principles of MRA, its advantages, its role in the diagnosis and management of aortic diseases, and how it compares with other imaging modalities.
Introduction to Magnetic Resonance Angiography
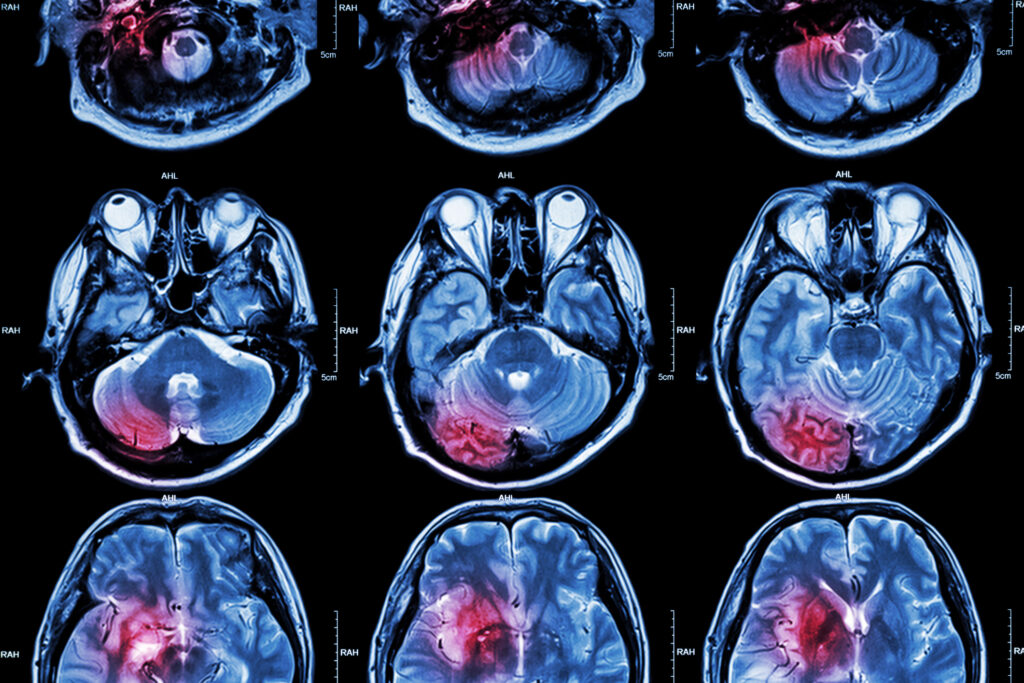
Magnetic Resonance Angiography is a specialised application of Magnetic Resonance Imaging (MRI) designed to visualise blood vessels. By exploiting the magnetic properties of hydrogen nuclei in the blood and using specific pulse sequences, MRA produces detailed images of the vascular system. It can be performed with or without contrast agents, typically gadolinium-based, which improve image clarity and diagnostic accuracy.
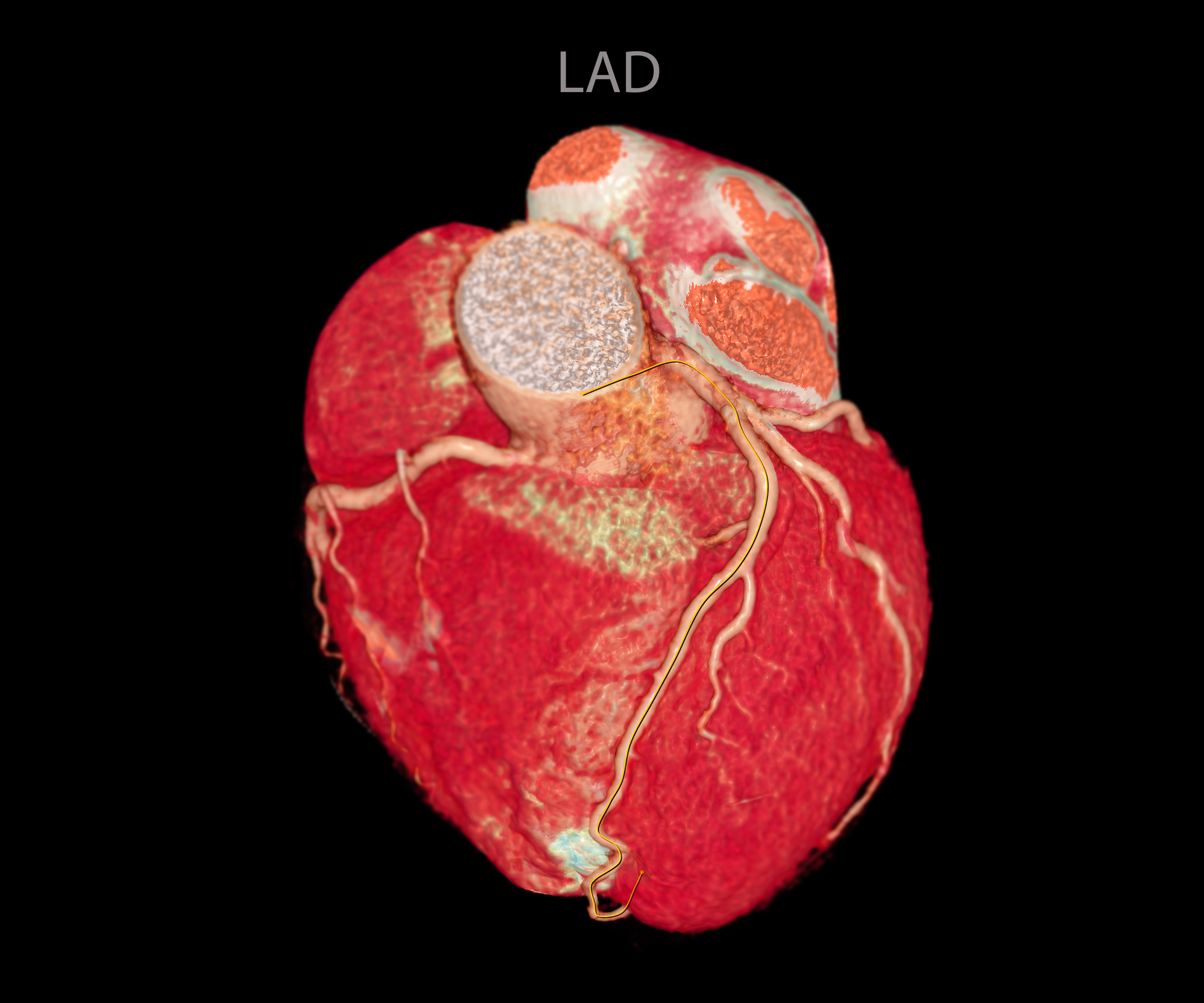
The ability of MRA to produce three-dimensional reconstructions of the vasculature allows clinicians to examine the anatomy and pathology of the aorta and its branches from multiple angles. Its non-invasive nature and absence of ionising radiation make it particularly suitable for younger patients, those requiring repeated imaging, and individuals with contraindications to iodinated contrast agents used in computed tomography angiography (CTA).
Anatomy of the Aorta and Its Branches
The aorta, the largest artery in the human body, originates from the left ventricle of the heart and distributes oxygenated blood to the systemic circulation. It is divided into four main segments: the ascending aorta, the aortic arch, the thoracic descending aorta, and the abdominal aorta. Each segment gives rise to important branches supplying vital organs and tissues.
From the ascending aorta emerge the coronary arteries, while the aortic arch gives rise to the brachiocephalic trunk, left common carotid artery, and left subclavian artery. The descending thoracic aorta provides branches to the intercostal spaces, and the abdominal aorta gives rise to major vessels, including the celiac trunk, superior and inferior mesenteric arteries, renal arteries, and iliac arteries. Given this complex anatomy and the crucial functions these vessels perform, diseases affecting the aorta and its branches can have serious clinical consequences.
Advantages of MRA in Aortic Imaging
MRA offers several advantages over other imaging techniques in the evaluation of aortic pathology. One of the most significant is the absence of ionising radiation, which is particularly important for younger patients and those requiring long-term follow-up. The use of gadolinium-based contrast agents also carries a lower risk of nephrotoxicity compared to iodinated contrast used in CT angiography, making MRA a safer option for patients with impaired renal function.
The ability of MRA to provide high-contrast, three-dimensional images of the vascular lumen and wall allows for precise assessment of both anatomical and pathological details. Furthermore, MRA can assess blood flow dynamics, enabling the detection of abnormalities such as turbulence, stenosis, and dissection. Another advantage is its superior soft tissue contrast, which facilitates the evaluation of perivascular structures and associated complications such as haematomas, aneurysmal wall changes, and inflammatory processes.
MRA Techniques for Aortic Imaging
Several MRA techniques are used in clinical practice, each suited to specific diagnostic requirements. Time-of-flight (TOF) and phase-contrast (PC) MRA are non-contrast methods that exploit differences in blood flow to generate vascular images. These are particularly useful in patients with contraindications to gadolinium.
Contrast-enhanced MRA (CE-MRA) is the most widely used technique for imaging the aorta and its branches. It involves intravenous injection of a gadolinium-based contrast agent, followed by rapid image acquisition during the arterial phase. CE-MRA provides excellent visualisation of the aortic lumen and its branches with high spatial resolution. Techniques such as time-resolved imaging further enhance the ability to capture dynamic blood flow and distinguish arterial from venous structures.
Role of MRA in Aortic Aneurysms
Aortic aneurysms are localised dilatations of the aorta that pose a risk of rupture, a life-threatening event. MRA plays an important role in the diagnosis, characterisation, and monitoring of aneurysms. It accurately measures the size, shape, and extent of the aneurysm, providing essential information for surgical or endovascular planning.
MRA can assess the involvement of branch vessels, mural thrombus formation, and changes in aneurysm size over time. In patients undergoing endovascular aneurysm repair (EVAR), MRA is valuable for post-procedural surveillance, enabling the detection of complications such as endoleaks without exposure to radiation.
Evaluation of Aortic Dissection with MRA
Aortic dissection, characterised by a tear in the intimal layer of the aorta allowing blood to enter the media and create a false lumen, is a medical emergency requiring prompt diagnosis. MRA is highly effective in detecting and classifying dissections, delineating the true and false lumens, and identifying the site of the intimal tear.
The high contrast and multiplanar capabilities of MRA allow for precise visualisation of branch vessel involvement, extension of the dissection, and potential complications such as aortic rupture or organ malperfusion. Moreover, functional imaging sequences can assess flow patterns within the true and false lumens, providing insights into haemodynamic consequences and guiding treatment decisions.
Assessment of Aortic Coarctation and Congenital Anomalies
MRA is particularly valuable in the evaluation of congenital aortic anomalies, such as coarctation of the aorta, interrupted aortic arch, and vascular rings. Its ability to produce detailed anatomical maps without radiation exposure is especially beneficial in paediatric and young adult populations.
In coarctation of the aorta, MRA not only identifies the site and severity of narrowing but also evaluates collateral circulation and associated cardiovascular anomalies. Post-surgical follow-up is another area where MRA excels, allowing for non-invasive monitoring of repair sites and detection of restenosis.
Role in Atherosclerotic and Occlusive Disease
Atherosclerosis affecting the aorta and its branches can lead to stenosis, occlusion, and downstream ischaemic complications. MRA is capable of detecting and characterising atherosclerotic plaques, assessing the degree of stenosis, and evaluating its impact on blood flow. It can also visualise thrombi, ulcerated plaques, and wall thickening, providing information relevant to both diagnosis and treatment planning.
MRA’s ability to image branch vessels such as the renal, mesenteric, and iliac arteries makes it valuable in identifying stenotic disease that may contribute to conditions like renovascular hypertension, mesenteric ischaemia, or peripheral arterial disease.
Comparison with Other Imaging Modalities
While CTA and conventional catheter angiography remain widely used, MRA offers several advantages in specific clinical contexts. CTA provides rapid acquisition and excellent spatial resolution but involves ionising radiation and iodinated contrast, limiting its use in certain patients. Catheter angiography, though still considered a gold standard for interventional planning, is invasive and carries procedural risks.
MRA, by contrast, is non-invasive, radiation-free, and suitable for repeated use, with excellent diagnostic accuracy for most aortic pathologies. However, limitations include longer acquisition times, susceptibility to motion artefacts, and contraindications in patients with certain metallic implants or severe renal dysfunction, where gadolinium use is restricted.
Future Directions and Technological Advancements
Recent advances in MRI technology continue to enhance the diagnostic capabilities of MRA. Techniques such as four-dimensional flow (4D flow) MRA allow for a comprehensive assessment of blood flow patterns and wall shear stress, offering new insights into the pathophysiology of aortic diseases. Improvements in spatial and temporal resolution, along with the development of non-contrast imaging techniques, are expanding the applicability of MRA in broader patient populations.
Artificial intelligence and machine learning are also being integrated into MRA image analysis, enabling automated detection and characterisation of vascular pathology and improving diagnostic accuracy. As these technologies evolve, MRA is expected to become an even more powerful tool in the evaluation of aortic diseases.
Conclusion
Magnetic Resonance Angiography has established itself as a key imaging modality in the evaluation of diseases of the aorta and its branches. Its ability to provide detailed, three-dimensional visualisation of vascular anatomy and pathology without ionising radiation offers significant advantages over traditional imaging methods. From the diagnosis of aneurysms and dissections to the assessment of congenital anomalies and atherosclerotic disease, MRA provides comprehensive information crucial for clinical decision-making.
With ongoing technological advancements and the integration of functional and quantitative imaging techniques, MRA is poised to play an increasingly central role in the diagnosis, management, and follow-up of aortic diseases, ultimately improving patient outcomes and advancing cardiovascular care.
Disclaimer
The information provided in this article is intended for general educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be relied upon as a substitute for consultation with qualified healthcare professionals. Magnetic Resonance Angiography (MRA) and other diagnostic imaging techniques should be considered and interpreted by trained medical practitioners within the context of a patient’s individual clinical circumstances. Open MedScience does not endorse any specific medical procedures, products, or treatment plans mentioned herein and accepts no responsibility for any decisions made based on the content of this article. Always seek the guidance of a qualified healthcare provider with any questions you may have regarding a medical condition.