Summary: Robotic neurosurgery is reshaping the way surgical interventions are performed on the brain and spine, offering enhanced precision, minimally invasive techniques, and improved clinical outcomes. This article provides a detailed exploration of the development and application of robotic systems in neurosurgery, assessing their benefits, limitations, and future potential. Through an examination of real-world cases, technological evolution, and clinical impact, it outlines the role robotic neurosurgery is playing in transforming the landscape of neurological care.
Keywords: Neurosurgery, Robotics, Brain surgery, Spinal surgery, Surgical accuracy, Minimally invasive
Historical Development and Key Technological Milestones
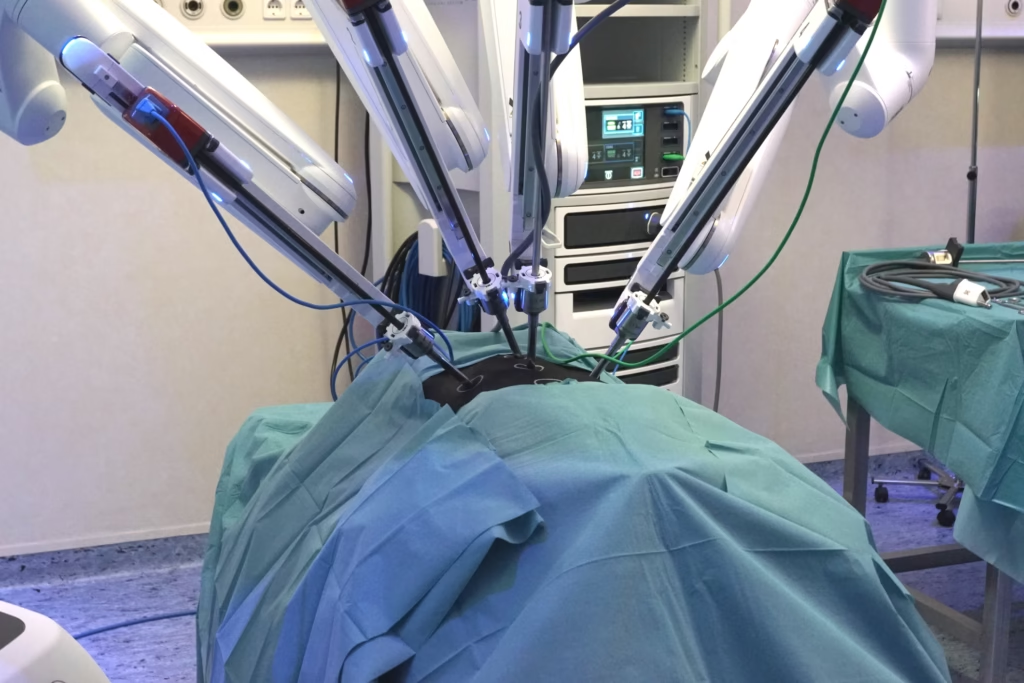
In recent years, the fusion of robotics with neurosurgery has led to a quiet revolution in operating theatres worldwide. Neurosurgical procedures are amongst the most delicate and high-stakes in all of medicine, given the complexity and critical functions of the central nervous system. The introduction of robotic systems into this field has allowed for surgical interventions that are more precise, less invasive, and often associated with faster recovery and fewer complications.
Although robotics has been used in surgery since the 1980s, its application in neurosurgery required more refined and responsive technology. The progress of imaging, computational power, artificial intelligence (AI), and sensor integration has now made robotic neurosurgery not only feasible but increasingly common in leading hospitals.
The first use of robotic systems in surgery was primarily focused on fields such as urology and orthopaedics. Neurosurgery followed later due to its unique demands for sub-millimetre accuracy. Early attempts involved rudimentary tools designed to assist with image guidance and basic positioning.
A breakthrough occurred in the early 2000s with systems such as NeuroArm, which introduced haptic feedback and MRI compatibility, enabling surgeons to operate with high precision while receiving tactile information. The development of robotic platforms, such as ROSA (Zimmer Biomet) and the Mazor X (Medtronic), soon followed, offering solutions tailored specifically to brain and spinal procedures.
Today’s robotic systems integrate seamlessly with high-resolution imaging, planning software, and surgeon-controlled robotic arms capable of extraordinarily fine movements. The combination of these elements supports not only complex procedures but also offers improved consistency and safety.
How Robotic Neurosurgery Operates
Robotic neurosurgery relies on a suite of interlinked technologies designed to enhance the surgeon’s capability without replacing them. Key components include:
1. Robotic Arms
These instruments, guided by the surgeon, can perform complex movements with high stability and without the minor tremors that human hands may introduce. They are particularly valuable in microsurgery, where stability is paramount.
2. Imaging Systems
Modern robotic platforms are heavily reliant on MRI and CT data, often obtained in real-time during surgery. This ensures that surgeons can visualise structures in fine detail and track progress as they operate.
3. Planning and Navigation Software
Software enables detailed preoperative planning, including trajectory mapping for tools and simulations of the procedure. During surgery, the same software provides intraoperative guidance, ensuring that the plan is followed with high accuracy.
4. Haptic Feedback and AI Integration
Some systems offer tactile feedback to replicate the feel of traditional surgery. AI is also being introduced to support decision-making and real-time adjustments during procedures.
Clinical Applications
Robotic systems are now used in a variety of neurosurgical procedures. The most common include:
Brain Tumour Resection: Robots assist surgeons in removing tumours while preserving healthy tissue, utilising real-time imaging and computer-guided paths. In procedures where millimetres can make the difference between cure and disability, robotic assistance is invaluable.
Deep Brain Stimulation (DBS): For conditions such as Parkinson’s disease, robotic platforms ensure electrodes are placed accurately within specific brain regions. Accurate placement is crucial for achieving effective symptom control and minimising side effects.
Spinal Fixation Surgery: Robotic systems assist in precisely placing screws and rods, reducing the need for large incisions and extensive dissection. This results in quicker recovery and less post-operative discomfort.
Epilepsy Surgery: Robots enable the targeted removal of seizure foci or the placement of diagnostic electrodes with significantly less disruption to surrounding brain tissue.
Stereotactic Biopsies and Procedures: Utilising robots for stereotactic neurosurgery enhances access to deep or otherwise challenging areas of the brain, enabling safe sampling or intervention with minimal risk.
Advantages of Robotic Neurosurgery
Greater Surgical Accuracy: One of the most cited benefits is the sub-millimetre accuracy that robots can achieve. This is crucial when operating near critical structures, such as blood vessels, motor cortex regions, or the brainstem.
Minimally Invasive Techniques: Smaller incisions result in less bleeding, a reduced risk of infection, and a faster recovery. This is particularly beneficial for patients with multiple comorbidities or limited physiological reserves.
Improved Patient Outcomes: Better accuracy and lower complication rates directly translate into improved outcomes, including reduced post-operative pain, shorter hospital stays, and higher overall satisfaction.
Reduced Surgeon Fatigue: Long operations can lead to physical strain. Robotics can reduce the burden by allowing more ergonomic working conditions and automating certain repetitive tasks.
Enhanced Training Opportunities: Simulation tools linked to robotic platforms enable trainees to practise on virtual patients, building skills and confidence without the risks associated with a live surgical environment.
Limitations and Ongoing Challenges
While promising, robotic neurosurgery is not without issues:
Cost and Maintenance: High initial investment, ongoing maintenance, and the need for specialised staff can be prohibitive. Smaller hospitals and public healthcare systems may struggle to justify these costs without significant external funding or demonstrable efficiency gains.
Training Requirements: Robotic systems require not only technical training but also a shift in surgical mindset. Teams must adapt to new workflows, and errors can occur during the learning curve.
Technology Dependence: Over-reliance on machines may dull manual surgical skills or create vulnerabilities if systems fail during procedures. Backup protocols must be robust and regularly rehearsed.
Ethical and Legal Questions: As robotics becomes more autonomous, questions of responsibility arise. Who is accountable in the event of error: the surgeon, the manufacturer, or the software provider?
Future Directions in Robotic Neurosurgery
The development of robotic neurosurgery is far from complete. Several trends are likely to shape its future:
Artificial Intelligence Integration: AI is being introduced to assist with real-time analysis, image interpretation, and even decision-making during surgery. This could further improve surgical precision and reduce errors.
Remote Surgery (Telesurgery): With fast, secure internet connections and remote control interfaces, it may become possible for expert surgeons to operate on patients in different locations, increasing access to specialist care.
Enhanced Sensory Feedback: Future systems may enhance the sensation of touch for the operating surgeon, thereby further improving safety and restoring a level of tactile perception that current systems currently lack.
Personalised Surgery: With the help of genomics, imaging, and AI, robotic neurosurgery could become tailored to the individual patient, using patient-specific data to guide surgical plans and interventions.
Conclusion
Robotic neurosurgery is no longer a futuristic idea but a tangible part of modern medicine. With clear advantages in precision, safety, and patient recovery, it offers a compelling case for adoption in many areas of neurosurgical practice. However, the technology also presents challenges in terms of cost, accessibility, and ethical complexity.
As robotic systems become more sophisticated and affordable, they are likely to become a standard tool in neurosurgical departments worldwide. The next decade may see even closer integration of AI, remote operation capabilities, and personalised surgical pathways—delivering care that is safer, faster, and more tailored to the individual patient than ever before.
Ultimately, robotic neurosurgery is not simply about machines replacing humans, but about technology enhancing what skilled professionals can achieve for their patients.
Disclaimer
The information provided in this article is intended for general educational and informational purposes only. Open Medscience does not offer medical advice, diagnosis, or treatment recommendations. The content reflects current knowledge and practices related to robotic neurosurgery at the time of publication and may not include the most recent developments. Readers should consult qualified healthcare professionals before making any decisions related to medical care or surgical options. The inclusion of specific technologies, systems, or companies does not constitute an endorsement by Open Medscience. While every effort has been made to ensure accuracy, Open Medscience accepts no responsibility for any loss, damage, or consequence arising from reliance on the information contained herein.