Summary: In recent years, alpha particle emitting radionuclides have gained attention for their potential to offer precise cancer control. By delivering strong but localised energy to malignant cells, these radionuclides can cause significant damage to tumour tissue while minimising harm to healthy cells. This article explores established alpha emitter options, their mechanisms of action, and their advantages compared to other forms of targeted radiation. Considerations such as chemical properties, production methods, and clinical outcomes are addressed, emphasising their suitability as a powerful class of therapeutic agent. Overcoming technical obstacles and ensuring each medical isotope’s safe distribution remain crucial in the field.
Keywords: radionuclide therapy; alpha emitter; targeted radiation; medical isotope; therapeutic agent; radiopharmaceutical.
Introduction to Alpha Particle Emission
Alpha particle emitting radionuclides are a special category of atomic species that hold significant promise in radionuclide therapy. An alpha emitter typically releases a helium-4 nucleus (composed of two protons and two neutrons) during its decay process, resulting in highly energetic particles that travel only a short distance in tissue. This short path length can focus radiation damage on specific targets while keeping collateral damage to surrounding healthy cells low. These alpha emitters can be delivered to malignant lesions through targeted radiation when bound to a suitable radiopharmaceutical.
For many years, research into alpha particle emitting radionuclides centred on both theoretical benefits and practical obstacles. However, emerging clinical data support the idea that these radionuclides can be a potent therapeutic agent for various cancers, including bone metastases and neuroendocrine tumours. As each medical isotope in this class carries unique properties, identifying the most suitable candidate for a given clinical indication is an ongoing challenge that involves production techniques, radiolabelling strategies, and toxicity profiles.
Key Alpha Emitters in Therapeutic Nuclear Medicine
Several alpha particle emitting radionuclides have been investigated for their suitability in radionuclide therapy. Among the most frequently studied are radium-223 (Ra-223), actinium-225 (Ac-225), thorium-227 (Th-227), and astatine-211 (At-211). Each alpha emitter has its decay properties, half-life, and chemical characteristics, affecting its production method and effectiveness as a therapeutic agent. Understanding these parameters is crucial when designing targeted protocols to deliver targeted radiation.
- Radium-223 received regulatory approval for the treatment of metastatic castration-resistant prostate cancer affecting bone. It targets osteoblastic lesions due to its similarity to calcium, thus becoming a potent radiopharmaceutical for bone disease. Ra-223 has a half-life of 11.4 days, which allows practical distribution and storage. Its decay leads to alpha emission that effectively destroys tumour cells, while its affinity for areas of increased bone turnover helps limit radiation exposure to healthy tissue.
- Actinium-225 has generated considerable interest for use in targeted therapies against leukaemia and solid tumours. One key advantage is its decay chain, which includes multiple alpha emissions, potentially enhancing its potency as a therapeutic agent. Researchers have explored radiolabelling Ac-225 to antibodies or peptides that bind tumour-associated antigens, providing site-specific targeted radiation. However, correctly handling this medical isotope is challenging since additional decay products must be managed to prevent unintended radiation to non-target organs.
- Thorium-227 has a half-life of 18.7 days, and Th-227 is also a promising alpha emitter. Similar to Ac-225, it can be attached to tumour-specific carriers, offering precise radionuclide therapy. A key consideration is controlling the retention of progeny isotopes produced during decay. Various chelating agents have been explored to keep the decay products at the intended tumour site, thereby reducing toxicity to healthy tissue.
- Astatine-211 has a relatively short half-life (7.2 hours), making it suitable for certain treatments where rapid clearance from non-target tissues is desired. As a halogen, it can be integrated into organic compounds, similar to iodine radionuclides. Its powerful alpha emissions have been investigated in the context of intracavity therapy for some brain and thyroid cancers. However, producing At-211 in sufficient quantities involves cyclotron-based methods, requiring specific infrastructure that might limit its clinical use.
Production and Availability of Alpha Emitters
Before a radiopharmaceutical can be employed clinically, it must be available in adequate quantities. Nuclear reactors or particle accelerators produce many alpha particle-emitting radionuclides. For instance, Ra-223 is often generated via a decay process from thorium-227, while Ac-225 is conventionally produced by the decay of radium-225 or through accelerator-based transmutation of thorium. Each route demands careful consideration of cost, safety, and scalability.
Research facilities worldwide have been exploring more efficient production methods in the quest for improved radionuclide therapy. Expanding the availability of each medical isotope is vital to support large-scale clinical trials and subsequent routine clinical use. Production capability is tied to national and international initiatives that unite governments, research institutions, and private companies. Through collaboration, it becomes possible to secure a stable supply of alpha emitters, ensuring that these promising therapies can reach a broader range of patients.
Radiolabelling and Molecular Carriers
One of the main ways to exploit the potency of alpha particle emitters is to link them to molecules that specifically target cancer cells. Monoclonal antibodies, peptides, and small molecules can be employed to direct the radiopharmaceutical to antigens or receptors overexpressed by malignant tissues. This selective approach results in high doses of targeted radiation delivered directly to tumour cells, lowering the risk of damaging healthy cells.
The process of attaching an alpha emitter to a carrier involves the use of chelators—chemical agents designed to hold the radioactive metal securely. This ensures that the radioactive ion remains in place until it decays within the targeted region. Different labelling strategies are required for non-metal isotopes like At-211, often involving covalent bonding rather than chelation. This step is crucial for achieving a stable and effective therapeutic agent. Any leakage of free radionuclide from the carrier could harm non-target organs such as the kidneys or bone marrow. Therefore, advanced radiochemistry methods are continually being developed to perfect conjugation strategies for various medical isotope types.
Biological Mechanisms of Alpha Emitters
Alpha particles exhibit high linear energy transfer (LET), depositing much energy over a short path. This characteristic underpins the potency of alpha emitting radionuclides in radionuclide therapy. By causing direct DNA double-strand breaks, alpha emissions trigger cell death in malignant cells. Even a few alpha tracks can be enough to kill a tumour cell, highlighting why an alpha emitter can be such a powerful therapeutic agent for targeted cancer treatment.
However, the same potency that makes alpha emissions effective can also raise toxicity concerns if an alpha emitter is misdirected. Off-target transport of a radiopharmaceutical may damage healthy tissues. Consequently, the carrier molecule’s specificity and the chelation chemistry’s stability are fundamental to safe and effective therapy. Research is ongoing to improve tumour selectivity, reduce immunogenic responses to large protein carriers, and develop new small-molecule or peptide-based strategies for precise targeted radiation.
Clinical Applications and Evidence
Clinical success with alpha emitting radionuclides is growing, with radium-223 leading the way. Approved by regulatory agencies for the treatment of bone metastases in castration-resistant prostate cancer, Ra-223 has been shown to extend survival, alleviate pain, and improve quality of life in many patients. This success story has sparked interest in applying radionuclide therapy with other alpha emitters to treat different solid tumours, lymphomas, and haematological malignancies.
Actinium-225-based radiopharmaceuticals are particularly exciting. Preliminary clinical trials have examined the safety and efficacy of Ac-225 labelling antibodies targeting leukaemia cells, demonstrating powerful tumour control in certain cases. Although careful management of dose-limiting toxicity is required, these early results suggest that Ac-225 could become a valuable therapeutic agent for cancers resistant to traditional treatments.
Astatine-211 also holds promise. Studies show that At-211 can produce significant tumour regressions in ovarian, glioma, and thyroid malignancy models. It may become a valuable option for specific patient populations through strategies that direct At-211 to cancerous tissues while allowing for swift clearance from normal cells. The short half-life of At-211 must be managed effectively, calling for robust distribution networks and local production using cyclotrons located near treatment centres.
Safety Considerations and Toxicity
Although alpha emitters are remarkably potent against cancer cells, safety management is essential. High-energy alpha particles can cause significant localised damage, and if the radiopharmaceutical is not localised correctly, toxicity to healthy tissues may be profound. Common concerns include myelosuppression (reduced bone marrow function), nephrotoxicity, and off-target organ toxicity, depending on the specific carrier and medical isotope.
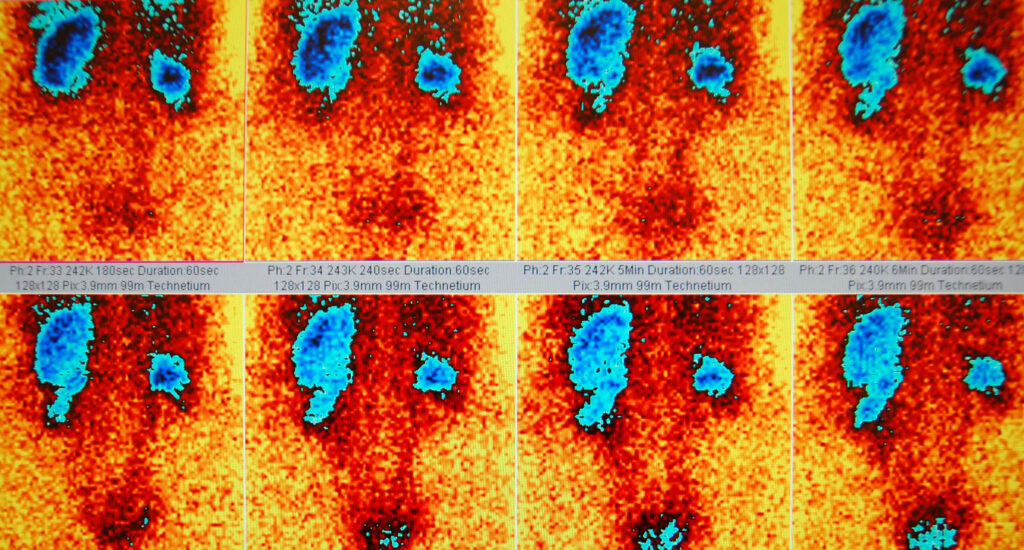
Thus, patient selection and accurate dosimetry become paramount in safe clinical use. Personalised treatment planning, where the administered activity is tailored to each individual’s absorption, clearance rates, and tumour burden, helps balance therapeutic benefits with adverse effects. Such planning uses imaging techniques, biochemical markers, and careful observation of side effects during treatment.
Technological and Manufacturing Advances
The efficient production of alpha emitters is one of the most significant hurdles in bringing these therapies to a broader population. Laboratories continually refine methods to generate enough medical isotope supply without excessive radioactive waste. For instance, new accelerator-based routes for Ac-225 production are under development to create a sustainable supply for widespread clinical use.
In parallel, improvements in radiochemistry techniques have made labelling proteins, peptides, and small molecules with alpha emitters simpler. Automated synthesis modules are becoming more accessible, improving reproducibility and reducing the risk of errors during production. As researchers refine these processes, they anticipate enhanced safety profiles, lower costs, and the potential to offer radionuclide therapy to more patients.
Regulatory and Practical Considerations
Developing a new radiopharmaceutical is a complex process involving health authorities’ approval. Regulatory bodies require rigorous testing of purity, stability, and safety. The short half-lives of many alpha emitters add urgency to the logistics of transport and administration, making it crucial to coordinate among production sites, nuclear medicine departments, and clinical teams.
Furthermore, the disposal of radioactive waste must be handled with caution. Each unused portion of a radioactive therapeutic agent poses a hazard if not managed according to strict environmental and safety regulations. This challenge extends to used vials, syringes, and other medical consumables that come into contact with radioactive materials.
Future Perspectives and Research Directions
Ongoing research aims to refine existing targeted radiation approaches and explore new alpha emitting radionuclides. There is also growing interest in combining radionuclide therapy with immunotherapy, chemotherapy, or external beam radiation for enhanced results. Early-stage studies indicate that alpha emitters can initiate immunogenic cell death, potentially boosting the body’s immune response against tumours.
Looking ahead, multi-isotope strategies may become more prevalent, combining alpha emitters with beta or Auger electron emitters for synergistic effects. This approach could allow for a more tailored treatment, matching tumour characteristics with the most effective therapeutic agent. Researchers are also examining ways to improve real-time imaging of alpha-emitting compounds, assisting clinicians in adapting therapy protocols to dynamic changes in tumour uptake.
Overcoming Challenges and Ensuring Widespread Adoption
Although alpha particle therapy has shown remarkable potential, challenges remain in scaling up production, mastering radiolabelling technology, and navigating the regulatory environment. Economic factors also play a part, as the cost of a specialised radiopharmaceutical can be high. Collaborative efforts between industry, governments, and academic institutions are essential to streamline these processes, ensuring that patients worldwide can benefit from the latest developments in medical isotope research.
Patient and clinician education is another vital part of promoting acceptance of alpha therapy. Clear communication about benefits, risks, and the role of this targeted approach helps patients make informed decisions about their treatment options. Transparent discussions regarding potential side effects and appropriate supportive measures can foster trust and encourage broader participation in clinical trials.
Conclusion
Alpha particle emitting radionuclides represent a transformative avenue within radionuclide therapy. Owing to their high linear energy transfer and capacity to deliver targeted radiation to malignant cells, they have demonstrated promising outcomes in certain cancers. Each alpha emitter discussed—Ra-223, Ac-225, Th-227, and At-211—has unique chemical and physical characteristics that influence its potential application, production requirements, and safety profile.
Collaborating among researchers, clinicians, and the pharmaceutical industry will be central to overcoming existing obstacles. By refining production pathways for each medical isotope, developing stable radiolabelling methods, and conducting robust clinical trials, the adoption of alpha particle therapy will continue to expand. Equally, efforts to optimise patient selection, individualise dosimetry, and manage toxicity are paramount to ensure this therapeutic agent’s safe and effective use.
With further research, alpha emitters could serve as a cornerstone of cancer treatment, providing hope for patients who might not respond to conventional therapies. Given the momentum in this field, it is clear that alpha emitting radionuclides hold an important place in the future of precision oncology.
Disclaimer
The information presented in Selected Alpha Particle Emitting Radionuclides for Therapeutic Nuclear Medicine by Open Medscience is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. The content reflects current scientific understanding and research as of the date of publication (7 January 2025), but developments in the field may alter its relevance or accuracy over time.
Open Medscience does not endorse or recommend any specific medical treatments, products, or procedures referenced in this article. The discussion of radionuclides and their clinical applications is intended to provide general background on therapeutic nuclear medicine and should not be interpreted as a recommendation for use in any individual case.
Readers are advised to consult qualified healthcare professionals for advice regarding medical conditions or treatment options. Additionally, regulatory approvals and clinical protocols may vary by country; it is the responsibility of the reader to ensure compliance with applicable laws, regulations, and professional standards.
Open Medscience disclaims any liability for loss, injury, or damage incurred as a consequence of reliance on the information provided herein.
home » diagnostic medical imaging blog » medical radiotherapeutics »