Iodine-131 Therapy
Iodine-131 therapy, a cornerstone in the treatment of thyroid conditions, particularly thyroid cancer, harnesses the specific properties of the radioactive isotope Iodine-131. This therapeutic approach is prevalent in the UK for its efficacy in targeting both benign and malignant thyroid tissue. Here, we delve into the fundamentals of this treatment, its application, potential side effects, and the care considerations necessary for patients undergoing this specialised form of therapy.
Fundamentals of Iodine-131 Therapy
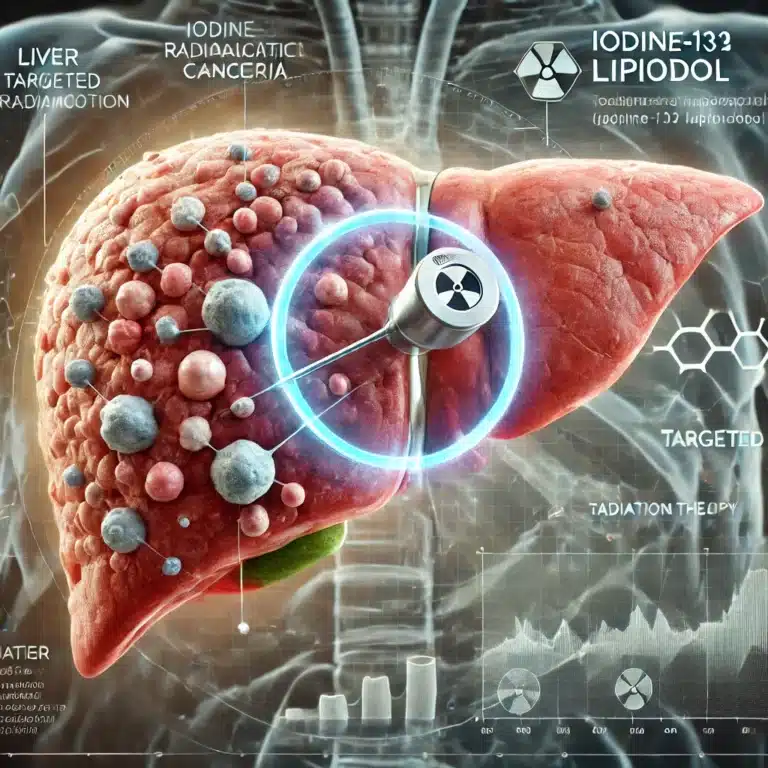
Iodine-131 therapy operates on the principle of radioactive decay. Iodine-131 emits beta and gamma radiation, destroying thyroid cells and allowing for diagnostic imaging. The thyroid gland naturally absorbs iodine. Thus, when Iodine-131 is administered orally, usually in a capsule or liquid form, it concentrates in thyroid cells. This selective uptake leads to the destruction of both normal thyroid tissue and thyroid cancer cells, providing a targeted approach to treatment.
Applications of Iodine-131
The primary application of Iodine-131 is in managing differentiated thyroid cancer, including papillary and follicular thyroid cancers. It’s used postoperatively to ablate any remaining thyroid tissue after the thyroid gland is surgically removed, a procedure known as thyroidectomy. Additionally, Iodine-131 can treat certain types of hyperthyroidism, such as Graves’ disease, by reducing the function of the overactive thyroid gland.
Side Effects and Risks
While effective, Iodine-131 therapy is not devoid of side effects. Short-term side effects may include neck pain, nausea, swelling of the salivary glands, dry mouth, and altered taste sensation. There is also a minor risk of developing secondary cancers long-term. To mitigate these risks, hospitals follow strict guidelines to monitor radiation exposure and limit the potential spread of radioactivity.
Post-Treatment Care
Patients receiving Iodine-131 therapy typically undergo a brief period of isolation to prevent radiation exposure to others. This isolation is crucial as the body can emit radiation for several days post-treatment. Healthcare providers offer detailed guidance on safety measures, such as avoiding close contact, particularly with children and pregnant women, and maintaining good hygiene to reduce radiation transmission through bodily fluids.
Patients are also monitored through follow-up appointments, during which thyroid function tests and scans are conducted to assess the efficacy of the treatment and adjust any further treatment plans.
In conclusion, Iodine-131 therapy is a pivotal treatment modality in the field of thyroid disease management within the UK. Its targeted approach effectively destroys thyroid cells with minimal impact on the rest of the body. However, careful handling and stringent safety protocols are essential to optimise outcomes and minimise risks for patients undergoing this therapy.
You are here:
home » Iodine-131 Therapy