Beta Emitter Therapy
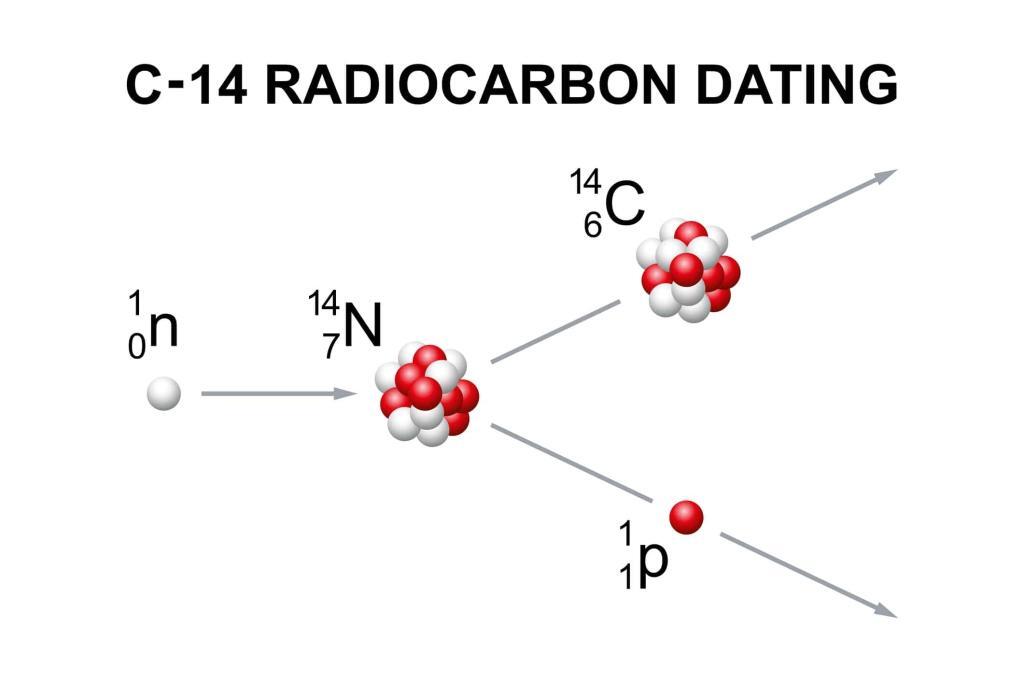
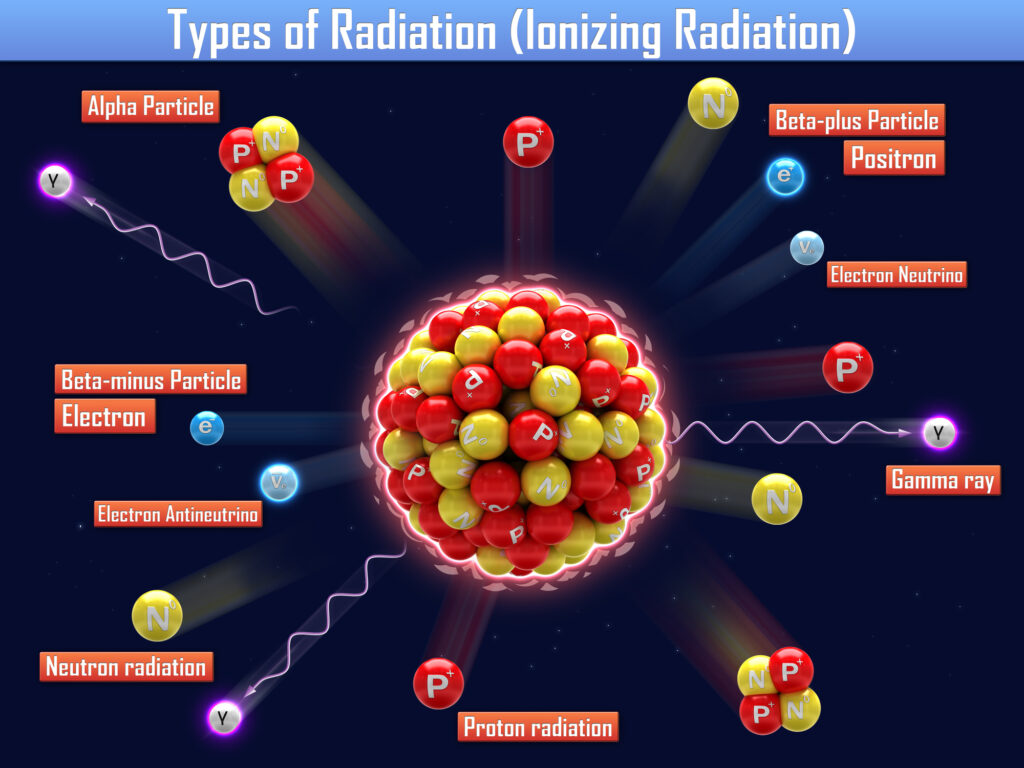
Beta emitter therapy, also known as beta radiation therapy, is a form of targeted radiotherapy that utilises beta radiation to treat certain diseases, predominantly cancer. This method capitalises on the destructive properties of beta particles—high-energy, high-speed electrons or positrons emitted by radioactive decay—to selectively attack and kill malignant cells while minimising damage to the surrounding healthy tissue.
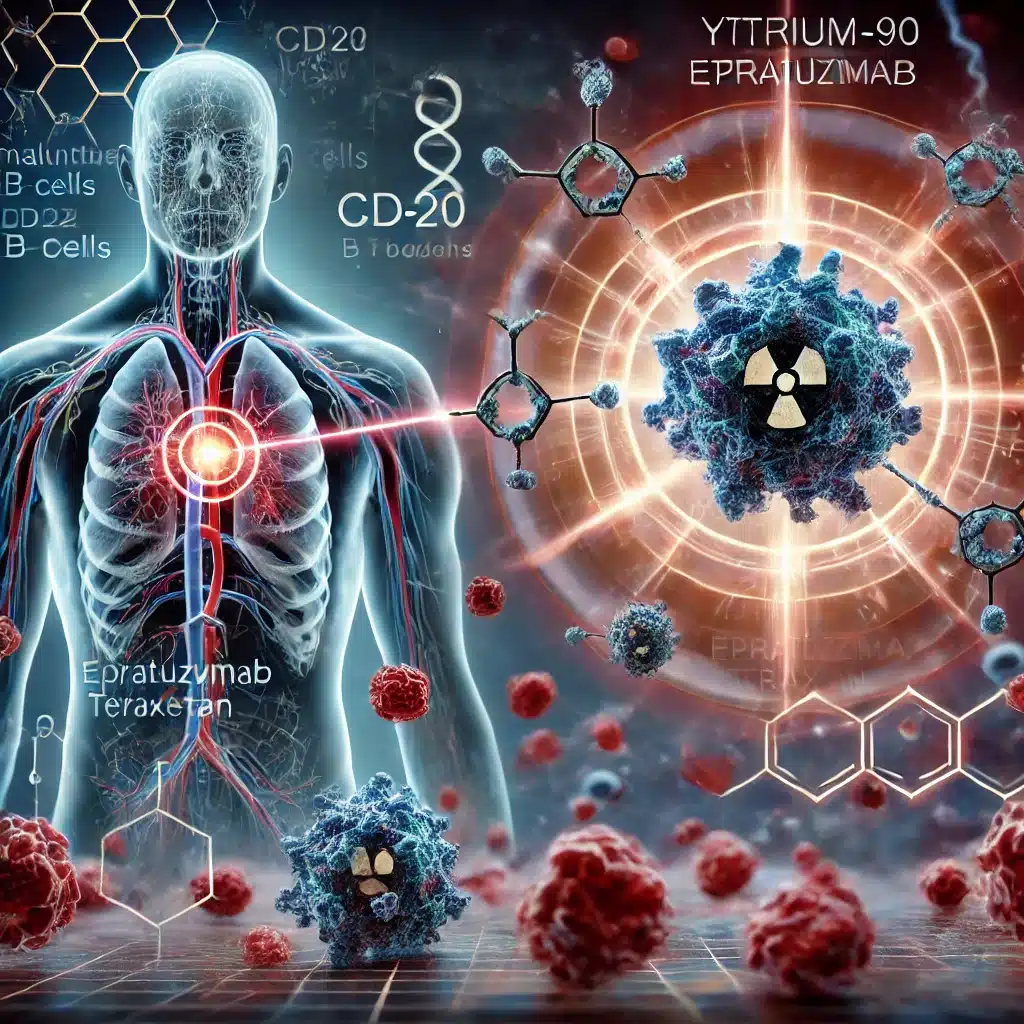
The underlying principle of beta emitter therapy is based on the radioactive decay of beta-emitting isotopes, such as iodine-131, yttrium-90, and lutetium-177. These isotopes are incorporated into compounds that specifically target cancer cells. For instance, in the treatment of thyroid cancer, iodine-131 is commonly used because the thyroid gland naturally absorbs iodine, thus delivering the radioactive material directly to the cancerous cells.
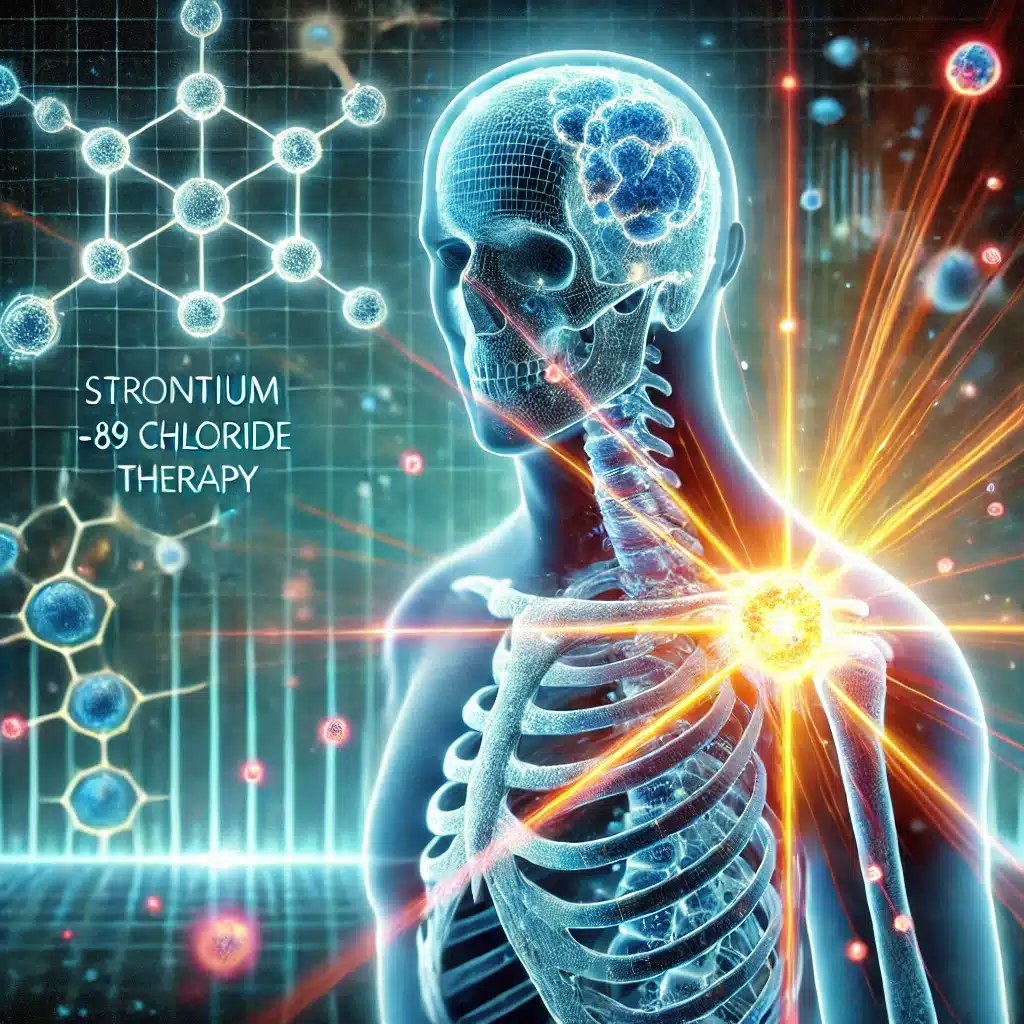
One of the main advantages of using beta emitters in cancer therapy is their ability to deliver a high dose of radiation directly to the target cells with a limited range of penetration, typically a few millimetres in tissue. This localised action reduces the risk of widespread radiation exposure, thereby limiting the side effects commonly associated with external beam radiation therapies.
Yttrium-90 is another widely used isotope in beta emitter therapy. It is particularly effective in the treatment of non-Hodgkin lymphoma and liver cancer. Yttrium-90 microspheres are injected directly into the liver’s bloodstream, allowing them to become lodged in the capillaries of liver tumours, where they deliver targeted radiation. This method, known as radioembolisation, has shown significant promise in controlling and reducing liver tumours, improving patient survival rates and quality of life.
Lutetium-177 is employed in a somewhat different context, particularly in peptide receptor radionuclide therapy (PRRT). In this treatment, Lutetium-177 is attached to a molecule specifically targeting somatostatin receptors, often abundant in neuroendocrine tumours. This approach allows for high specificity in targeting and killing cancer cells while preserving healthy cells, making it an effective treatment for managing symptoms and extending survival in patients with this type of cancer.
However, the efficacy and precision of beta emitter therapy pose challenges and risks. The handling and disposal of radioactive materials require stringent safety protocols to protect both medical personnel and patients from undue radiation exposure. Moreover, the specificity of the isotopes to target tissues can sometimes lead to incomplete treatment of the cancer if not all tumorous cells express the targeted receptors or absorb the radioactive compound.
In conclusion, beta emitter therapy represents a significant advancement in the field of oncology, providing effective, targeted treatment options for various cancers. As research continues, the potential applications of this therapy are expanding, offering hope for more refined and effective treatments in the future.
You are here:
home » Beta Emitter Therapy