Summary: Medical imaging has traditionally been associated with diagnosing structural abnormalities, tumours, fractures, and vascular diseases. However, advancements in imaging science have extended its capabilities into the detection, monitoring, and understanding of viral infections in the human body. By providing visual insights into how viruses affect tissues and organs, imaging modalities such as magnetic resonance imaging (MRI), computed tomography (CT), positron emission tomography (PET), ultrasound, and emerging molecular imaging techniques are transforming the way viral diseases are diagnosed and managed. These technologies not only support early detection and disease characterisation but also guide treatment decisions, monitor therapeutic responses, and contribute to the development of new antiviral therapies. As viruses continue to evolve and pose global health challenges, medical imaging stands at the forefront of precision diagnostics and personalised medicine in virology.
Keywords: Medical Imaging, Viral Detection, MRI, PET, Molecular Imaging, Diagnostics.
Expanding the Role of Imaging Beyond Structural Disease
For decades, medical imaging has been an indispensable tool in clinical medicine, primarily used to visualise structural and anatomical changes associated with various diseases. Yet, as viral infections continue to be a major cause of morbidity and mortality worldwide, the role of imaging is evolving. Viral diseases, once diagnosed primarily through serological and molecular tests, are increasingly being studied and detected using advanced imaging techniques. These methods enable clinicians to observe the indirect and direct effects of viruses on the body, from inflammation and tissue damage to metabolic changes and immune responses.
Imaging technologies are particularly valuable because they offer a non-invasive window into disease progression, capturing dynamic physiological processes in real time. They allow healthcare professionals to identify complications, assess organ involvement, and detect viral activity even when laboratory tests alone may not provide sufficient information. As imaging science integrates with molecular biology and virology, it is emerging as a crucial tool in understanding viral pathogenesis and improving patient outcomes.
MRI and CT: Visualising Tissue Damage and Inflammatory Responses
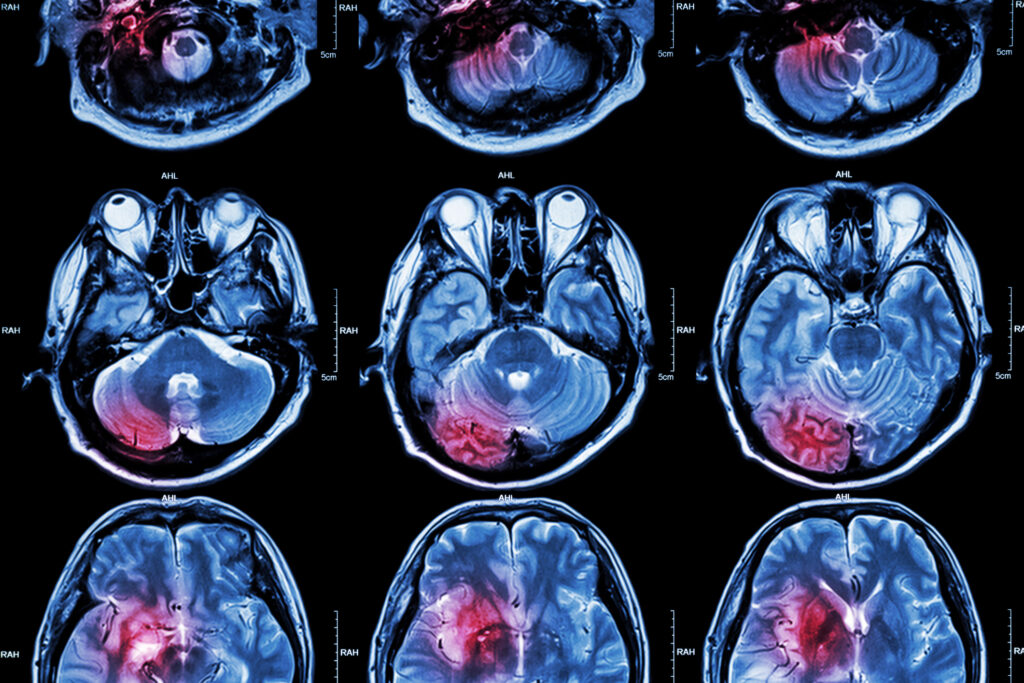
Magnetic resonance imaging (MRI) and computed tomography (CT) remain two of the most widely used imaging modalities in detecting the effects of viral infections. While these techniques do not typically visualise viruses directly due to their microscopic size, they are instrumental in revealing the structural and functional changes viruses cause in tissues and organs.
MRI is particularly effective at identifying inflammation, demyelination, and oedema in soft tissues, which are common consequences of viral infections. For example, in viral encephalitis caused by herpes simplex virus, MRI can show characteristic signal abnormalities in the temporal lobes, aiding rapid diagnosis and timely treatment. Similarly, MRI has been used to detect cardiac inflammation in viral myocarditis, where it reveals myocardial oedema, fibrosis, and functional impairment.
CT, on the other hand, is widely used to detect respiratory viral infections. During the COVID-19 pandemic, CT imaging played a central role in identifying ground-glass opacities, consolidations, and other characteristic lung changes associated with SARS-CoV-2 infection. These findings not only helped diagnose infection but also provided valuable prognostic information regarding disease severity and progression. In cases of viral hepatitis, CT and MRI can identify liver inflammation, fibrosis, and cirrhosis, helping clinicians evaluate the extent of hepatic damage and plan appropriate interventions.
Both MRI and CT demonstrate how imaging can bridge the gap between laboratory findings and clinical presentation by providing direct visual evidence of viral effects on tissues. Their ability to detect complications such as encephalitis, pneumonia, or myocarditis underscores their value in the comprehensive assessment of viral diseases.
PET and SPECT: Metabolic and Molecular Insights into Viral Activity
Positron emission tomography (PET) and single-photon emission computed tomography (SPECT) represent the next level of sophistication in medical imaging by offering functional and molecular information rather than purely anatomical details. These nuclear medicine techniques use radiotracers to highlight metabolic processes and molecular interactions that change during viral infections.
Viruses often alter cellular metabolism and immune activity, and PET imaging can detect these changes. For instance, 18F-fluorodeoxyglucose (FDG)-PET, which measures glucose metabolism, can reveal areas of heightened immune activity during viral infections. Increased FDG uptake has been observed in patients with HIV, hepatitis, and COVID-19, indicating active inflammation and immune cell recruitment. PET imaging can also be used to monitor the success of antiviral therapy by showing reductions in metabolic activity as the infection resolves.
SPECT imaging, though less spatially detailed than PET, is valuable for assessing immune responses and tracking labelled antibodies or antiviral drugs. It can be used to study viral dissemination patterns or evaluate how immune cells interact with infected tissues.
The integration of PET and SPECT into viral diagnostics is particularly significant for research and drug development. By visualising viral replication sites and host responses, these modalities contribute to a deeper understanding of viral pathophysiology and support the design of more effective therapies.
Molecular Imaging: Targeting Viruses at the Cellular and Molecular Level
One of the most exciting developments in the detection of viruses is molecular imaging, a field that combines imaging technology with molecular biology to visualise specific cellular and molecular events. Unlike conventional imaging, which primarily identifies structural or metabolic changes, molecular imaging can detect viral components or the cellular processes they trigger.
Techniques such as reporter gene imaging, targeted contrast agents, and nanoparticle-based probes are being developed to visualise viral infection at unprecedented levels of specificity. Reporter genes inserted into viral genomes can express detectable signals, allowing real-time monitoring of viral replication and spread in living organisms. Targeted probes designed to bind viral proteins or infected cells enable precise localisation of infection sites, even before significant tissue damage occurs.
Molecular imaging holds significant promise in the study of latent and chronic viral infections. For example, it can help identify reservoirs of latent HIV, a critical step in efforts to achieve a functional cure. It also shows potential in tracking hepatitis B virus covalently closed circular DNA (cccDNA), a persistent viral form that evades conventional diagnostic methods.
As molecular imaging advances, it will complement traditional diagnostic techniques by enabling earlier detection, more accurate disease staging, and better monitoring of therapeutic interventions. This precision could revolutionise how viral infections are diagnosed and treated.
Clinical Applications: Imaging Viral Diseases Across Organ Systems
The clinical utility of medical imaging in viral detection spans multiple organ systems, reflecting the diverse manifestations of viral infections. In the central nervous system, imaging plays a key role in diagnosing viral encephalitis, meningitis, and progressive multifocal leukoencephalopathy. MRI’s sensitivity to white matter changes and inflammation is particularly valuable in these cases, often providing the first indication of a viral cause when clinical symptoms are non-specific.
In the cardiovascular system, imaging is essential for detecting viral myocarditis and pericarditis. Cardiac MRI not only confirms the diagnosis but also assesses disease severity and monitors response to therapy. Similarly, PET imaging has been explored to detect vascular inflammation linked to viral infections, such as the endothelial damage seen in severe COVID-19.
The respiratory system remains a major focus of viral imaging. CT scans are widely used to evaluate viral pneumonias, and their patterns can help differentiate between viral and bacterial causes. During outbreaks of influenza, SARS, MERS, and COVID-19, imaging provided crucial diagnostic support, especially when molecular testing was limited or results were delayed.
In the liver, MRI and ultrasound are integral to assessing viral hepatitis and its complications. They allow clinicians to detect fibrosis, cirrhosis, and hepatocellular carcinoma early, improving patient outcomes. Similarly, in the gastrointestinal tract, imaging can identify complications from viral infections such as cytomegalovirus colitis.
These diverse clinical applications demonstrate that imaging is not limited to detecting viruses themselves but extends to understanding their systemic effects. This comprehensive view enables clinicians to provide more accurate diagnoses, anticipate complications, and tailor treatment strategies to individual patients.
Future Directions: AI, Hybrid Imaging, and Precision Virology
The future of viral detection through medical imaging lies at the intersection of technology, biology, and artificial intelligence (AI). AI algorithms are increasingly being used to enhance image interpretation, detect subtle changes that may escape human observation, and predict disease progression. During the COVID-19 pandemic, AI-assisted CT analysis significantly improved the speed and accuracy of diagnosis, highlighting its potential in future viral outbreaks.
Hybrid imaging systems, such as PET/MRI and PET/CT, are becoming more prevalent, combining the strengths of anatomical and functional imaging in a single scan. These systems provide comprehensive data on both the structural and molecular changes associated with viral infections, offering a more complete picture of disease processes.
Emerging techniques like hyperpolarised MRI, optical imaging, and photoacoustic imaging are expanding the capabilities of viral detection even further. These methods promise higher sensitivity, faster acquisition times, and new types of contrast that could reveal viral activity at the cellular level.
Moreover, the integration of imaging with precision medicine is set to transform virology. By linking imaging findings with genomic and proteomic data, clinicians can gain insights into how specific viral strains interact with the host and respond to therapy. This integrated approach could pave the way for personalised antiviral treatments tailored to individual patients’ disease profiles.
Conclusion: Medical Imaging as a Key Tool in Viral Diagnostics
Medical imaging is evolving from a tool that visualises structural changes to one that provides deep insights into molecular and cellular processes, making it increasingly important in the detection and management of viral infections. MRI and CT reveal the structural and inflammatory consequences of infection, while PET and SPECT offer functional and metabolic perspectives. Molecular imaging pushes the boundaries further, enabling the detection of viral activity at the cellular level and supporting the development of new diagnostic and therapeutic approaches.
As imaging technologies become more sophisticated and integrated with AI and molecular biology, they will play an even greater role in virology. They will not only support earlier and more accurate diagnoses but also contribute to understanding viral behaviour, guiding treatment decisions, and monitoring therapeutic outcomes. In an era where emerging viruses pose ongoing global health threats, medical imaging stands as an essential tool in the fight against viral disease, bridging the gap between laboratory science and clinical care.
Q: What is the central role of medical imaging in detecting viruses?
A: Medical imaging helps detect and monitor the effects of viral infections by visualising the structural, functional, and molecular changes they cause in the body. Although viruses themselves are too small to be seen directly, imaging shows the damage they inflict on tissues and organs, reveals inflammatory responses, tracks disease progression, and supports treatment planning.
Q: Which imaging techniques are most commonly used for detecting viral infections?
A: The most commonly used techniques include magnetic resonance imaging (MRI), computed tomography (CT), positron emission tomography (PET), single-photon emission computed tomography (SPECT), ultrasound, and molecular imaging. Each provides different types of information, ranging from structural changes to molecular activity.
Q: How does MRI help in diagnosing viral infections?
A: MRI is highly sensitive to changes in soft tissues and is used to detect inflammation, oedema, demyelination, and tissue damage caused by viruses. For example, it can show temporal lobe abnormalities in herpes simplex encephalitis or myocardial inflammation in viral myocarditis.
Q: What role does CT imaging play during viral outbreaks?
A: CT is especially useful in detecting respiratory infections. During the COVID-19 pandemic, CT scans revealed lung changes such as ground-glass opacities and consolidations, which helped diagnose the disease, assess severity, and guide treatment even when molecular test results were pending.
Q: How do PET and SPECT contribute to viral detection?
A: PET and SPECT provide functional and molecular insights by highlighting metabolic and immune changes during infection. PET scans using radiotracers like ^18F-FDG can identify areas of increased immune activity, while SPECT can track immune responses or the distribution of antiviral drugs. These techniques are also valuable for monitoring how well treatments are working.
Q: What is molecular imaging, and how is it different from traditional imaging?
A: Molecular imaging focuses on visualising cellular and molecular events rather than just anatomical structures. It uses targeted probes, reporter genes, or nanoparticles to detect specific viral components or infected cells, often before visible tissue damage occurs. This approach enables earlier and more precise detection than conventional imaging methods.
Q: In which organ systems is medical imaging most useful for detecting viral infections?
A: Imaging is valuable across many organ systems. It detects encephalitis in the brain, myocarditis in the heart, pneumonia in the lungs, hepatitis in the liver, and viral colitis in the gastrointestinal tract. Each modality provides information relevant to the affected organ, helping clinicians diagnose and manage complications.
Q: How is artificial intelligence (AI) improving viral detection in imaging?
A: AI enhances image interpretation by identifying subtle changes that may be missed by human observers and predicting disease progression. It was widely used during the COVID-19 pandemic to improve diagnostic speed and accuracy from CT scans. AI also supports automated image analysis in large-scale screening and research.
Q: What are hybrid imaging systems, and why are they significant?
A: Hybrid systems, such as PET/CT and PET/MRI, combine the anatomical detail of structural imaging with the molecular and functional data of nuclear imaging. This integration provides a more complete picture of how viruses affect the body, improving diagnosis, monitoring, and research.
Q: How might medical imaging shape the future of viral diagnostics?
A: The future lies in combining imaging with AI, genomics, and precision medicine to deliver earlier, more accurate, and personalised diagnoses. Advanced imaging technologies and molecular probes will allow direct tracking of viral activity, guide the development of new antiviral therapies, and support targeted treatment strategies.
Q: Can medical imaging detect viruses directly?
A: Not usually. Most imaging techniques cannot visualise viruses due to their microscopic size. Instead, they detect the biological and pathological changes viruses cause in tissues, organs, and metabolic processes. Molecular imaging is an exception, as it can sometimes identify viral components or infected cells using targeted probes.
Q: Why is medical imaging becoming increasingly important in virology?
A: As viruses continue to evolve and pose global health threats, imaging provides vital information that laboratory tests alone cannot. It offers a real-time, non-invasive way to monitor disease progression, detect complications, and evaluate treatment responses, making it an essential tool in modern virology and personalised medicine.
Disclaimer
The information provided in this article, “The Role of Medical Imaging in Detecting Viruses in the Human Body”, is intended for educational and informational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Medical imaging techniques discussed herein should only be performed and interpreted by qualified healthcare professionals. Readers should not use this information to diagnose or manage any medical condition without consulting a suitably qualified medical practitioner. Open MedScience does not accept any responsibility or liability for any actions taken based on the content of this article.