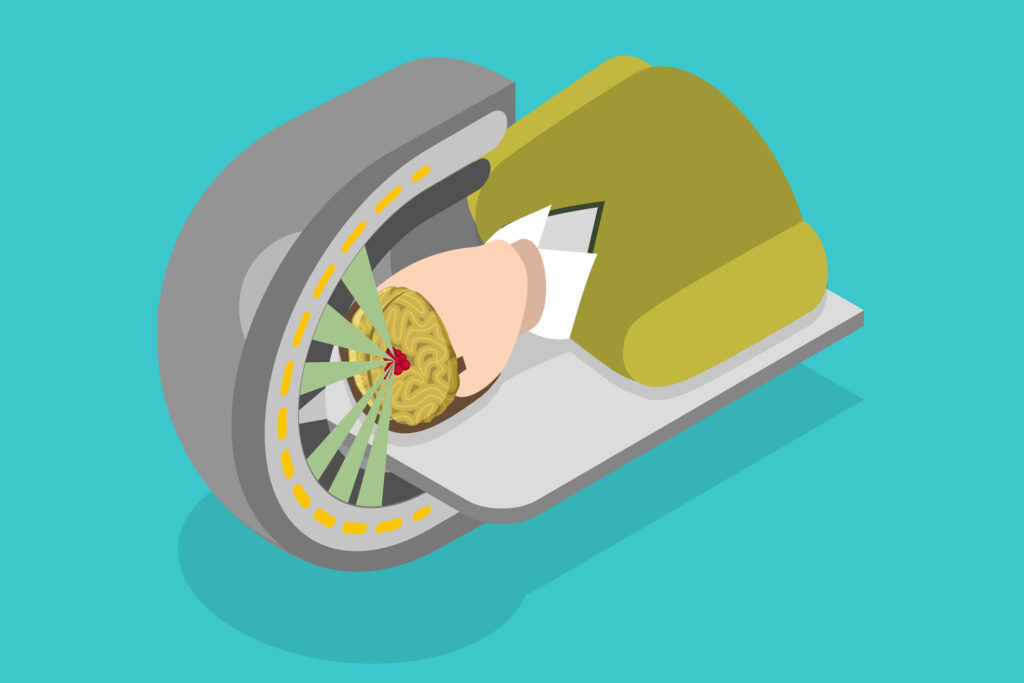
Radionuclide therapy has gained prominence as an effective treatment for various types of cancers, particularly those involving the thyroid, prostate, and neuroendocrine systems. By delivering targeted radiation to malignant cells, this therapy offers a more precise approach than conventional external beam radiation. However, radionuclide therapy is not without its adverse effects. Patients undergoing such treatment may experience both acute and long-term side effects that range from mild to severe. These effects can impact several bodily systems, including the haematological, gastrointestinal, and renal systems. Additionally, secondary malignancies and radiation toxicity are potential risks associated with radionuclide therapy. This article focuses on the common and less frequent adverse effects of radionuclide therapy, providing a detailed overview of the potential risks involved.
Introduction to Radionuclide Therapy
Radionuclide therapy, also known as targeted radiotherapy or molecular radiotherapy, involves administering radioactive substances to target cancer cells selectively. The therapy has shown substantial success in treating cancers such as thyroid carcinoma, neuroendocrine tumours, and metastatic prostate cancer. Radionuclides like iodine-131, lutetium-177, and yttrium-90 are commonly used to deliver radiation directly to cancer cells, thereby reducing the risk of damage to healthy tissues.
Although radionuclide therapy has a high efficacy rate, it is accompanied by potential risks. These adverse effects can manifest as short-term complications immediately following treatment or long-term issues that arise after months or even years. Understanding these adverse effects is essential for healthcare professionals to manage them effectively and improve patient outcomes.
Common Adverse Effects
Haematological Toxicity
Haematological toxicity is one of the most frequently observed adverse effects of radionuclide therapy. The bone marrow is particularly vulnerable to radiation damage, as it is responsible for the production of blood cells. When exposed to radiation, bone marrow function can become compromised, leading to a condition known as myelosuppression.
Myelosuppression and Its Implications
Myelosuppression refers to the reduction in the production of blood cells, including red blood cells, white blood cells, and platelets. This condition can result in anaemia, increased susceptibility to infections, and impaired blood clotting. Patients undergoing radionuclide therapy may require frequent blood tests to monitor their haematological parameters and may need supportive treatments, such as blood transfusions or growth factors, to manage these complications.
The severity of myelosuppression depends on factors such as the type and dosage of radionuclide used, the patient’s pre-existing health condition, and the duration of therapy. In most cases, myelosuppression is reversible after the treatment is completed, but it may take weeks or months for full recovery.
Gastrointestinal Toxicity
Gastrointestinal (GI) side effects are also commonly associated with radionuclide therapy. The GI tract is sensitive to radiation, and patients may experience a range of symptoms depending on the radionuclide used and the dosage administered.
Nausea and Vomiting
Nausea and vomiting are among the most frequent acute side effects of radionuclide therapy. They typically occur shortly after the administration of the radionuclide and can last for several days. These symptoms are generally managed with antiemetic medications, which help control nausea and prevent vomiting. While the majority of patients respond well to these medications, some may require further interventions, such as adjusting the treatment regimen.
Diarrhoea and Abdominal Pain
Diarrhoea and abdominal pain are also common side effects, especially when radionuclide therapy targets the abdominal or pelvic regions. These symptoms can significantly affect a patient’s quality of life during treatment. In some cases, diarrhoea may persist beyond the treatment period, necessitating further medical intervention and dietary modifications.
Less Common but Serious Adverse Effects
Renal Toxicity
Renal toxicity is a less common but serious complication of radionuclide therapy, particularly when the kidneys are exposed to significant levels of radiation. Lutetium-177 and yttrium-90, which are commonly used in radionuclide therapy, are primarily excreted through the kidneys, increasing the risk of renal damage.
Risk Factors and Management
Patients with pre-existing kidney conditions, those who are elderly, or those receiving high doses of radionuclides are at an increased risk of developing renal toxicity. Symptoms may include reduced kidney function, proteinuria (excess protein in the urine), and elevated creatinine levels. In severe cases, renal failure may occur, requiring dialysis or other interventions.
To mitigate the risk of renal toxicity, healthcare professionals may use protective agents such as amino acid infusions, which help reduce radiation exposure to the kidneys. Regular monitoring of kidney function is also essential throughout the treatment process.
Secondary Malignancies
One of the more concerning long-term risks of radionuclide therapy is the potential for secondary malignancies. While radionuclide therapy is highly targeted, it is not entirely free from the risk of causing radiation-induced cancers. This risk is particularly relevant for younger patients, who may have a longer life expectancy and, thus, a higher chance of developing a secondary malignancy later in life.
Mechanisms and Incidence
Radiation-induced cancers may develop in tissues adjacent to or distant from the treatment site. The risk of secondary malignancies is related to the total radiation dose delivered, the type of radionuclide used, and the patient’s genetic predisposition. The incidence of secondary malignancies after radionuclide therapy is generally low, but the possibility remains a significant concern that necessitates long-term follow-up and surveillance.
Radiation Toxicity
Radiation toxicity refers to the broader category of adverse effects that can arise from the exposure of healthy tissues to radiation during radionuclide therapy. While the therapy is designed to deliver radiation primarily to cancer cells, some degree of collateral damage to surrounding tissues is unavoidable.
Acute Radiation Toxicity
Acute radiation toxicity occurs shortly after treatment and is generally characterised by inflammation and damage to tissues in the immediate vicinity of the tumour. Symptoms may include skin reactions, such as redness and irritation, as well as swelling and tenderness at the treatment site. In some cases, acute toxicity can affect internal organs, leading to symptoms such as fatigue, fever, and loss of appetite.
Chronic Radiation Toxicity
Chronic radiation toxicity may develop months or even years after the completion of radionuclide therapy. This form of toxicity can manifest as fibrosis, which is the abnormal thickening of tissues due to excessive scarring. Fibrosis can affect various organs, including the lungs, liver, and gastrointestinal tract, leading to impaired organ function and reduced quality of life.
The management of chronic radiation toxicity is challenging, as the damage may be irreversible. In some cases, medical interventions, such as steroids or other anti-inflammatory medications, may be used to control symptoms and prevent further progression of the condition.
Specific Adverse Effects by Radionuclide
Iodine-131
Iodine-131 is one of the most commonly used radionuclides in the treatment of thyroid cancer. While it is highly effective in targeting thyroid tissue, it is also associated with several specific adverse effects.
One of the notable side effects of iodine-131 therapy is damage to the salivary glands. Patients may experience dry mouth (xerostomia), swelling, and pain in the glands, which can affect their ability to eat and speak comfortably. In some cases, salivary gland dysfunction can be long-lasting and may require ongoing treatment to manage symptoms.
Although iodine-131 is used to target thyroid cancer cells, it can also destroy healthy thyroid tissue, leading to hypothyroidism. Patients who develop hypothyroidism after iodine-131 therapy may require lifelong thyroid hormone replacement therapy to maintain normal metabolic function.
Lutetium-177
Lutetium-177 is frequently used in the treatment of neuroendocrine tumours and prostate cancer. While generally well tolerated, it can cause certain specific side effects.
Fatigue and general malaise are common side effects of lutetium-177 therapy. Patients often report feeling unusually tired or weak during and after treatment. These symptoms can persist for several weeks, and supportive care, including rest and nutritional support, may be necessary to help patients recover.
As mentioned earlier, lutetium-177 can cause haematological toxicity, particularly in the form of bone marrow suppression. This effect may result in reduced blood cell counts and an increased risk of infections, bleeding, and anaemia.
Mitigating Adverse Effects
Pre-Treatment Assessment
One of the most important strategies for minimising the adverse effects of radionuclide therapy is conducting a thorough pre-treatment assessment. This includes evaluating the patient’s overall health, kidney function, and bone marrow reserves, as well as identifying any pre-existing conditions that may increase the risk of complications.
Protective Agents
The use of protective agents, such as amino acid infusions and antioxidants, can help reduce the radiation exposure to healthy tissues. These agents are often administered alongside radionuclide therapy to protect organs such as the kidneys and salivary glands.
Post-Treatment Monitoring
Regular post-treatment monitoring is crucial for detecting and managing adverse effects early. Blood tests, imaging studies, and clinical evaluations should be performed at regular intervals to assess the patient’s response to treatment and identify any emerging complications.
Conclusion
Radionuclide therapy is a powerful tool in the fight against cancer, offering a targeted approach that minimises the damage to surrounding healthy tissues. However, like any form of cancer treatment, it is not without its risks. Patients undergoing radionuclide therapy may experience a range of adverse effects, from mild and temporary symptoms like nausea and fatigue to more serious complications such as myelosuppression, renal toxicity, and the potential for secondary malignancies.
While many of these side effects can be managed with appropriate medical interventions, the risk of long-term complications underscores the importance of careful patient selection, pre-treatment assessment, and ongoing monitoring. By understanding the adverse effects associated with radionuclide therapy, healthcare professionals can better support their patients and ensure that the benefits of treatment outweigh the risks.
Disclaimer
The content presented in this article is intended for informational and educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. While efforts have been made to ensure the accuracy and reliability of the information provided, Open Medscience makes no representations or warranties regarding the completeness, accuracy, or applicability of the content to individual cases.
Radionuclide therapy and its associated adverse effects may vary significantly between patients, depending on individual health conditions, treatment protocols, and other clinical factors. Readers are strongly advised to consult a qualified healthcare professional before making any decisions related to medical treatment. Any reliance placed on the information provided in this article is strictly at the reader’s own risk.
Open Medscience, its authors, editors, and affiliates accept no responsibility or liability for any loss, harm, or damage resulting from the use or misuse of the information contained herein. This article does not constitute an endorsement of any specific medical treatment, therapy, or clinical practice.
You are here: home » diagnostic medical imaging blog »