Summary: The tumour grading system is essential in cancer diagnosis, treatment planning, and prognosis. It classifies tumours based on cellular characteristics observed under a microscope, giving insights into tumour aggressiveness and potential behaviour. This article explores the tumour grading system, its significance, grading criteria, and its impact on treatment strategies.
Keywords: Tumour grading; Cancer diagnosis; Treatment planning; Cellular characteristics; Molecular testing; Prognosis.
Introduction to the Tumour Grading System
Cancer remains one of the leading causes of morbidity and mortality worldwide, with varying types, behaviours, and treatment outcomes. One critical aspect of cancer evaluation is the tumour grading system, which provides a method for assessing the malignancy’s aggressiveness and potential growth rate. The grade of a tumour is distinct from its stage: while staging indicates the size and spread of the cancer, grading focuses on the microscopic appearance of cancer cells and how much they resemble normal cells.
Tumour grading plays a pivotal role in determining prognosis and guiding treatment decisions. By assessing cellular abnormalities, clinicians gain valuable insights into how quickly the tumour is likely to grow and spread, thus aiding in the development of an effective treatment plan tailored to each patient.
Significance of Tumour Grading in Cancer Diagnosis
Tumour grading is crucial for understanding the potential behaviour of cancer. It helps predict the tumour’s growth rate and its likelihood of spreading to other parts of the body. A higher-grade tumour generally signifies a more aggressive cancer that may spread more quickly. Conversely, a lower-grade tumour may indicate a slower-growing cancer that could be less likely to metastasise.
Grading also provides a framework for evaluating prognosis, as higher grades typically correlate with poorer outcomes. As such, the tumour grade is an important factor in deciding whether aggressive treatments, such as chemotherapy or radiotherapy, are necessary alongside surgery or other interventions.
Classification of Tumour Grades
Tumour grades are often classified into three or four primary categories based on their microscopic characteristics. While each cancer type may have specific grading criteria, the general classification typically includes the following:
- Grade 1 (Low grade): Cancer cells look more like normal cells, suggesting they are slow-growing and less likely to spread. Low-grade tumours often have a better prognosis and may not require aggressive treatment.
- Grade 2 (Intermediate grade): Cancer cells are moderately abnormal, indicating a slightly higher growth rate and an intermediate prognosis. These tumours may require more monitoring and treatment.
- Grade 3 (High grade): Cancer cells appear highly abnormal and bear little resemblance to normal cells, signifying a faster growth rate and increased likelihood of spread. High-grade tumours usually demand aggressive treatment approaches.
- Grade 4 (Very high grade): Some grading systems include a fourth grade, which signifies the most abnormal cells, indicating highly aggressive cancer with a poor prognosis.
Grading Criteria and Methods
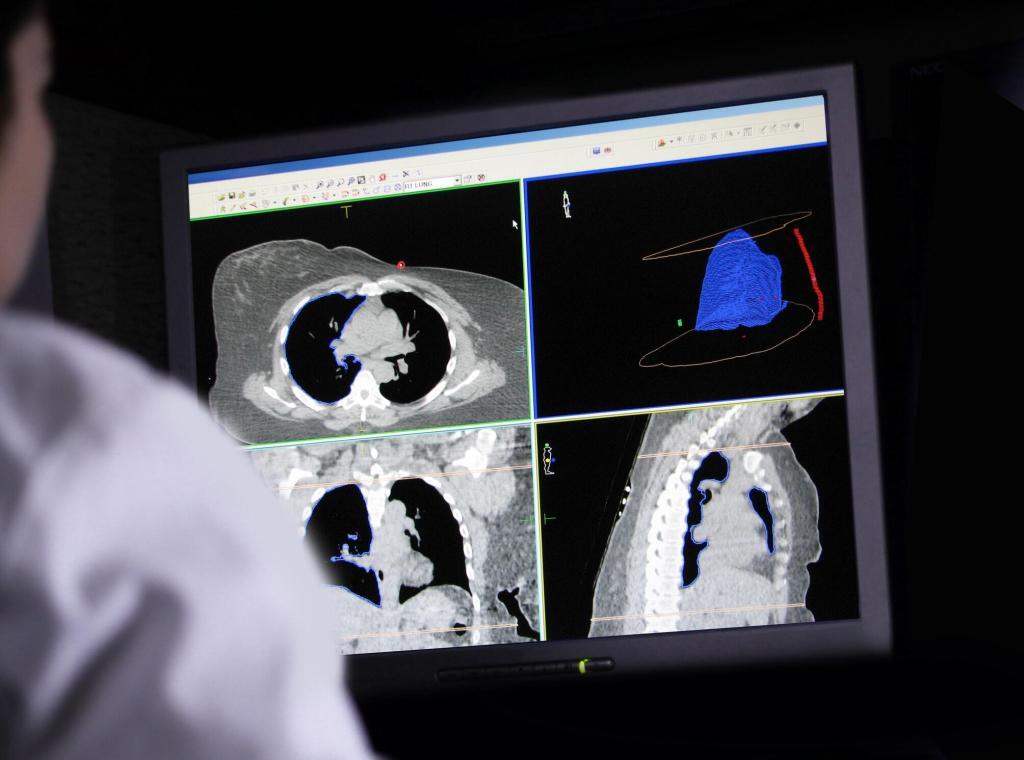
Different criteria are used to assess the grade of a tumour. Key factors include cell appearance, size, organisation, and mitotic rate (the rate at which cells divide). Pathologists examine tumour samples under a microscope to determine the grade based on these characteristics. Specific grading systems vary by cancer type, with notable examples including:
- Gleason Score for Prostate Cancer: The Gleason system assesses prostate cancer aggressiveness by scoring the two most predominant cell patterns from 1 to 5, with 5 being the most abnormal. The two scores are then added to provide a final grade (e.g., 3+4=7).
- Nottingham Grading System for Breast Cancer: This system evaluates breast cancer by examining tubule formation, nuclear grade, and mitotic count, assigning a score for each. The combined score determines the tumour grade from I to III.
- WHO Classification for CNS Tumours: The World Health Organisation (WHO) grades central nervous system (CNS) tumours from I to IV, with Grade I being least aggressive and Grade IV being the most aggressive.
By using these established grading systems, pathologists ensure a standardised approach to assessing different types of cancer, enabling a more accurate prediction of tumour behaviour and response to treatment.
Impact of Tumour Grade on Treatment Decisions
The tumour grade is a significant factor in determining the appropriate treatment approach. Low-grade tumours might be effectively managed with surgical removal alone, with minimal need for additional therapies. For example, in cases of Grade 1 breast cancer, surgery might be sufficient without the need for chemotherapy or radiation.
Intermediate-grade tumours may require a combination of surgery, radiation, and potentially chemotherapy to control the cancer’s spread. For example, Grade 2 prostate cancers often benefit from localised treatments but may also need hormonal therapy.
High-grade tumours are usually aggressive and require an intensive treatment approach, including surgery, chemotherapy, radiation, and targeted therapies. Grade 3 or 4 brain tumours, for example, often necessitate an aggressive multi-modal treatment plan to prolong survival.
Thus, the tumour grade enables oncologists to personalise cancer treatment, selecting therapies that match the tumour’s anticipated behaviour and potential growth rate.
The Role of Molecular and Genetic Testing in Tumour Grading
While traditional grading relies on cell morphology, molecular and genetic testing is becoming increasingly important in cancer diagnostics. Certain genetic mutations and biomarkers can influence tumour behaviour, even within the same grade. For instance, breast cancers with HER2-positive status or BRCA mutations may behave more aggressively, requiring targeted therapies even if the tumour grade is low.
These molecular characteristics help refine treatment approaches, often leading to more precise and effective interventions. Tumour grading, coupled with genetic insights, enhances the accuracy of prognosis and enables truly personalised cancer care.
Challenges and Limitations of the Tumour Grading System
The tumour grading system, while essential, has certain limitations. One major challenge is inter-observer variability, as grading is subjective and relies on a pathologist’s interpretation. Different pathologists might assign different grades to the same tumour, potentially impacting treatment decisions.
Moreover, tumour grades do not always predict patient outcomes accurately. Some high-grade tumours may respond well to treatment, while low-grade tumours may behave more aggressively than anticipated. This variability highlights the importance of integrating other diagnostic factors, such as staging and molecular profiling, to create a comprehensive picture of cancer behaviour.
The Future of Tumour Grading: Towards a More Integrated Approach
As cancer research advances, there is a growing focus on integrating tumour grading with molecular and genetic information. This approach, known as “integrated diagnostics,” combines traditional grading with insights from genetic testing, biomarker analysis, and other advanced techniques. The aim is to develop a more precise tumour classification system that captures the full complexity of cancer behaviour.
Machine learning and artificial intelligence (AI) are also being explored to improve the accuracy and consistency of tumour grading. AI-driven image analysis can help standardise the grading process, reducing subjectivity and ensuring uniformity in tumour classification.
By combining traditional grading with cutting-edge technology, the future of cancer diagnostics looks promising. This integrated approach could lead to more accurate predictions of tumour behaviour, enabling oncologists to tailor treatments with greater precision.
Patient Implications: Understanding the Tumour Grade
For patients, understanding the tumour grade provides insight into the nature of their cancer and what to expect from treatment. Patients with low-grade tumours can often approach treatment with greater optimism, while those with high-grade tumours may prepare for a more aggressive treatment journey.
Clear communication about tumour grading is essential to help patients understand the significance of their diagnosis and the rationale behind treatment recommendations. As more information becomes available through molecular and genetic testing, patients are empowered with a more comprehensive understanding of their cancer, enabling informed decisions about their care.
Conclusion
The tumour grading system remains a cornerstone of cancer diagnosis and treatment planning. By categorising tumours based on cellular abnormalities, the grading system helps predict cancer aggressiveness and guides treatment decisions. While limitations exist, particularly regarding inter-observer variability, advancements in molecular testing and AI-driven diagnostics are poised to refine tumour classification and improve patient outcomes.
For healthcare providers and patients alike, understanding the tumour grade offers essential insights into the cancer’s behaviour, helping shape effective and personalised treatment strategies. As research progresses, an integrated approach to tumour grading promises a future where cancer care is increasingly precise, tailored, and effective in addressing the unique challenges of each patient’s journey.
Disclaimer
The content provided in this article is for informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Open Medscience does not offer medical services or personalised medical guidance. Readers should always consult with a qualified healthcare professional regarding any questions or concerns they may have about their health or a medical condition. While efforts have been made to ensure the accuracy and currency of the information presented, Open Medscience makes no guarantees and accepts no responsibility for any errors, omissions, or outcomes resulting from the use of this content. Any reliance placed on the information is strictly at the reader’s own risk.