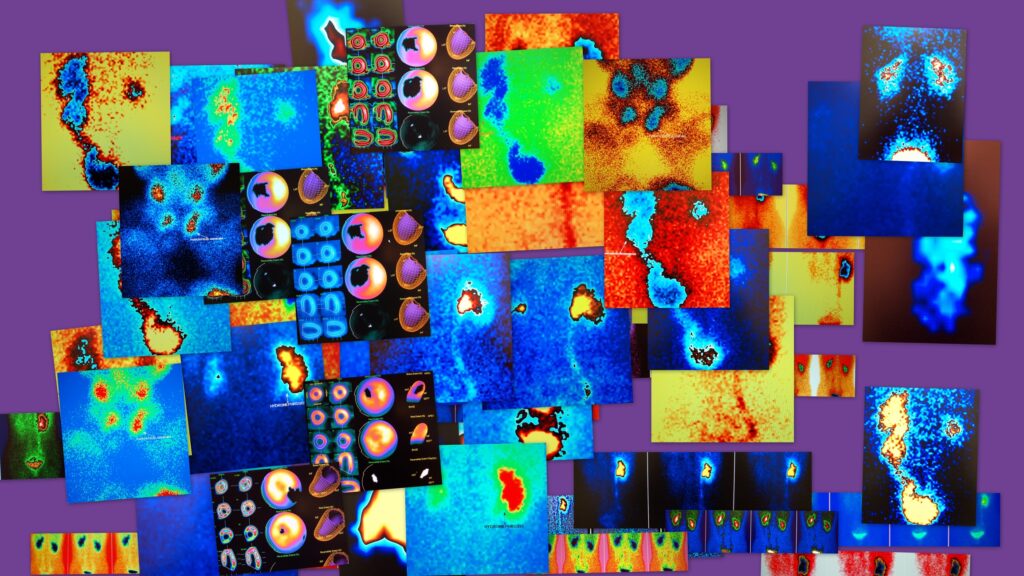
Summary: Medical imaging is an indispensable tool in modern healthcare, offering a window into the human body that aids in the diagnosis, monitoring, and treatment of countless diseases. Image classification, a subset of machine learning, is transforming this field by enabling faster, more accurate interpretation of medical images. This article examines the principles of AI imaging classification, explores the key methodologies, discusses clinical applications, and addresses the challenges and future directions in this rapidly evolving discipline
Introduction to Image Classification in Medicine
Medical imaging has revolutionised the way clinicians diagnose and treat diseases. Traditionally, the interpretation of medical images relied on expert radiologists who manually reviewed scans such as X-rays, MRIs, and CTs. The advent of machine learning (ML) and artificial intelligence (AI) has shifted the paradigm, introducing automated and semi-automated methods to classify and interpret these images.
AI image classification is a subset of computer vision that involves labelling images into predefined categories. In clinical practice, this means identifying abnormalities, detecting diseases, or monitoring changes in tissue over time. By automating these processes, image classification can reduce human error, speed up diagnoses, and expand access to expert-level analysis in under-resourced settings.
Key Principles of Image Classification
Image Preprocessing
Image preprocessing ensures the input data is clean and standardised. Steps include:
- Noise Reduction: Removing artefacts and irrelevant information from medical images.
- Normalisation: Adjusting intensity values to ensure uniformity across images.
- Segmentation: Identifying and isolating regions of interest (e.g., tumours or organs).
Feature Extraction
Feature extraction identifies key patterns or elements within an image. This step can involve:
- Texture Analysis: Differentiating tissues based on their textural properties.
- Shape Recognition: Detecting structural anomalies such as tumours.
- Edge Detection: Highlighting boundaries between different tissues.
Classification Algorithms
The core of image classification lies in the algorithms used. These can range from traditional statistical models to advanced neural networks.
Image Classification Methods
Traditional Machine Learning Approaches
Before the rise of deep learning, traditional ML techniques dominated:
- Support Vector Machines (SVMs): These models classify images by finding an optimal boundary that separates classes.
- K-Nearest Neighbour (KNN): A simple, non-parametric method that classifies based on proximity to labelled data points.
- Random Forests: Ensemble methods that combine multiple decision trees for robust predictions.
Deep Learning Models
Deep learning has revolutionised image classification, particularly in medical imaging:
- Convolutional Neural Networks (CNNs): CNNs are particularly suited to image data, using convolutional layers to detect spatial hierarchies in images. They are widely used in tasks such as tumour detection and organ segmentation.
- Recurrent Neural Networks (RNNs): Used in sequential data analysis, these are applicable in time-series imaging like dynamic MRIs.
- Transformers: Emerging models like Vision Transformers (ViTs) provide state-of-the-art results by capturing global relationships in images.
Hybrid Methods
Combining traditional ML with deep learning can leverage the strengths of both approaches. For instance:
- Feature extraction using classical methods followed by classification using CNNs.
- Integration of clinical metadata with image-based predictions for improved accuracy.
Clinical Applications of Image Classification
Disease Detection and Diagnosis
Image classification plays a pivotal role in diagnosing diseases:
- Cancer Detection: AI models can detect tumours in mammograms, CT scans, and MRIs with high precision.
- Cardiovascular Diseases: Automated tools classify abnormalities in echocardiograms, aiding in early detection of heart conditions.
- Neurological Disorders: Image classification supports the diagnosis of conditions like Alzheimer’s by identifying atrophy in brain scans.
Monitoring Disease Progression
Longitudinal studies require tracking changes in medical images over time. Image classification enables:
- Quantification of Tumour Growth: Measuring changes in tumour size and shape across scans.
- Evaluation of Treatment Response: Analysing how tissues respond to therapies such as chemotherapy or radiotherapy.
Surgical Planning and Guidance
Accurate image classification supports pre-surgical planning by:
- Identifying critical structures and pathologies.
- Providing 3D reconstructions for better visualisation.
Public Health and Screening Programmes
AI-driven classification can expand access to healthcare:
- Mass Screening: Analysing large datasets of images for diseases like tuberculosis or diabetic retinopathy.
- Outreach in Remote Areas: Cloud-based classification models enable diagnosis in under-resourced settings.
Challenges in Image Classification
Data Quality and Quantity
- Limited Datasets: High-quality, labelled medical datasets are scarce due to privacy concerns and the cost of annotation.
- Variability in Imaging Modalities: Differences in machine settings, imaging protocols, and patient anatomy introduce noise.
Interpretability and Explainability
Medical professionals require models to provide understandable outputs. Deep learning models, often criticised as “black boxes,” can hinder clinical adoption if their decisions cannot be explained.
Regulatory and Ethical Issues
- Bias in Training Data: Unequal representation of patient populations can lead to biased predictions.
- Data Privacy: Ensuring patient confidentiality while using and sharing medical images for training models is critical.
- Regulatory Approval: Medical AI systems must meet stringent regulatory standards, delaying deployment.
Integration into Clinical Workflows
Seamless integration of AI tools into clinical settings requires overcoming:
- Technical Barriers: Compatibility with existing hospital information systems.
- Human Factors: Gaining trust and acceptance from healthcare professionals.
Future Directions
Federated Learning
Federated learning enables model training across multiple institutions without sharing patient data. This approach can address data scarcity and privacy concerns.
Multimodal Analysis
Combining data from various sources, such as imaging, genomic, and clinical data, can enhance classification accuracy.
Real-Time Image Analysis
Advances in computational power will enable real-time classification, facilitating applications like intraoperative imaging and point-of-care diagnostics.
Personalised Medicine
AI models can identify patient-specific characteristics in medical images, paving the way for personalised treatment plans.
Democratisation of AI in Healthcare
Efforts to create open-source tools and datasets will expand the reach of image classification, particularly in low-resource settings.
Conclusion
Image classification is reshaping clinical diagnostics, offering the potential to improve accuracy, efficiency, and accessibility in healthcare. While challenges remain in data quality, explainability, and ethical considerations, ongoing advancements in technology and methodology promise a future where AI-driven image classification is a cornerstone of modern medicine.
This field stands as a testament to the transformative power of AI, bridging the gap between cutting-edge technology and compassionate patient care. With continued collaboration between technologists, clinicians, and policymakers, image classification is poised to redefine how we understand and treat human health.
Disclaimer
The content of this article, Transforming Healthcare: AI-Powered Medical Imaging Classification, is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment recommendations, and should not be used as a substitute for consultation with qualified healthcare professionals.
While every effort has been made to ensure the accuracy of the information presented, Open Medscience makes no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability of the content for any purpose. Any reliance you place on such information is therefore strictly at your own risk.
Discussions of artificial intelligence (AI) and machine learning (ML) technologies, including their applications in medical imaging, reflect the views and interpretations of the authors as of the publication date. These technologies are rapidly evolving, and the information may become outdated or superseded by future developments or regulations.
Open Medscience does not endorse any specific products, tools, algorithms, companies, or third-party services mentioned in the article. Inclusion of such references is for illustrative purposes only.
Readers are advised to consult regulatory guidelines and institutional policies relevant to the implementation and use of AI in clinical settings, and to seek expert advice before making any decisions based on the content herein.
You are here: home » diagnostic medical imaging blog »