Summary: Radiopharmaceutical therapy is revolutionising cancer treatment by combining targeted precision with potent radiation to eliminate tumours while minimising damage to healthy tissues. This article explores its principles, current applications, and the promising future of this transformative approach in oncology.
Introduction: A New Era in Cancer Therapy
Cancer treatment has long relied on surgery, chemotherapy, and radiotherapy. However, these methods often carry significant side effects, and their effectiveness may be limited in certain cancers. Radiopharmaceutical therapy (RPT) offers a paradigm shift—an innovative approach that uses radioactive compounds to selectively target and destroy cancer cells while sparing healthy tissue. With advances in molecular imaging and radiochemistry, RPT is rapidly gaining momentum as a cornerstone of modern oncology.
What is Radiopharmaceutical Therapy?
Radiopharmaceutical therapy in cancer involves the use of radioactive isotopes linked to molecules that specifically target cancer cells. These compounds are injected into the body, where they travel through the bloodstream to locate and bind to tumour cells. The radiation emitted by the isotopes kills the cancer cells by damaging their DNA or disrupting cellular processes.
Types of Radiation Used
RPT employs different types of radiation depending on the treatment goals:
- Alpha radiation: High-energy, short-range particles effective in destroying cancer cells while causing minimal damage to surrounding tissues.
- Beta radiation: Longer-range particles suitable for targeting larger or more diffuse tumours.
- Auger electrons: Extremely short-range particles ideal for targeting cancer at the cellular level when delivered directly to the nucleus.
Key Radiopharmaceuticals in Use
Several radiopharmaceuticals have gained regulatory approval and are transforming cancer care. Notable examples include:
Lutetium-177 (Lu-177) Dotatate
- Target: Neuroendocrine tumours
- Mechanism: Lu-177 emits beta radiation, effectively targeting and destroying cancer cells with minimal side effects.
- Clinical Impact: Demonstrates significant improvements in progression-free survival and quality of life for patients with advanced neuroendocrine cancers.
Radium-223 Dichloride (Ra-223)
- Target: Bone metastases from prostate cancer
- Mechanism: Alpha radiation selectively targets bone lesions while sparing healthy bone marrow.
- Clinical Impact: Reduces pain and improves survival in patients with metastatic castration-resistant prostate cancer.
Iodine-131 (I-131)
- Target: Thyroid cancer
- Mechanism: Beta radiation destroys residual thyroid tissue and metastatic cancer after thyroidectomy.
- Clinical Impact: Considered the gold standard for treating differentiated thyroid cancers.
Advantages of Radiopharmaceutical Therapy
Precision Targeting
RPT exploits the specificity of molecular targets, such as receptors or antigens, ensuring that radiation is delivered directly to cancer cells. This precision reduces off-target effects compared to traditional radiotherapy.
Minimal Side Effects
Because RPT spares healthy tissues, patients experience fewer side effects such as nausea, hair loss, and organ toxicity. This improves their overall quality of life during and after treatment.
Potential for Combination Therapies
Radiopharmaceuticals can be combined with other treatments, such as immunotherapy or chemotherapy, to enhance therapeutic outcomes. For example, Lu-177 has shown promise in combination with checkpoint inhibitors.
Treating Metastatic and Resistant Cancers
RPT is particularly effective in treating metastatic and chemotherapy-resistant cancers, offering hope to patients with limited treatment options.
The Role of Molecular Imaging in RPT
The success of RPT hinges on advanced imaging technologies that enable accurate tumour localisation and treatment monitoring. Positron emission tomography (PET) and single-photon emission computed tomography (SPECT) play vital roles in:
- Pre-treatment assessment: Identifying patients most likely to benefit from RPT.
- Dosimetry: Tailoring the radioactive dose to maximise efficacy while minimising toxicity.
- Monitoring: Tracking treatment response and disease progression.
Challenges in Radiopharmaceutical Therapy
Limited Availability
The production and distribution of radiopharmaceuticals are complex and require specialised facilities. This limits their availability in many regions.
High Costs
The development and delivery of RPT are expensive, often making it inaccessible to patients in low- and middle-income countries.
Regulatory Hurdles
Strict regulations surrounding the use of radioactive materials can slow down the approval and implementation of new therapies.
Safety Concerns
Handling and administering radioactive substances require stringent safety protocols to protect healthcare workers and patients.
Emerging Developments in RPT
Theranostics: A Dual Approach
Theranostics combines diagnostic imaging and therapy using the same radiopharmaceutical. For example, gallium-68 (Ga-68) is used for PET imaging, while Lu-177 delivers targeted therapy to the same molecular target. This personalised approach ensures precise treatment and real-time monitoring.
Novel Isotopes and Targets
Researchers are exploring new isotopes such as actinium-225 (Ac-225) and terbium-161 (Tb-161) for their unique radiation properties. Additionally, identifying novel molecular targets expands the scope of RPT to previously untreatable cancers.
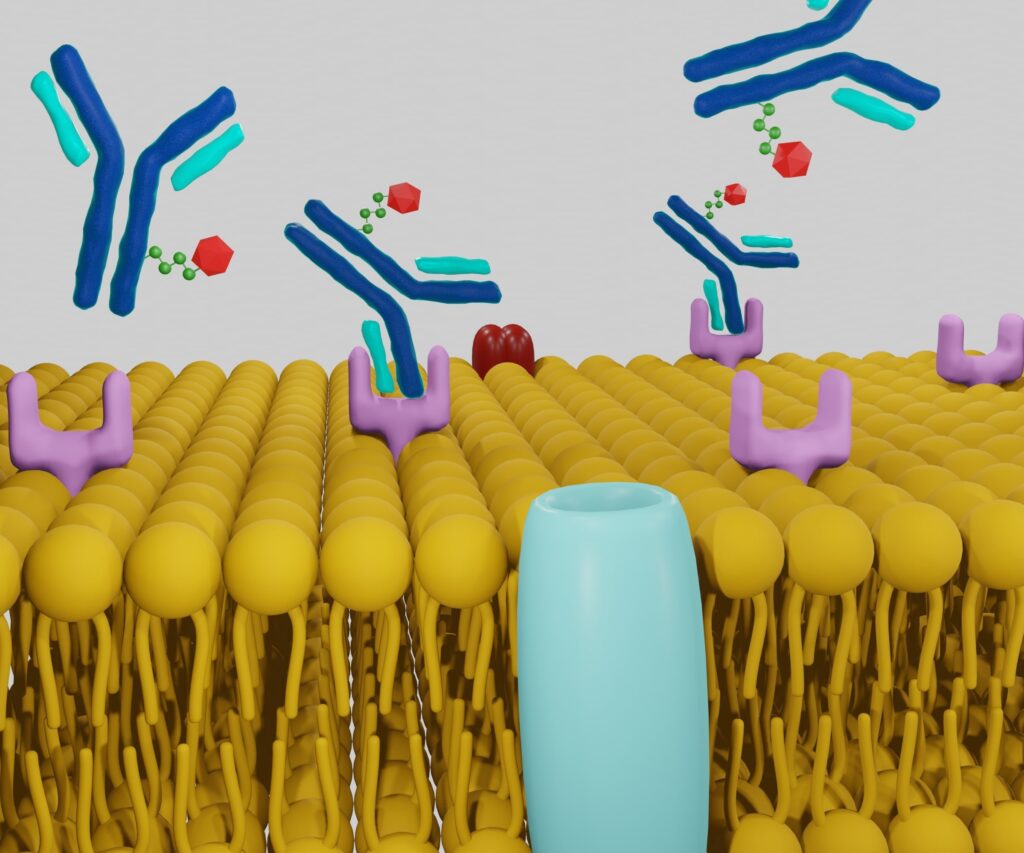
Immuno-Radiotherapy
Combining RPT with immunotherapy is an exciting frontier. Radiation can enhance immune responses by increasing tumour antigen presentation, creating a synergistic effect when paired with immune checkpoint inhibitors.
Artificial Intelligence in RPT
AI is being integrated into RPT for optimising dosimetry, predicting treatment responses, and developing new radiopharmaceuticals. This technology has the potential to revolutionise treatment planning and outcomes.
Clinical Success Stories
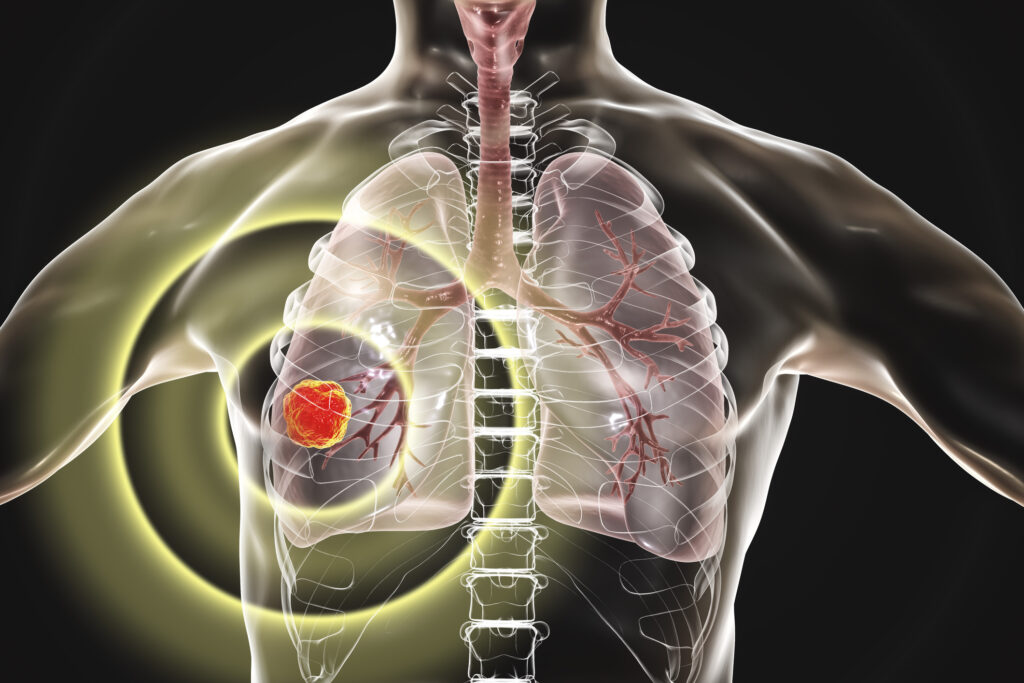
Prostate Cancer: Lu-177 PSMA Therapy
Lu-177 prostate-specific membrane antigen (PSMA) therapy has shown remarkable efficacy in metastatic prostate cancer. Clinical trials demonstrate significant reductions in tumour burden and prolonged survival, making it a game-changer for patients with advanced disease.
Neuroendocrine Tumours: PRRT
Peptide receptor radionuclide therapy (PRRT) using Lu-177 has transformed the management of neuroendocrine tumours. Patients experience improved quality of life, reduced symptoms, and extended survival times.
Paediatric Oncology: Novel Applications
Radiopharmaceuticals are being adapted for paediatric cancers, offering hope for children with aggressive or recurrent tumours. For instance, I-131 metaiodobenzylguanidine (MIBG) has shown promise in treating neuroblastoma.
The Future of Radiopharmaceutical Therapy in Cancer
The horizon for RPT is promising, with ongoing research poised to address current challenges and expand its applications. Key areas of focus include:
- Expanding Accessibility: Developing cost-effective production and distribution methods to make RPT widely available.
- Improving Safety: Innovations in shielding and administration techniques to enhance safety for healthcare workers.
- Personalised Medicine: Leveraging genomic and proteomic data to tailor treatments to individual patients.
- Public Awareness: Increasing education about RPT among patients and healthcare providers to promote its adoption.
Conclusion: A Revolution in Cancer Care
Radiopharmaceutical therapy is reshaping the landscape of oncology with its precision, efficacy, and potential for innovation. From treating rare neuroendocrine tumours to tackling metastatic prostate cancer, RPT offers new hope to millions worldwide. As research progresses and barriers are overcome, this cutting-edge therapy is set to become a cornerstone of cancer treatment for patients and healthcare professionals alike.
Disclaimer
The information provided in this article, “Radiopharmaceutical Therapy in Cancer: A Beacon of Hope in Oncology”, is intended for general informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Open Medscience does not endorse or recommend any specific treatment, therapy, or healthcare provider. Readers should always seek the advice of their physician or other qualified healthcare professional with any questions regarding a medical condition or treatment options.
While every effort has been made to ensure the accuracy of the content at the time of publication (23 November 2024), ongoing research and clinical developments may lead to changes in standards of care. Open Medscience assumes no responsibility or liability for any errors, omissions, or consequences arising from the use of the information provided.
You are here: home » diagnostic medical imaging blog »