Summary: Minimally invasive surgery techniques are reshaping the healthcare landscape, heralding a silent yet impactful revolution. With advancements in technology and medical practices, traditional open surgeries are being replaced by less invasive techniques that promise faster recovery, reduced pain, and fewer complications for patients. This article explores the transformative journey of minimally invasive procedures, with a focus on their application in cardiovascular care and stroke management, supported by innovative imaging and integrated systems.
Keywords: Minimally Invasive Surgery; Cardiovascular Interventions; Image-Guided Therapy; Stroke Care; Interventional Procedures; Healthcare Innovation.
The Transition to Minimally Invasive Surgery
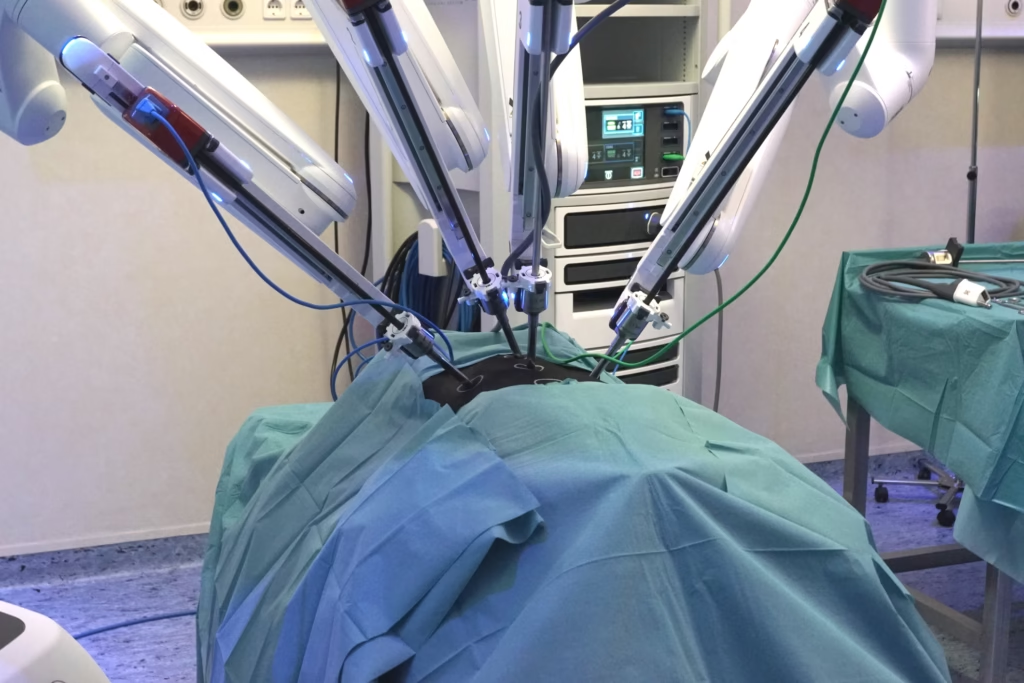
In the past decade, the medical field has witnessed an undeniable shift towards minimally invasive techniques. These procedures have fundamentally changed the way surgeons approach complex conditions, enabling them to operate with precision while minimising trauma to the body. From keyhole surgeries to catheter-based interventions, this transition has been driven by patient demand for faster recovery and healthcare systems’ focus on improving outcomes.
Benefits of Minimally Invasive Procedures
Minimally invasive surgeries offer numerous advantages over traditional methods, including:
- Reduced Recovery Time: Patients can return to daily activities sooner.
- Less Pain and Scarring: Smaller incisions translate to less discomfort and improved cosmetic outcomes.
- Lower Risk of Infection: With reduced exposure during procedures, the risk of postoperative complications is minimised.
- Cost-Effectiveness: Shorter hospital stays and quicker recoveries lower healthcare expenses.
Revolutionising Cardiovascular Care
One of the most significant impacts of minimally invasive surgery techniques is in the treatment of cardiovascular conditions. Interventional cardiology now uses techniques such as transcatheter aortic valve replacement (TAVR), coronary angioplasty, and atrial fibrillation ablation, reducing the need for open-heart surgeries.
The Role of Advanced Imaging in Cardiac Interventions
Cardiovascular procedures often rely on real-time imaging technologies to guide interventions. Modern systems integrate multiple imaging modalities, including:
- 2D X-Ray Fluoroscopy: Provides a live view of instruments and anatomy.
- 3D Ultrasound: Offers detailed images of soft tissues and blood flow.
- Intravascular Ultrasound (IVUS): Allows visualisation within blood vessels.
- Physiological Measurements (FFR/iFR): Assess blood flow and pressure in coronary arteries.
By merging these data streams, interventional cardiologists can perform highly precise procedures while maintaining situational awareness, ultimately improving patient outcomes.
The Integration Imperative
As the complexity of minimally invasive procedures grows, integrating systems, software, and devices becomes paramount. Hospitals are investing in comprehensive platforms that unify data from imaging tools, physiological monitors, and surgical instruments. This integration provides several benefits:
- Enhanced Control: Physicians can access all relevant information on a single interface.
- Improved Confidence: Seamless workflows allow surgeons to focus on critical tasks.
- Real-Time Decision-Making: Integrated systems enable dynamic adjustments during procedures.
Expanding Access to Life-Saving Stroke Care
Stroke remains one of the most devastating medical emergencies, with a global incidence rate of one every two seconds. Mechanical thrombectomy, a minimally invasive technique for removing blood clots, has emerged as a game-changer in stroke treatment. However, accessibility remains a critical issue.
Challenges in Stroke Management
- Limited Access: Less than 5% of the global population has access to mechanical thrombectomy.
- Lack of Training: Many healthcare professionals lack the expertise to perform advanced interventions.
- Infrastructural Gaps: Stroke-ready hospitals are sparse in many regions.
The Role of Innovation and Collaboration
Organisations like Philips and the World Stroke Organization are addressing these challenges by:
- Developing Mobile Stroke Units: Equipped with imaging tools and thrombolysis capabilities.
- Training Healthcare Professionals: Conducting workshops and certification programmes for interventional techniques.
- Improving Imaging Systems: Portable, high-resolution imaging devices that can be deployed in remote areas.
These efforts aim to expand access and improve stroke survival rates globally.
The Future of Minimally Invasive Surgery
The silent revolution in surgery is far from over. Emerging technologies such as robotics, artificial intelligence, and augmented reality are poised to further enhance minimally invasive techniques. In the future, we may see:
- Robot-Assisted Surgeries: Offering unmatched precision and consistency.
- AI-Driven Decision Support: Helping surgeons interpret complex data in real time.
- Virtual and Augmented Reality Training: Immersive platforms for skill development and procedure rehearsal.
Patient-Centred Care
As the field advances, the emphasis will remain on patient outcomes. Minimally invasive surgery aligns with the broader goals of personalised medicine by tailoring interventions to individual needs while reducing the physical and emotional toll on patients.
Conclusion
Minimally invasive procedures represent a silent but transformative revolution in surgery. By leveraging cutting-edge imaging, integrated systems, and innovative techniques, these advancements are reshaping the future of medical care. From cardiovascular interventions to stroke management, this approach is improving accessibility, outcomes, and quality of life for patients worldwide. As technology continues to evolve, the potential for minimally invasive surgery to redefine healthcare delivery is boundless.
Disclaimer
The content presented in this article is intended for informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare providers with any questions you may have regarding a medical condition or treatment options. The opinions and views expressed are those of the authors and do not necessarily reflect the official policy or position of Open Medscience. While every effort has been made to ensure the accuracy and reliability of the information provided, Open Medscience makes no guarantees and assumes no responsibility for errors or omissions. References to specific products, technologies, or companies are for illustrative purposes only and do not constitute endorsement or recommendation.