Cancer remains one of the world’s most formidable health challenges. It affects individuals across all demographics, profoundly impacting families, communities, and healthcare systems. The disease’s complexity and diversity make it a persistent adversary in global health. According to the World Health Organization, the global cancer burden is rising sharply, with over 35 million new cases annually projected by 2050, representing a 77% increase from 2022 estimates. This surge is attributed to factors such as population aging, growth, and increased exposure to risk factors like tobacco, alcohol, obesity, and environmental pollutants. Despite these daunting numbers, advances in diagnosis and prevention are offering new hope, saving millions of lives, and reshaping the future of cancer care.
How Can You Stay Updated with the Latest Oncology News?
To remain informed about the latest oncology news, consider trusted sources like OncoDaily, which is essential for healthcare professionals, researchers, and patients. OncoDaily is a platform that provides timely updates, expert insights, and comprehensive coverage of cancer research and treatment breakthroughs. By regularly consulting such resources, individuals can ensure they are up-to-date with the advancements shaping the field of oncology.
How Are AI and Machine Learning Changing Cancer Detection?
AI and machine learning are transforming cancer detection by enabling highly accurate image analysis, using deep learning to classify tumors, applying natural language processing to identify missed diagnoses in medical texts, and leveraging predictive risk models to detect early signs of cancer based on patient data.
- AI-powered imaging analysis: Now detects tumors in mammograms with up to 94.5% accuracy, enhancing radiologists’ ability to identify malignancies.
- Deep learning algorithms: Are used to classify skin lesions, with some models matching or outperforming dermatologists in melanoma identification.
- Natural language processing: Is being deployed in radiology reports to flag missed diagnoses across hospital systems.
- Predictive risk models: Built from electronic health records, allow earlier intervention based on subtle symptom patterns or biomarker shifts.
A key example is the NHS’s Cancer 360 system, which unifies patient data to speed up urgent case identification and helped Chelsea and Westminster Hospital meet the 28-day diagnosis target. Similarly, Imidex and Spesana are improving early lung cancer detection by combining an FDA-cleared AI algorithm with a medical data platform, enhancing nodule identification in chest X-rays.
These innovations highlight how AI software is streamlining diagnostics and improving outcomes.
What Are the New Blood Tests for Early Cancer Detection?
New blood tests like liquid biopsies and MCED can detect cancer early from a single blood sample. These tests analyze tumor-derived materials such as circulating tumor DNA (ctDNA), offering a non-invasive way to identify cancers at an earlier, more treatable stage.
Liquid biopsies detect cancer in blood
Liquid biopsies analyze ctDNA, RNA, and other tumor fragments circulating in the bloodstream, enabling early, non-invasive cancer detection. They are especially useful for patients unable to undergo surgical biopsies.
MCED tests identify multiple cancers
Multi-cancer early detection (MCED) tests, such as Galleri by GRAIL, can detect over 50 cancer types from a single blood draw. This allows for the identification of cancer even before clinical symptoms appear.
One notable example is PAC-MANN, developed by Oregon Health & Science University. This test identifies early-stage pancreatic cancer with 85% accuracy by measuring protease activity in the blood. It requires only a small sample and takes just 45 minutes to process, making it a cost-effective and scalable solution for population-level screening.
Can Genomic Profiling Improve Cancer Prevention?
Genomic profiling can improve cancer prevention by identifying inherited risk through polygenic scores and germline mutations, guiding early intervention, and personalized surveillance strategies.
- Polygenic risk scores (PRS): Aggregate thousands of common genetic variants to stratify cancer susceptibility. For instance, individuals in the top PRS quantile for breast cancer face a threefold increased risk.
- Germline mutation testing: For BRCA1/2 or Lynch syndrome genes, guides decisions on prophylactic surgery or intensive surveillance.
- All of Us Research Program (NIH): Aim to link genomic risk with lifestyle data to create tailored prevention protocols.
A prominent example is the Genomics England 100,000 Genomes Project, which demonstrated that a proportion of cancer patients carried actionable inherited mutations, leading to changes in their treatment and prevention strategies. This large-scale initiative highlighted the practical value of genomic profiling in cancer care.
What Are the Latest Advances in Cancer Biomarkers?
Recent advances in cancer biomarkers include circulating tumor cells, breath-based VOC detection, and urine tests using DNA or microRNAs, expanding beyond traditional protein markers like PSA and CA-125.
- Protein-based biomarkers: Such as PSA (for prostate cancer) and CA-125 (for ovarian cancer) remain in use but have limitations in specificity.
- Circulating tumor cells (CTCs): Provide real-time information on tumor activity and are being evaluated for use in lung and colorectal cancer.
- Volatile organic compounds (VOCs): Detected in exhaled breath, these are currently undergoing clinical trials for lung, oesophageal, and gastric cancers.
- Urine-based tests: Used for bladder and prostate cancer, these tests leverage methylated DNA fragments or microRNAs for early detection.
According to the National Cancer Institute (NCI), biomarker-driven diagnostics are essential for shifting from broad, population-level screening to more individualized and precise cancer detection strategies. By identifying biological markers specific to certain cancer types or patient profiles, clinicians can detect malignancies earlier, tailor screening intervals, and reduce overdiagnosis. This is especially important in cancers like lung, colorectal, and breast, where molecular heterogeneity impacts treatment outcomes.
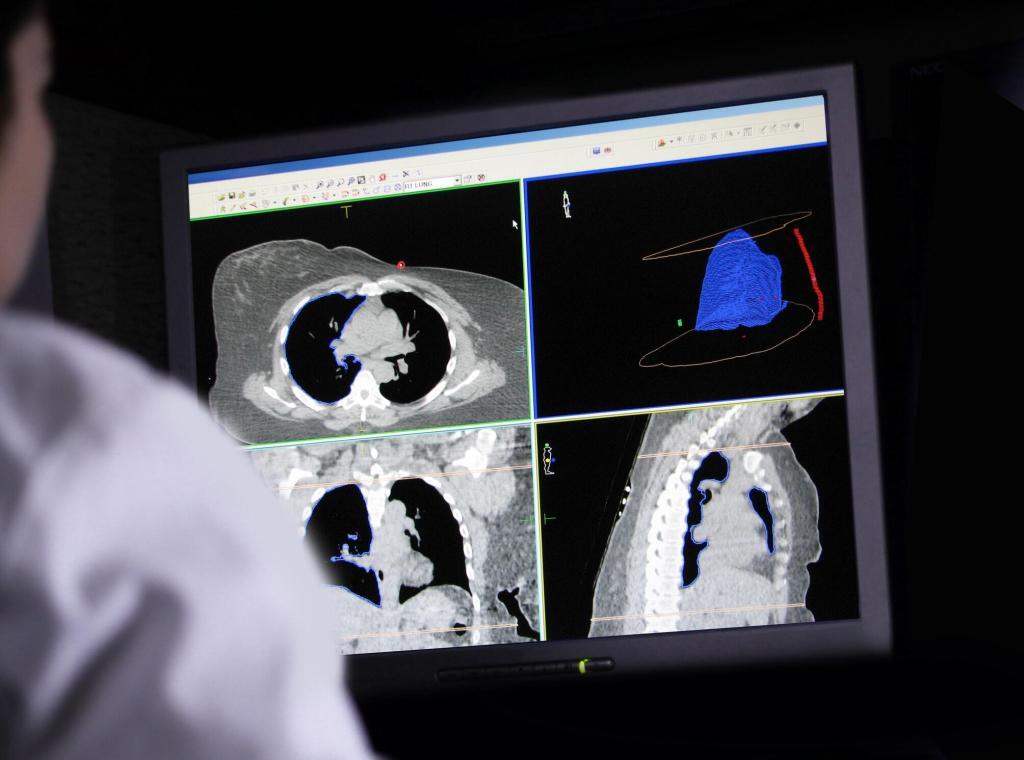
What Are the Latest Imaging Innovations in Early Cancer Detection?
Recent imaging innovations like LDCT, 3D mammography, advanced MRI, and fluorescence-guided surgery improve early cancer detection, reduce mortality, and support precise, tissue-sparing treatment.
LDCT reduces lung cancer mortality
Low-dose computed tomography (LDCT) for lung cancer screening reduces mortality by 20% among heavy smokers, according to the National Lung Screening Trial. It enables the detection of small, asymptomatic tumors before they progress.
3D mammography improves breast cancer detection
Digital breast tomosynthesis (3D mammography) enhances the detection of invasive breast cancers and lowers false positives by 15% compared to standard 2D mammography.
It offers clearer imaging of dense breast tissue.
MRI advancements aid early tumor localization
MRI techniques like diffusion-weighted imaging improve the early localization of tumors, particularly in the prostate and brain, where precision is critical. This helps guide treatment planning and biopsy targeting.
Intraoperative imaging supports complete tumor removal
Fluorescence-guided surgery and other intraoperative imaging tools help surgeons fully resect tumors while preserving surrounding healthy tissue. They increase the chances of achieving clean surgical margins.
AI overlays are now integrated into imaging hardware, helping radiologists identify subtle malignancies in real time with increasing reliability.
What Are Cancer Vaccines for Prevention?
Cancer vaccines for prevention aim to reduce cancer risk by targeting infections or tumor-specific antigens, with proven success in HPV and hepatitis B vaccines, and ongoing trials for personalized mRNA and Lynch syndrome–targeted vaccines.
- HPV vaccination: Proven to prevent over 90% of cervical cancer cases, according to WHO data (2023).
- Hepatitis B vaccines: Significantly reduce liver cancer incidence in high-risk regions such as East Asia and Sub-Saharan Africa.
- Personalized mRNA vaccines: Targeting patient-specific tumor neoantigens, these are currently in clinical trials for melanoma, pancreatic, and lung cancers.
- Preventive cancer vaccines for high-risk populations: Trials are underway for individuals with Lynch syndrome, including the Tri-Ad5 vaccine.
How Are Wearables and Digital Tools Used in Cancer Screening?
Wearables, symptom-tracking apps, and digital twins enable early cancer detection by passively monitoring health changes, logging symptoms, and modeling individual risk.
Smartwatches and biosensors track subtle health changes
Smartwatches and biosensors monitor heart rate variability, sleep, and physical activity—metrics that may shift subtly in the presence of early disease. These tools passively collect data, offering continuous, low-effort monitoring.
Symptom-tracking apps support proactive monitoring
Apps allow high-risk individuals to log symptoms like pain, bleeding, or fatigue and receive automated alerts to prompt diagnostic follow-up. They empower users to detect patterns that might otherwise be missed.
Digital twins personalize cancer risk assessment
AI-driven digital twins simulate individual health profiles to project cancer risk trajectories and tailor screening strategies. They combine genetic, clinical, and lifestyle data to improve precision.
A notable example is the Breast Cancer Weight Loss (BWEL) study by Dana-Farber, where Fitbit devices were used to monitor physical activity and fatigue patterns in breast cancer patients, demonstrating the potential of wearables in real-time symptom tracking.
This demonstrates how continuous biometric monitoring could be adapted for early cancer detection, especially for high-risk individuals who may not show immediate clinical signs.
What’s the Role of Environment-Based Models in Cancer Prevention?
Tools like Exposome databases, AI modeling, and wearable trackers help link environmental exposures to cancer risk and enable personalized prevention strategies.
- Exposome databases: Track environmental exposures such as air pollution, UV radiation, and endocrine-disrupting chemicals, linking them to cancer registries for long-term risk analysis.
- AI-based modeling tools: Platforms like Google’s DeepMind are used to model gene-environment interactions, helping to predict cancer development across large population cohorts.
- Personalized exposure assessments: Use tools like wearable pollutant trackers to monitor individual exposure levels and support tailored cancer risk reduction strategies.
These tools highlight modifiable risk factors and support prevention interventions tailored to local environments and individual susceptibility.
What Are the Global Disparities and Equity Challenges in Early Cancer Diagnosis?
Early cancer diagnosis in low- and middle-income countries is hindered by limited screening access, weak healthcare infrastructure, socioeconomic barriers, and lack of supportive policies.
Access to Screening and Diagnostic Services
In many LMICs, there is limited access to essential screening programs and diagnostic tools. This lack often results in cancers being diagnosed at more advanced stages, reducing the chances of successful treatment.
Healthcare Infrastructure and Resources
LMICs frequently face shortages of trained healthcare professionals, inadequate medical facilities, and limited availability of essential medicines and technologies. These challenges hinder timely and accurate cancer diagnoses.
Socioeconomic and Cultural Barriers
Factors such as poverty, low health literacy, cultural beliefs, and stigma associated with cancer can deter individuals from seeking early medical attention. Additionally, gender inequalities may prevent women from accessing necessary healthcare services.
Policy and Funding Limitations
Insufficient governmental policies and funding dedicated to cancer prevention and early detection exacerbate these disparities. Without robust national cancer control programs, many LMICs struggle to implement effective screening and diagnostic initiatives.
Example: Over 94% of cervical cancer deaths occur in LMICs due to limited HPV screening and vaccination (WHO).
For instance, Rwanda has implemented a nationwide HPV vaccination program, significantly reducing the incidence of cervical cancer among young women.
Conclusion
Advances in cancer diagnosis and prevention, such as AI, liquid biopsies, genomic profiling, vaccines, and wearables, are revolutionizing early detection and personalized care. These innovations facilitate earlier identification of cancer and inform targeted prevention strategies. However, implementing these solutions globally requires political commitment, adequate funding, and comprehensive education of healthcare providers to bridge existing disparities.
Disclaimer
The content provided in Top Breakthroughs in Cancer Diagnosis and Prevention is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment and should not be relied upon as a substitute for professional medical guidance. Readers are encouraged to consult qualified healthcare providers regarding any questions about their health, medical conditions, or treatment options.
While every effort has been made to ensure the accuracy and currency of the information presented, Open Medscience makes no representations or warranties, express or implied, about the completeness, reliability, or suitability of the content. Developments in medical research may cause some information to become outdated over time.
References to specific technologies, tests, or companies are for illustrative purposes and do not imply endorsement by Open Medscience. External links and cited sources are provided for convenience and do not constitute approval of their content or views.
Open Medscience disclaims all liability for any loss, injury, or damage arising from the use of or reliance on the information provided in this article.
You are here: home » diagnostic medical imaging blog »